You must be signed in to read the rest of this article.
Registration on AEGIS Dental Network is free. Sign up today!
Forgot your password? Click Here!
Conservation of Tooth Structure Utilizing Bonded Hybrid Ceramics
Chad C. Duplantis, DDS
ABSTRACT
Not surprisingly, dentistry has changed drastically over the past several decades. Much like their colleagues in medicine, dental professionals have developed a more engaged approach to overall health in addition to dental health. In support of the overall health of the patient, clinicians must account for the preservation of tissue. This trend has caused many practitioners to be increasingly cognizant of minimally invasive dentistry throughout their diagnostic, treatment, and preventative procedures. Technology has played a key role in the provision of this conservative approach to dentistry. Focusing on a minimally invasive approach to indirect dentistry, this article examines a post-diagnostic protocol that emphasizes CAD/CAM technology and advancements in materials. The merging of these two elements of dentistry allows the clinician to create lifelike restorations in an efficient and predictable manner.
Upon diagnostic assessment of a tooth, clinicians are faced with many options regarding the ultimate treatment decision. Several factors must be assessed regarding the tooth and the functional and esthetic needs of the patient in order to make a sound decision. Once the type of restoration is determined, the clinician must decide whether the restoration is to be direct or indirect and what material to use. With many restorative material options available, this decision process can be arduous, especially for a young, relatively inexperienced clinician.
Chairside indirect dentistry (ie, CAD/CAM) affords clinicians numerous choices to treat patients efficiently and effectively. The first chairside indirect restoration was placed in 1985 by Dr. Werner H. Mörmann in Zurich, Switzerland.1 The CAD/CAM industry has grown exponentially since its introduction to the dental marketplace. The ever-growing adoption of CAD/CAM has been fueled by various manufacturers creating advancements in both the technology used to acquire and design restorations and the materials used. Currently, multiple CAD/CAM materials, including hybrid ceramics, are available to create these restorations.
In addition to full-coverage restorations, partial-coverage restorations can be fabricated utilizing CAD/CAM technology. Advancements in adhesives also have made partial-coverage restorations a reality. These restorations conserve tooth structure and are long-lasting, functional, and esthetic. A partial-coverage restoration can either be fully contained within the confines of the tooth as an inlay or provide coverage of one or more cusps as an onlay. This article will examine the onlay as a viable restoration for clinical dentistry using hybrid ceramics.
The Onlay
Upon proper assessment of a tooth for a restoration, several factors must be considered regardless of whether the restoration will be new or a replacement of an existing restoration. The type of restoration is dependent on the size of the cavity created either by decay, removal of the existing restoration, or a combination of the two. After the assessment, a conservative cavity preparation could enable a direct restoration, which may be restored with amalgam, composite resin, or another material of choice. In some instances, a conservative restoration may be treated with an inlay. A larger cavity preparation may require cuspal coverage, thereby necessitating an indirect restoration such as a crown or onlay. While an onlay typically would be less invasive than a crown, the use of such a restoration is not always possible. Extensive occlusal or circumferential destruction of the tooth due either to decay or a previous restoration may prohibit treatment of the tooth with a partial-coverage restoration.
Veneziani has provided an encompassing definition of an onlay restoration, describing it as a "partial crown restoration made in composite or full ceramic, which has to be seated passively, and adhesively cemented in a cavity characterized by specific attributes." Furthermore, he offers two indications for the onlay restoration: (1) a wide Class II cavity with cusp coverage (one or more), and (2) restoration of a large occlusal surface compromised by wear and/or biocorrosion."2
Progression of Materials for Cuspal Coverage
Amalgam
Dating back to 1826, amalgam has been the most widely used material in dentistry.3 Through numerous compositional changes, amalgam has withstood the test of time; however, more recently its usage has dwindled. In 2010, a study found that the usage of composite resin restorations outnumbered amalgam restorations by 2 to 1. Several factors have contributed to the decrease of amalgam usage, including patients' fears over mercury toxicity, corrosion, esthetics, and the quest for a more conservative and bonded restoration.4 To this day, there are numerous amalgam restorations that have performed quite well over time. Skilled clinicians could even place an alloy with pins and/or amalgam bonding agents that can replace a cusp successfully. Although this material has demonstrated clinical success, many clinicians and patients are opting for newer and more esthetic materials.4
Composite Resins
Composite resins have been used successfully in dentistry for a number of decades. They have been used effectively in both small and large restorations due to positive developments in polymerization shrinkage and coefficient of thermal expansion. Manufacturers have also altered filler content and percentages to increase load-bearing capabilities. However, composite resins require careful placement and can be tedious to work with for clinicians. This is especially true for cuspal coverage. In a study evaluating 25 teeth that required cuspal coverage, no teeth had reported sensitivity at 2 weeks or at 30-month intervals postoperatively.5 This demonstrates the capability to cover cusps with minimal sensitivity, which has been reported as a problem by clinicians. Additional studies validate these restorations as a viable alternative to indirect restorations.6 Although direct composite resin has proven to be successful, many clinicians consider the placement of indirect restorations to be more efficient and predictable, especially using CAD/CAM technology, which has made the use of newer hybrid CAD/CAM blocks more appealing to clinicians.
Gold
Gold has proven its worth in dentistry for many years. Cast gold is durable and strong, and yet gold does not adversely wear the opposing dentition. In contrast to amalgam, gold does not corrode either. Gold is a desirable option for indirect dentistry, as gold onlays are beautiful. Cast gold survival rates have been documented as high as 97% for 10 years, and 94.1% at 10 years for partial-coverage restorations.7
Although gold has demonstrated considerable success, esthetics and cost minimize its use in modern-day dentistry. Gold has become so expensive that it is hard to justify the cost for a dental restoration with so many other available options Today, patients are increasingly looking to remove metal from their dentition and use a more esthetic alternative. Finally, many other materials offer the advantage of enabling an indirect restoration on the same day with CAD/CAM technology. Gold, however, is still a viable option if a patient is not averse to its esthetics.
Ceramics
Ceramics have a lengthy history in dentistry as both a veneering substrate and monolithic substrate for indirect restorations. The first documented ceramic inlay utilizing a CAD/CAM system, which as noted earlier was placed by Dr. Mörmann in 1985, was fabricated using a feldspathic porcelain (VITA Mark I, VITA Zahnfabrik, vita-zahnfabrik.com).1 The initial version of this material demonstrated a 10-year success rate of greater than 90%.8 The manufacturer incorporated some changes in the material, and the latter version (VITA Mark II) was also used for many years with great success. The changes were aimed at improving polishability, decreasing wear, and increasing strength. Although strength was increased, the material was only 130 MPa and up to 160 MPa if glazed.9 The second generation achieved 10-year success rates of 85.7%. Despite the success, this was a relatively weak material, and ceramics tend to be brittle in nature. Fracture was the most common cause of the failure of the restoration.10 With this being said, preparation design must allow for appropriate material thickness.
Despite the extensive history of ceramics, some characteristics exist that may diminish the longevity of a dental restoration. This is especially true in partial-coverage restorations. Ceramics are inherently brittle11; this requires the clinician to account for appropriate material thickness. If glazed, ceramics tend to wear the opposing dentition somewhat compared to other indirect restorative materials.12 A polished ceramic surface demonstrates less wear to opposing dentition yet still demonstrates a capacity to wear.13 Additionally, some clinicians who incorporate CAD/CAM restorations into their practice may consider the firing time after milling as inefficient. These characteristics have led to the creation of newer materials that are more user-friendly.
Hybrid Dental Ceramics
The advancement of dentistry, especially CAD/CAM, depends largely on the development of technology and materials. To address the need for esthetics, comparability to the human dentition, and wear resistance to the opposing dentition, a new classification of materials has emerged. This new classification, which the authors refer to as "hybrid dental ceramic" restorative materials, embodies the favorable qualities of composites and ceramics. Several brands from various manufacturers are available, and these materials are each unique in composition. The commonality among them is that they have both ceramic and resin components, but their microstructure and degree of filler vary. These hybrid dental ceramics are less brittle compared to conventional dental ceramics, which reduces the risk for failure before and after fabrication. They also exhibit excellent marginal adaptation and can be repaired predictably with composite resin.14
The two main categories of hybrid dental ceramics are polymer-infiltrated ceramic network (PICN) materials and resins with dispersed fillers. VITA Enamic® (VITA Zahnfabrik) is an example of a PICN. Several materials, including Lava™ Ultimate (3M Oral Care, 3m.com), Grandio blocs (VOCO, vocoamerica.com), CAMouflage® NOW (Glidewell, glidewelldental.com), CERASMART® (GC America, gcamerica.com), and Shofu Block HC (Shofu, shofu.com), among others, are in the category of resins with dispersed fillers.15,16 These hybrid dental ceramics are described in the following paragraphs.
VITA Enamic- The first material to be introduced in this classification, VITA Enamic, as previously stated, is a PICN. The manufacturer states that the material combines the benefits of composites and ceramics to relay strength and elasticity and behave similarly to human dentin, and that the product's attributes decrease the potential for crack propagation and fracture.17 It is composed of 86% ceramic (75% volume, mainly silicon dioxide, and aluminum oxide) and 14% polymer (25% volume, urethane dimethacrylate [UDMA] and triethylene glycol dimethacrylate [TEGDMA]), and possesses a flexural strength of 150 MPa to 160 MPa. Indications include full-coverage indirect restorations, partial-coverage indirect restorations, and veneers. 17,18 While bonding of these materials will be discussed later, this particular material is unique in that it can be etched with 5% hydrofluoric acid for 60 seconds on the intaglio surface due to the unique ceramic (ie, PICN) composition.17,18
LAVA Ultimate- As VITA introduced Enamic, 3M was working on a product of its own that claimed to have "revolutionary nanoceramic technology." This was the first product in the resins with dispersed fillers category. The material boasted a shorter milling time in comparison to other CAD/CAM materials and also was said to have a shock-absorptive capability along with ease of finishing and polishing, while offering a 10-year manufacturer warranty.19 Due to its unique composition, the product was designed to behave like conventional ceramic or glass-ceramics. LAVA Ultimate is comprised of nanomer particles (silica of 20-nm diameter and zirconia of 4-nm to 11-nm diameter) and treated with a silane coupling agent. The result is 80% nanocluster particles with a 20% infiltrated resin (bisphenol A-glycidyl methacrylate [bis-GMA], UDMA, bisphenol A-glycidyl methacrylate ethoxylated [bis-EMA], TEGDMA) matrix.20 The composition is aimed at creating greater wear resistance than resin alone. Its flexural strength is around 200 MPa.19 After several years on the market, this material encountered some difficulties in the clinical setting, mostly concerning the debonding of full-coverage restorations. Upon realization of the extent of the issue, the manufacturer pulled the indication of this material for full-coverage restorations in June 2015. The material, however, is still indicated for inlays, onlays, and veneers.21
Grandio blocs- Introduced in 2017, these blocks are nanoceramic hybrid resins with dispersed fillers, similar to other comparable products. However, they are differentiated by having an increased filler content that is said to be the highest achievable filler content in this classification of materials. The block is 86% filled with nanoceramic hybrid fillers and 14% resin (UDMA and DMA).20,22 This amount of filler relates to a flexural strength of 333 MPa.23 In addition to excellent strength, these blocks have a tooth-like modulus of elasticity and thermal cycling, a relatively low water sorption, and a very high radiopacity (308%), as per ISO 4049.24 In addition, the hybrid composition allows for a decreased milling time, which leads to a more efficient workflow. Grandio blocs are also easily repaired intraorally and available in two sizes to accommodate various sized restorations and 11 shades with higher and lower translucency options; indications are crowns, inlays, onlays, veneers, and implant-supported crowns.22
CAMouflage NOW- This nanohybrid resin, released in 2018, is formulated to be a material that is easy to mill. Its compressive strength of approximately 190 MPa makes this product comparable in strength to its competitors. The material, according to the manufacturer, is comprised of approximately 78% glass-ceramic filler (barium glass and silica nanoparticles) and 22% resin (bis-GMA, ethoxylated bis-phenol A dimethacrylate [EBPADM], and TEGDMA). CAMouflage NOW is indicated for inlays, onlays, veneers, and full-coverage crowns.25
CERASMART- This nanoceramic block is designed with the intention of merging the desirable characteristics of ceramic and resin technology. The material is comprised of 71% silica and barium glass nanoparticles and 29% resin (bisphenole A ethoxylate dimethacrylate [bis-MEPP], UDMA, and DMA).21 With a flexural strength of 238 MPa, this material is designed for minimal preparation of anterior, posterior, and implant restorations. There are no contraindications to full- or partial-coverage restorations, according to the manufacturer.26
Shofu Block HC- Another member of the ever-growing classification of chairside CAD/CAM materials known as resins with dispersed fillers, Shofu Block HC is said to be a unique hybrid material with no contraindications for restorations.27The product is comprised of a 61% zirconium silicate embedded in a polymer matrix (UDMA and TEGDMA). Flexural strength is 191 MPa. It reportedly is easy to polish, friendly to opposing dentition, and mills quickly.27
In addition to the products presented, others exist that also may be classified as hybrid dental ceramics. Additionally, it is anticipated that many more materials will enter this classification in the coming years.
Onlay Preparation Design
When considering an onlay or partial-coverage restoration, the clinician must first assess the quality of the remaining tooth. If there is enough good tooth structure supragingivally, an onlay may be a viable option. After caries or previous restoration removal, the amount of destruction created often dictates the final design. Proper adhesive technique, which will be discussed later, allows the clinician to be conservative in preparation and create a divergent preparation to ensure proper seating.
As previously stated, ceramics have been used with great success for many years. A leading manufacturer of dental ceramics (Ivoclar Vivadent, ivoclarvivadent.com) has created guidelines that are appropriate for all-ceramic indirect restorations and, based on the author's experience, can be easily translated to hybrid ceramics. These guidelines are as follows28,29 (Minor modifications noted in parentheses may be incorporated, depending on the condition of the tooth, to help ensure success.):
• The preparation margins should not be located in the area of static or dynamic antagonist contacts.
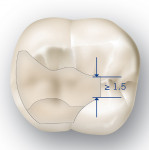
• The preparation depth must be at least 1.5 mm and the width of the isthmus must be at least 1 mm in the fissure area. (A width of 1.5 mm in the fissure area and at least 1 mm at the pulpal floor is the recommended modification [Figure 1].)
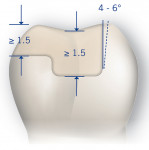
• The proximal box should be prepared with slightly diverging walls, and an angle of 100 to 120 degrees should be observed between the proximal cavity walls and the prospective proximal inlay surfaces. Marginal ridge contacts on the inlay should be avoided in case of pronounced convex cavity walls without adequate support by the proximal shoulder (4- to 6-degree diverging walls [Figure 2]).
• Internal edges should be rounded to prevent stress concentration within the ceramic material; slice cuts or feather edges should not be prepared.
• At least 1 mm of space should be allotted in the cusp areas for onlays. (To ensure allowance for adequate material thickness, 1.5 mm of space, if possible, is the recommended modification [Figure 2].)
Beyond these guidelines, all contacts should be on the tooth or substrate. In other words, care should be taken so that no contacts are on a margin of the restoration to avoid premature failure. If an undercut is present, it should be addressed with a flowable composite prior to impression. This added step will help ensure that the restoration seats passively upon cementation.
In addition to adhering to these guidelines for attaining a successful and long-lasting restoration, clinicians should follow the manufacturer's recommendations to account for appropriate material thickness, which may vary. Figure 1 and Figure 2 depict a recommended onlay design.
Bonding of Hybrid Ceramic Restorations
To properly bond these hybrid ceramic restorations in place, it is important to understand the chemical composition of these materials. Additionally, the two main categories of hybrid dental ceramics-PICN and resins with dispersed fillers-are handled differently pre-bonding. Although each material manufacturer may recommend a certain brand, each material can be bonded using a universal adhesive and an adhesive resin cement.
A significant difference exists between the bonding of PICN restorations and the bonding of restorations in the resins with dispersed fillers category for the post-milling/pre-bonding treatment of the intaglio surface. After the restorations, regardless of category, are milled, they should be cleaned with isopropyl alcohol to remove any lubricant that may have accumulated in the milling process. Due to the unique composition of ceramic in the PICN material, it is recommended that the intaglio surface be etched (5% hydrofluoric acid for 60 seconds).17,18 Many clinicians consider etching to be advantageous as it has been shown to increase bond strengths in ceramics.18 The bonding protocol, as per the manufacturer, is 37% phosphoric acid-etch for 30 seconds (enamel only, selective-etch) on the prepared tooth, followed by judicious application of the desired adhesive. After the appropriate etching of the restoration, a silane is added before adhesive is applied to the intaglio surface. The manufacturer's directions are not specific as to a suggested bonding agent or adhesive resin cement.18
For the hybrid ceramics in the resins with dispersed fillers category, the pretreatment of the intaglio surface excludes the etching step. While the composition of the PICN blocks is conducive to etching, the opposite is true for this other classification of materials. After the cleaning of the restoration with isopropyl alcohol post-milling, it is recommended to air-abrade the intaglio surface. Bonding protocols typically include air-abrading/sandblasting the intaglio surface of these restorations with a ≤50-µm particle at 30 psi until a matte finish is realized. Following air-abrasion, the restoration should again be cleaned with isopropyl alcohol and moisture-free air. Unlike the PICN, a silanating agent is not used for this category of hybrid ceramics. A universal adhesive is used on the intaglio surface and air-thinned. The tooth is treated in accordance with the manufacturer's instructions for the specific universal adhesive chosen. This may include self-etching, total-etching, or selective-etching. The tooth etchant is dependent on the clinician's preference. An adhesive resin cement is used to bond the restoration permanently. Adherence to these instructions should lead to clinical success and longevity of the restoration.21
Clinical Cases
Two clinical cases are presented to demonstrate the use of two different hybrid ceramic materials. The cases also illustrate two dissimilar indications for partial-coverage restorations.
Case 1
A 59-year-old male patient presented with a failing alloy restoration on tooth No. 3, along with spots of occlusal decay. Signs of leakage of the alloy, as well as fracture lines, seemed to place the distolingual cusp in jeopardy (Figure 3).
After anesthesia administration and onset, the existing alloy was removed. Prior to the removal of all the caries it was evident that the enamel on the distofacial cusp lacked support and the distolingual cusp was compromised (Figure 4). All active caries was removed, and the clinician then considered several treatment options. One was to place a direct alloy or composite resin restoration. Another option was a full-coverage restoration using an esthetic material such as lithium disilicate, zirconia, or a combination of the two. A third possibility, which the clinician ultimately selected, was for a partial-coverage onlay to repair the affected portion of the tooth. This decision was made based on predictability of the restoration, the necessity for cuspal coverage, and conservation of unaffected tooth structure. Hybrid ceramic would be the material of choice.
The preparation was refined by reducing the distofacial and distopalatal cusps (Figure 5). Grandio blocs was chosen for this clinical case. As previously mentioned, this material is 86% filled and possesses a 333 MPa flexural strength.20,22,23 Because this tooth was the last in occlusion, maximum strength was a key consideration in the material choice.
The restoration was designed and milled using a CEREC® Primescan intraoral scanner and CEREC® 5.1 software (Dentsply Sirona, dentsplysirona.com). The nanoceramic hybrid CAD/CAM block was size 12, shade A2 HT. Once the restoration design was completed it was sent to the mill (CEREC® MC XL, Dentsply Sirona); mill time was less than 6 minutes. The block was removed, the sprue was removed, and the restoration was cleaned with alcohol and water and polished in the laboratory with a Robinson bristle brush. The intaglio surface was then air-abraded with 30-µm corundum particles, modified by silica at 40 psi (CoJet™ Sand, 3M Oral Care) (Figure 6). Following verification of marginal adaptation and occlusal contacts, the restoration was seated utilizing the manufacturer's bonding protocol for Grandio blocs.
A bonding agent (Ceramic Bond, VOCO) was placed on the intaglio surface for 60 seconds and allowed to air-dry. The excess was removed with a gentle air stream so that no pooling occurred. For the tooth, the enamel was selectively etched with 37% phosphoric acid for 20 seconds. Although etching is an optional step, the author believes that research supports a selective-etch (enamel-only) technique.30 Following enamel etching, the preparation was cleaned with a desensitizer (Hemaseal & Cide™, Advantage Dental Products, Inc, advantagedentalinc.com), and adhesive (Futurabond U, VOCO) was applied to the tooth for 20 seconds and gently air-dried (Figure 7 and Figure 8). The adhesive was light-cured for 10 seconds on the surface of the tooth. A dual-curing universal composite-based luting material (Bifix QM, VOCO) was the cement of choice. It can be placed either on the intaglio surface of the crown or, as the author prefers, on the tooth prior to seating. Once the restoration was placed, it was tack-cured for 2 to 3 seconds. The excess was cleaned up, and the remainder was allowed to set fully for 4 minutes. The setting time for this dual-cure resin cement from insertion is 3 minutes (Figure 9 and Figure 10).31,32
After the setting of the cement, the restoration was polished. For polishing, the restoration was finished with a gold fluted carbide bur (NeoBurr® Esthetic Finishers, EF6, Microcopy, microcopydental.com) at the margins. The occlusal surface was adjusted using a fine diamond football bur (NeoDiamond® Fine, Red, #368, Microcopy). The final polish was attained utilizing diamond-impregnated, flexible polishing spirals (A.S.A.P All Surface Access Polishers, Clinician's Choice, clinicianschoice.com) (Figure 11 and Figure 12).
Case 2
A 60-year-old man presented following orthodontic treatment. Although the orthodontics had produced an overall stable bite, the patient was concerned about a resultant occlusal discrepancy between teeth Nos. 28 and 29 and the opposing dentition. He inquired as to whether there was a conservative way to close the vertical space (Figure 13 and Figure 14).
During his examination, a rather large disto-occlusal alloy on tooth No. 29 and an occlusal composite on tooth No. 28 were noted. The clinician and patient discussed several treatment options, including two full-coverage restorations on teeth Nos. 28 and 29. Favoring a minimally invasive approach, it was decided to remove the alloy on tooth No. 29 and the composite on tooth No. 28 and fabricate onlays/overlays. The main goal was to close the vertical discrepancy.
The composite restoration on tooth No. 28 was removed, and the occlusal surface was prepared slightly to allow for proper bonding. The alloy and minimal amount of recurrent decay in tooth No. 29 were removed, and the occlusal surface was prepared minimally as well (Figure 15). The preparations were scanned using an intraoral scanner (iTero Element® 2, Align Technology, Inc, itero.com) and the onlays were designed utilizing fastdesign.io™ software (Glidewell). The restorations were then milled using the fastmill.io™ mill system (Glidewell) and CAMouflage NOW blocks, shade A2 HT (Glidewell). The restorations milled in less than 8 minutes each.
The final restorations were handled, for the most part, in the same manner as in Case 1, from removal from the mill to the insertion and cementation. The only difference was the treatment of the intaglio surface of the restorations. On this material, placement of a ceramic priming agent is not recommended. A universal adhesive (Futurabond U) was placed after air abrasion and before bonding with a dual-cure resin cement (Bifix QM). The restorations resolved the patient's chief complaint of excessive post-orthodontic occlusal discrepancies in an efficient and minimally invasive manner (Figure 16 and Figure 17).
Conclusion
CAD/CAM dentistry is progressing daily. Dentists are increasingly accepting and adopting the benefits that this technology affords the dental practice. The digital workflows and newer materials offer an efficient alternative to traditional laboratory-driven dentistry that satisfies the clinician and patient. The newer hybrid ceramic materials provide an indirect restoration alternative to direct materials and conventional ceramics for both experienced and inexperienced users. Clinicians must know the composition and benefits of the various hybrid dental ceramic materials and understand the diagnosis and treatment options. Clinicians may benefit from observing the experiences of others before deciding which is the best option for their practice. Bonding protocols are dependent on the composition of the restorative materials and vary from manufacturer to manufacturer, and of course, it is advised to follow the manufacturer's instructions. Following these principles can help ensure longevity for the restoration.
Disclosure
The author has received an honorarium from VOCO America Inc. for this article.
About the Author
Chad C. Duplantis, DDS
Private Practice, Fort Worth, Texas; Fellow, Academy of General Dentistry
References
1. Mörmann WH, Bindl A. All-ceramic, chair-side computer-aided design/computer-aided machining restorations. Dent Clin North Am. 2002;46(2):405-426.
2. Veneziani M. Posterior indirect adhesive restorations: updated indications and the morphology driven preparation technique. Int J Esthet Dent. 2017;12(2):204-230.
3. Bharti R, Wadhwani KK, Tikku AP, Chandra A. Dental amalgam: an update. J Conserv Dent. 2010;13(4):204-208.
4. Jackson R. Esthetic inlays and onlays. In: Freedman GA, ed. Contemporary Esthetic Dentistry. St. Louis, MO: Elsevier Mosby; 2012:469.
5. Deliperi S, Bardwell DN. Clinical evaluation of direct cuspal coverage with posterior composite resin restorations. J Esthet Restor Dent. 2006;18(5):256-267.
6. Manhart J. Cusp replacement with an extensive posterior direct restoration using a nanohybrid bulk-fill ormocer. International Dentistry - African Edition. 2015;9(3):6-16.
7. Bandlish LK, Mariatos G. Long-term survivals of ‘direct-wax' cast gold onlays: a retrospective study in a general dental practice. Br Dent J. 2009;207(3):111-115.
8. Otto T, De Nisco S. Computer-aided direct ceramic restorations: a 10-year prospective clinical study of Cerec CAD/CAM inlays and onlays. Int J Prosthodont. 2002;15(2):122-128.
9. Giordano R. Materials for chairside CAD/CAM-produced restorations. J Am Dent Assoc. 2006;137 suppl:14S-21S.
10. Zimmer S, Göhlich O, Rüttermann S, et al. Long-term survival of Cerec restorations: a 10-year study. Oper Dent. 2008;33(5):484-487.
11. Ansong R, Flinn B, Chung KH, et al. Fracture toughness of heat-pressed and layered ceramics. J Prosthet Dent. 2013;109(4):234-240.
12. Janyavula S, Lawson N, Cakir D, et al. The wear of polished and glazed zirconia against enamel. J Prosthet Dent. 2013;109(1):22-29.
13. Sethi S, Kakade D, Jambhekar S, Jain V. An in vitro investigation to compare the surface roughness of auto glazed, reglazed and chair side polished surfaces of Ivoclar and Vita feldspathic porcelain. J Indian Prosthodont Soc. 2013;13(4):478-485.
14. Alamoush RA, Silikas N, Salim NA, et al. Effect of the composition of CAD/CAM composite blocks on mechanical properties. Biomed Res Int. 2018;2018:4893143.
15. Yu H. Material selection for CAD/CAM dentistry: glass ceramic or hybrid materials? Dent Oral Craniofac Res. 5: DOI: 10.15761/DOCR.1000278.
16. Mainjot AK, Dupont NM, Oudkerk JC, et al. From artisanal to CAD-CAM blocks: state of the art of indirect composites. J Dent Res. 2016;95(5):487-495.
17. VITA ENAMIC - the first hybrid dental ceramic in the world [press release]. Bad Säckingen, Germany: VITA Zahnfabrik; September 24, 2012. https://www.vita-zahnfabrik.com/en/VITA-ENAMIC-the-first-hybrid-dental-ceramic-in-the-world-4682,57329.html. Accessed December 22, 2020.
18. VITA ENAMIC Technical and scientific documentation. Bad Säckingen, Germany: VITA Zahnfabrik; November 2013. https://s3-eu-west-1.amazonaws.com/core3d-website/content/pdfs/VITA-ENAMIC-Technical-Scientfic-Documentation.pdf. Accessed December 22, 2020.
19. Lava™ Ultimate CAD/CAM Restorative. Technical Product Profile. St. Paul, MN: 3M ESPE; 2011. . Accessed December 22, 2020.
20. Alamoush RA, Silikas N, Salim NA, et al. Effect of the composition of CAD/CAM composite blocks on mechanical properties. Biomed Res Int. 2018;2018:4893143.
21. Notice: Change in Indication - Lava™ Ultimate Restorative. St. Paul, MN: 3M Oral Care; June 12, 2015. https://multimedia.3m.com/mws/media/1198023O/lava-ultimate-restorative-change-of-indication-notice.pdf. Accessed December 22, 2020.
22. VOCO Grandio Blocs. Indian Land, SC: VOCO America Inc; 2017. https://cdn.vivarep.com/contrib/va/kol/queue/voco_finalgrandioblocsusbrochure.20180208185521509.pdf. Accessed December 22, 2020.
23. Lyu C, Spintzyk S, Oldenburger D, et al. Two-body wear behavior of nano-hybrid technology produced CAD/CAM composite-resin blocks. J Dent Res. 2017;96(spec iss A):1002.
24. Grandio Blocs, Grandio Disc Processing Instructions. Cuxhaven, Germany: VOCO GmbH; 2017. https://www.voco.dental/cn/portaldata/1/resources/products/folders/gb/grandio-blocs-disc-processing-instruction_fol_gb.pdf. Accessed December 22, 2020.
25. CAMouflage NOW Technical Brochure. Irvine, CA: Glidewell Dental; 2019.
26. Ceramic and CAD/CAM: Shofu Block and Disk HC. San Marcos, CA: Shofu Dental Corp; 2018.
27. New Material for CAD/CAM-based Restorative Dentistry. Inside Dentistry eBooks. Shofu Dental Corp. September 2017. . Accessed December 22, 2020.
28. IPS e.max® Clinical Guide. Amherst, NY: Ivoclar Vivadent; 2011:11. https://www.ivoclarvivadent.com/zoolu-website/media/document/1269/IPS+e-max+Clinical+Guide. Accessed December 22, 2020.
29. All-Ceramic Chairside Preparation Guide for IPS Empress® and IPS e.max®. Amherst, NY: Ivoclar Vivadent; 2009. https://issuu.com/ivoclarvivadent/docs/all_ceramic_prep_guide. Accessed December 22, 2020.
30. Frankenberger R, Lohbauer U, Roggendorf MJ, et al. Selective enamel etching reconsidered: better than etch-and-rinse and self-etch? J Adhes Dent. 2008;10(5):339-344.
31. VOCO Futurabond U Instructions for use. Cuxhaven, Germany: VOCO GmbH; 2013. https://www.voco.dental/en/portaldata/1/resources/products/instructions-for-use/e1/futurabond-u_ifu_e1.pdf. Accessed December 22, 2020.
32. VOCO Bifix® QM Instructions for use. Cuxhaven, Germany: VOCO GmbH; 2017. https://www.voco.dental/en/portaldata/1/resources/products/instructions-for-use/e1/bifix-qm_ifu_e1.pdf. Accessed December 22, 2020.