You must be signed in to read the rest of this article.
Registration on AEGIS Dental Network is free. Sign up today!
Forgot your password? Click Here!
Novel Modifications to the Trephine Core/Osteotome Technique
An innovative alternative for implant site development
Anna M. Brunetti, DMD, MDS | Howard Drew, DMD | Andrew Sullivan, DDS | Joel Pascuzzi, DMD | Emil Cappetta, DMD
Inadequate bone height is often encountered in the posterior maxilla, complicating implant placement. The use of a combined trephine/osteotome technique has been introduced to increase bone height. This technique is less invasive than the lateral window and allows a relatively atraumatic implosion of autogenous bone displacing the floor of the sinus, increasing the amount of alveolar bone at the anticipated fixture site. The authors suggest novel modifications to make the technique more advantageous. Modifications include a two-stage procedure to place longer fixtures, use of the trephine and piezo tips when sinus floors are uneven, and multiple site sinus elevations. The following case presentations illustrate these novel modifications to maximize implant success in the posterior maxilla.
Sinus Augmentation Approaches
Common factors affecting implant success include the quantity and quality of bone, occlusal forces, and the anatomy of the maxillary posterior. Following tooth extraction, the rate of resorption is faster within the first 6 months, affecting the width and height of the ridge and compromising future implant placement.1 According to Lil and colleagues,2 the limiting factor for implant placement in this region is available bone height. According to previous studies, implant failures in the maxillary posterior region are attributed to type IV quality of bone.3-5
An absence of functional loading from tooth loss can result in severe bone resorption as the sinus walls gradually thin because of the increase in size of the maxillary sinus as pneumatization occurs.6 Thus, future implant placement is compromised, necessitating additional surgical procedures. Traditionally, lateral window and internal sinus augmentation procedures have been proposed to facilitate implant placement.7-10
Fugazzotto articulated an alternative approach to sinus augmentation, utilizing a trephine core plus osteotomes.11 When residual bone height was 4 to 5 mm in the posterior maxilla, he found utilization of a trephine created less trauma when compared to traditional internal sinus augmentations. In addition, the technique conserved autogenous bone and minimized the risk of membrane perforation by avoiding a 2-mm twist drill to begin the osteotomy sites.11-13 In his studies, Fugazzotto found 100% success rates in comparison to 97.3% success rate with the lateral approach.14
The trephine core technique can also be utilized to develop sites when simultaneous implant placement is not possible. Maxillary molar extraction sites were found to have a 96% to 97.8% success rate for implants in function for up to 3 years.15-17 In a clinical retrospective study, Kolerman and colleagues showed an 11-year 100% survival rate for implants placed in the maxillary posterior region using this technique.18
The proposed modifications to the trephine core technique allow for implant site development in the posterior maxilla in both single and multiple edentulous sites. Fugazzotto previously demonstrated the technique for immediate implant placement at a maximum length of 8.5 mm.11 The authors have attempted to further develop single and multiple sites to allow for longer length implants. In comparison to 8 mm long implants, implant lengths greater than 10 mm have had a more favorable cumulative success rate (88.9% versus 93.4%)19 with internal sinus lift procedures.
Surgical Technique
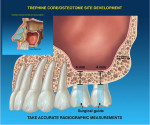
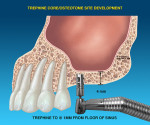
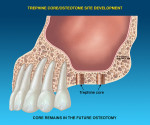
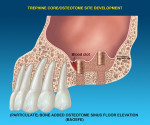
Preoperative radiographic measurements are made to evaluate residual bone height at the site of future implant placement. In edentulous sites, a palatal crestal incision is used. At the time of maxillary molar extractions, a palatal incision around the palatal root is utilized to allow membrane placement. Vertical releasing incisions are made buccally and full-thickness flaps are reflected in conjunction with periosteal releasing incisions to allow flap advancement. A calibrated trephine bur is then used to create a core. The interradicular bone of the maxillary molar usually serves as the core. The trephine core should be a minimum 2 mm less than the bucco-palatal width, ensuring 1 mm of bone on each side. Trephination is approximately 1 mm shy of the sinus membrane. To achieve good contact with the alveolar crest without “skipping of the bur,” the trephine is first used in reverse to engage bone, and then forward to continue cutting.18 Maximum cutting speed is 1200 rpm. Once the trephine core is completed, the lateral walls should be free from adjacent bone, while the core remains intact with the floor of the sinus. A calibrated osteotome is selected, which corresponds to the diameter of the trephine preparation. The osteotome is used with gentle malleting forces to implode the core to a depth of approximately 1 mm less than that of the prepared site. If cone-beam computed tomography confirms a thick schneiderian membrane, the authors have found that you can gently mallet beyond the overlapped area. Once the desired height is achieved, the osteotomy is gently packed with allograft material and covered with a resorbable membrane. In cases where primary closure is not attainable, a non-resorbable dense-PTFE membrane can be utilized.20
Once the membrane is stabilized, mucoperiosteal flaps are replaced and sutured to attempt primary closure. In regards to membrane stability, we have found for small sites, stability can be achieved through a fibrin clot adhesion. In larger sites, tacks can be added for additional stability.
The healing period ranges from 3 to 6 months. At the time of re-entry, implant placement is accomplished either by an additional osteotome internal lift or conventional drilling. A tapered implant design is preferred for increased stability,21 especially in areas where a cortical plate may be thin or missing due to type IV quality bone. The following case reports describe a technique of site development for future implant therapy.
Case Examples
Case 1
A 62-year-old systemically healthy man was referred to the postgraduate periodontics department at Rutgers School of Dental Medicine in Newark, New Jersey, for fixed prosthetic rehabilitation of the left posterior maxilla. Clinical and radiographic (Figure 1) evaluation revealed a non-restorable tooth No. 12 and pneumatized sinus in area 14. Due to poor root anatomy of tooth No. 15, conventional fixed prosthetics was contraindicated. It was proposed to place implants in sites 12 and 14 for implant-supported restorations. Immediate implant placement was not recommended due to presence of periapical pathology in area 12. Site development utilizing the trephine core/osteotome technique was proposed in area 14.
The surgical procedure was performed under local anesthesia (2% lidocaine, 1:100,000 epinephrine). Palatal crestal as well as intrasulcular incisions were made, and full-thickness mucoperiosteal flaps were reflected on the buccal. A trephine bur 2 mm less in diameter than the bucco-palatal width of the molar socket was used to create a core that was apically displaced using gentle malleting forces on osteotomes of similar diameter to elevate the sinus floor (Figure 2). The site was packed with mineralized cortical allograft and a resorbable membrane was placed. The flaps were carefully sutured with 4.0 Vicryl® (Johnson & Johnson, www.jnj.com) to attempt tension-free primary closure. Tooth No. 12 was extracted; the socket was curetted and grafted at the same visit. Radiographs were made following the surgical procedure (Figure 3) and 4 months following site development. Two tapered implants (4 & 5 mm x 11.5 mm) were placed in the maxillary left first premolar and first molar locations (Figure 4). The implants were made of commercially pure titanium with a roughened surface (Biomet 3i, www.biomet3i.com). A 500-mg dose of amoxicillin was prescribed three times per day for 7 days postoperatively. Ibuprofen (600 mg) was prescribed as needed. The patient was instructed to use 0.12% chlorhexidine gluconate (Peridex™, 3M ESPE, www.3mespe.com) rinse twice daily for 10 days. A soft diet and appropriate oral hygiene were recommended for 2 weeks.
Sutures were removed 14 days after the surgical procedure. The postoperative recovery was uneventful. The patient was examined clinically and radiographically each week in the first month after surgery and twice a month in the subsequent 2 months. The healing process was uneventful. Four months after implant placement, a screw-retained metal-ceramic three-unit fixed partial denture was delivered. One year after prosthesis placement, the implants had clinical and radiologic stability (Figure 5). (See online exclusive schematics illustrating this surgical technique in Figure 13 through Figure 18.)
Case 2
A 58-year-old systemically healthy man was referred to the postgraduate periodontics department at Rutgers School of Dental Medicine for evaluation and treatment of the maxillary right first molar (Figure 6). Clinical and radiographic evaluation revealed recurrent subcrestal caries beneath the current prosthesis and the tooth was considered non-restorable. The authors proposed extraction with site development for future implant placement.
The surgical procedure was performed under local anesthesia (2% lidocaine, 1:100,000 epinephrine). The first molar was sectioned and atraumatically extracted using periotomes. Upon extraction, a buccal dehiscence was found. However, good interradicular bone remained. Vertical releasing incisions were made on the buccal aspect to evaluate the extent of the defect. A trephine bur was used to create a core, and a corresponding osteotome was used to gently implode the core, apically displacing the floor of the sinus membrane (Figure 7). The site was packed with mineralized cortical allograft and a resorbable membrane was placed over the socket, making sure to cover the buccal defect. Flaps were released on the buccal and carefully sutured using 4.0 Vicryl to achieve tension-free primary closure. Radiographs were made following the surgical procedure (Figure 8). A 500-mg dose of amoxicillin was prescribed three times per day for 7 days postoperatively. Ibuprofen (600 mg) was prescribed as needed. The patient was instructed to use 0.12% chlorhexidine gluconate rinse twice daily for 10 days. A soft diet and appropriate oral hygiene were recommended for 2 weeks.
Sutures were removed 14 days after the surgical procedure. The postoperative recovery was uneventful. The patient was examined clinically and radiographically each week in the first month after surgery and twice a month in the subsequent 2 months. The healing process was uneventful. There were no sinus complications. A tapered implant (5 mm x 11.5 mm) was placed in the maxillary right first molar position 4 months following site development (Figure 9). A screw-retained metal-ceramic implant crown was delivered 6 months following implant placement. One year after prosthesis placement, the implant was clinically and radiographically stable (Figure 10).
Discussion
Sinus augmentation procedures are widely performed to correct vertical deficiencies encountered in the posterior maxillary region to enable optimal implant placement. While the lateral window approach has been used successfully as a sinus augmentation procedure, there are several disadvantages to this technique. It is more invasive in comparison to an internal approach, and technically more demanding when adjacent teeth are present. The risks of membrane perforation as well as postoperative complications are higher.22 Therefore, a less invasive technique designed to achieve the same goals may prove beneficial.
The trephine core technique is advantageous in a clinical setting. It is a sinus augmentation and site development procedure that is less invasive than the lateral window approach. While membrane perforation is a potential complication, this procedure has fewer postoperative complications and less risk of membrane perforation than the lateral window technique since the autogenous core is attached to the schneiderian membrane, allowing a cushion between surgical instruments and the floor of the sinus. It is a relatively simple procedure with short chairside time, allowing for increased case acceptance.
The modified technique of the trephine core/osteotome procedure can be used in different clinical settings. The technique is useful in cases such as: 1) single edentulous sites where simultaneous implant placement is not achievable; 2) compromised single molar sites where anatomical restrictions and adjacent teeth complicate the lateral window approach;16 3) at the time of maxillary first molar extractions; and 4) when employing multiple trephine cores to augment the sinus for long span edentulous sites in the posterior maxilla. Anatomical considerations that may be encountered, such as an uneven sinus floor, or a thicker schneiderian membrane, can be surgically managed applying this technique in combination with piezosurgery to successfully displace the cores (Figure 11 and Figure 12). Through the use of slow controlled malleting, extensive augmentation of the sinus can be accomplished from the crestal approach rather than the lateral window approach. Additionally, unlike the conventional Summers technique, this novel approach allows multiple site developments for the addition of multiple implant fixtures performed in a single surgical procedure.
Conclusions
The trephine core/osteotome technique has been previously described in the literature to facilitate immediate implant placement in the maxillary molar region. In the publications by Fugazzotto,11-14 he was able to place 8.5 mm length implant fixtures utilizing this technique. Few studies to date have shown the benefits of this technique for site development. The case reports presented illustrate modifications to the proposed technique, which facilitate longer length implant placement (>8.5 mm) in the maxillary molar region. These adaptations support previous studies that show an increased success rate for implant lengths greater than 8.5 mm.19 This novel approach has also taken advantage of both single and multiple edentulous sites. The use of multiple trephine cores to efficiently augment the sinus in a single surgical procedure decreases time for re-entry when compared to the lateral window approach.
This technique increases bone height to allow longer length implant placement, and implant success in the posterior maxilla.
Acknowledgements
The authors wish to acknowledge Drs. Amy Ovaydi, Nidhi Shah, and Sofia Petrov for assisting on the cases.
Disclosures
The authors have no relevant conflicts of interest to disclose.
About the Authors
Anna M. Brunetti, DMD, MDS
Assistant Clinical Professor
Department of Periodontics
Rutgers School of Dental Medicine
Newark, New Jersey
Private Practice
Red Bank, New Jersey
Howard Drew, DMD
Clinical Professor
Department of Periodontics
Rutgers School of Dental Medicine
Newark, New Jersey
Andrew Sullivan, DDS
Clinical Professor and Interim Chairman
Department of Periodontics
Rutgers School of Dental Medicine
Newark, New Jersey
Joel Pascuzzi, DMD
Clinical Professor
Department of Periodontics
Rutgers School of Dental Medicine
Newark, New Jersey
Emil Cappetta, DMD
Clinical Professor
Department of Periodontics
Rutgers School of Dental Medicine
Newark, New Jersey
References
1. Johnson K. A study of the dimensional changes occurring in the maxilla following tooth extraction. Aust Dent J. 1969;14(4):241-244.
2. Lil W, Blahout R, Ulm C, et al. Reduction of the maxillary implant site with the degree of atrophy [in German]. Z Zahnärztl Implantol. 1992;8:54-61.
3. Fugazzotto PA, Wheeler SL, Lindsay JA. Success and failure rates of cylinder implants in type IV bone. J Periodontol. 1993;64(11):1085-1087.
4. Chrcanovic BR, Albrektsson T, Wennerberg A. Reasons for failures of oral implants. J Oral Rehabil. 2014;41(6):443-476.
5. Jaffin RA, Berman CL. The excessive loss of Bränemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991;62(1):2-4.
6. Solar P, Aro G, Ulm C, Bernhart T. The effects of tooth loss on the anatomy of the maxilla [in German]. Schweiz Monatsschr Zahnmed. 1998;108(9):871-878.
7. Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38(8):613-616.
8. Tatum H Jr. Maxillary and sinus implant reconstructions. Dent Clin North Am. 1986;30(2):207-229.
9. Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007;22(suppl):49-70.
10. Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15(2):152-160.
11. Fugazzotto PA, Vlassis J. Long-term success of sinus augmentation using various surgical approaches and grafting materials. Int J Oral Maxillofac Implants. 1998;13(1):52-58.
12. Fugazzotto PA. Sinus floor augmentation at the time of maxillary molar extraction: technique and report of preliminary results. Int J Oral Maxillofac Implants. 1999;14(4):536-542.
13. Fugazzotto PA. Treatment options for augmentation of the posterior maxilla. Implant Dent. 2000;9(3):281-287.
14. Fugazzotto PA. The modified trephine/osteotome sinus augmentation technique: technical considerations and discussion of indications. Implant Dent. 2001;10(4):259-264.
15. Fugazzotto PA, De PS. Sinus floor augmentation at the time of maxillary molar extraction: success and failure rates of 137 implants in function for up to 3 years. J Periodontol. 2002;73(1):39-44.
16. Toffler M. Staged sinus augmentation using a crestal core elevation procedure and modified osteotomes to minimize membrane perforation. Pract Proced Aesthet Dent. 2002;14(9):767-774.
17. Toffler M. Minimally invasive sinus floor elevation procedures for simultaneous and staged implant placement. NY State Dent J. 2004;70(8):38-44.
18. Kolerman R, Moses O, Artzi Z, et al. Maxillary sinus augmentation by the crestal core elevation technique. J Periodontol. 2011;82(1):42-51.
19. Ferrigno N, Laureti M, Fanali S. Dental implants placement in conjunction with osteotome sinus floor elevation: a 12-year life-table analysis from a prospective study on 588 ITI implants. Clin Oral Implants Res. 2006;17(2):194-205.
20. Maridati P, Cremonesi S, Fontana F, Maiorana C. Treatment of a dense PTFE membrane exposure: a case report. Clin Oral Impl Res. 2014;5(Suppl.10):617.
21. O’Sullivan D, Sennerby L, Meredith N. Influence of implant taper on the primary and secondary stability of osseointegrated titanium implants. Clin Oral Implants Res. 2004;15(4):474-480.
22. Soltan M, Smiler DG. Trephine bone core sinus elevation graft. Implant Dent. 2004;13(2):148-152.