You must be signed in to read the rest of this article.
Registration on AEGIS Dental Network is free. Sign up today!
Forgot your password? Click Here!
Communicating Shade Between Dental Clinic and Laboratory
Using the eLAB system
By Taylan Sari, CDT - MDC; Nathaniel Lawson, DMD, PhD; Chin-chuan Fu, DDS, MS, FACP; Galip Gurel, DDS, MSc
Shade matching crowns using a conventional shade guide is limited by the color perceptibility of the operator recording the shade,1 the limited range of shades in the shade guide,2 and the variation in color between different shade guides and ceramic systems.3 Electronic shade-taking devices have been developed to aid in standardization of shade taking; however, most systems are only used to give the technician general locations of shade within the tooth. This article will give a brief overview of a new shade matching system, present a pilot study conducted to generate a chart for selecting the shade of lithium disilicate blocks, and present a case to demonstrate this system.
Digital photography can be used by the dentist and technician team as a versatile tool to communicate both a shade and shape map. One limitation of digital photography, however, is that the accuracy of a shade in a photograph may not deliver a true representation of color from the patient's mouth to the computer screen in the laboratory. There are multiple reasons for these inaccuracies, including variations in the light source of the photograph, in the sensor in the digital camera, in the settings on the camera, in the processing of the photograph, and even in the display of the computer monitor used to view the final image. In order to correct for these inaccuracies, one approach would be to color correct each step of the process to end up with a true representation of the tooth on the computer screen.4 This approach still requires the technician to then visually match the color of the tooth on the screen with the crown on the bench.
Another approach, developed by renowned dental technician Sascha Hein, is referred to as "eLABor_aid," or "eLAB" for short. This approach has been thoroughly documented,5 and it will be briefly summarized in this article. In essence, a standardized photograph is taken of the teeth with a specialized gray card, the photograph is processed with known parameters, and then color data is measured on the image and matched with data that have been measured for ceramic systems and placed into charts.
The first step is to capture a standardized photograph (Figure 1). This is accomplished with a DSLR camera and 60- or 105-mm macro lens. Either two mounted speedlights or a ringflash can be used and then modified with a polarized filter (polar_eyes Cross Polarization Filter, PhotoMed, photomed.net) to remove the surface glare. Defined settings are set on the camera (shutter speed 1/125, aperture of f22, ISO 100, manual flash 1/1). The photo is then taken at a standard distance5 with a gray card (white_balance Gray Reference Card, PhotoMed) placed in the plane of the neighboring intact teeth. The .raw file of the image is analyzed using photo editing software (Adobe Lightroom, Adobe, adobe.com). White balance and exposure balance are performed based on the gray card.
The most unusual aspect of this technique is that the corrected image is then used to determine L*a*b* color values at any spot on the tooth. L*a*b* is a method for defining color consisting of three components. "L" is a measure of value (ie, brightness) with larger numbers representing higher value (increased brightness). "a" measures the intensity of red, and "b" measures the intensity of yellow. Using a software application (Digital Color Meter, Apple, apple.com), the L*a*b* values for any spot on the tooth can be determined by dragging the computer cursor over that area of the tooth. This process has been documented in several online videos.6 The usefulness of these L*a*b* values is that they can be matched to the known L*a*b* values of commercially available dental ceramics.
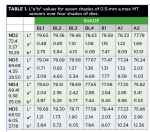
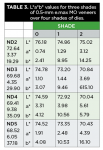
The L*a*b* values of commonly used dental ceramics at 2-mm thickness have been measured and are provided as a reference chart. These charts can be produced by individual technicians themselves or obtained through continuing education courses. This information is used by the technician when choosing the shade of veneering porcelain. One challenge with these standard charts is that they do not account for any changes in the color of the final ceramic restoration imparted by an underlying tooth preparation. Therefore, the authors undertook a pilot study to determine the L*a*b* values of various shades of 0.5 mm e.max CAD (Ivoclar Vivadent, ivoclarvivadent.com) on top of various shades of tooth preparations using the eLAB system.
Pilot Study to Create Shade Chart
A stone Gellar model was produced with pink silicone on the gingival area to replicate the oral condition. A stone maxillary central incisor die was prepared to achieve a veneer preparation of 0.5-mm thickness on the facial surface. A wax veneer was hand prepared to achieve an even 0.5-mm thickness, which was measured by caliper. The stone die and wax pattern were scanned and the 0.5-mm monolithic veneer was designed using inLab CAD Software (Dentpsly Sirona). The veneer thickness was confirmed in the software. The stone tooth preparation die was then duplicated using a clear silicone mold. The mold was filled with a die material (IPS Natural Die Material, Ivoclar Vivadent) of four different shades (ND2, ND3, ND4, and ND5) to produce one duplicate in each shade. e.max CAD veneers were then milled using seven shades in the LT translucency (BL1, BL2, BL3, BL4, B1, A1, and A2), six shades in the MT translucency (BL2, BL3, BL4, B1, A1, and A2), and three shades in the MO translucency (0,1, and 2). The veneers were coated with a layer of spray glaze and crystallized according to the manufacturer's recommendations.
Each combination of tooth die and veneer were then photographed according to the eLAB protocol (Figure 2). The veneers were placed on the tooth models using a thin layer of glycerine. A Nikon D7200 (Nikon, nikonusa.com) with a 105-mm lens and R1C1 flash kit was used with the polar_eyes polarization filter. The images were taken with a reproduction ratio of 1:1.8. The camera settings were shutter speed 1/125, aperture f22, ISO 100, manual flash 1/1. The white_balance Gray Reference Card was placed and fixed in the plane of the veneer when the photographs were taken. The images were then processed in Adobe Lightroom. First, the camera profile was adjusted for the Nikon D7200. The white balance was set based on the color of the gray card and the exposure balanced by changing the luminosity until the gray card read its known value (L*79). L*a*b* values were then collected for each veneer using the Digital Color Meter software. The tooth was measured at three points in the middle area of the tooth. Prior to selecting each point of measurement, the cursor was hovered around the general area to ensure that the L*a*b* value was in the range of surrounding points to prevent recording any anomalies. The three measurements were averaged and the average L*a*b* values for each veneer/die combination were placed into Table 1 through Table 3. These charts allow the technician to choose a shade and translucency of e.max CAD based on the desired color of the tooth and the color of the tooth preparation. Only the higher value shades were tested in this pilot study as anecdotal experience reveals that these shades are more affected by the color of the tooth substructure. Also, e.max HT (Ivoclar Vivadent) was not tested as it was assumed that this translucency would not be used if there was concern regarding the color of the substructure. This technique will be demonstrated in a clinical example.
Case Study
Teeth Nos. 8 and 9 were prepared for e.max CAD crowns. The dentist provided information that the tooth preparation shade was close to an ND6 (Figure 3). Using the eLAB protocol, the dentist provided a digital image of teeth Nos. 22 through 27 (Figure 4). In this case, the dentist could have also provided images of teeth Nos. 6 through 8 and Nos. 9 through 11. The camera profile was adjusted for the Nikon D7200 (Figure 5). The white balance was set based on the color of the gray card (Figure 6 and Figure 7) and the exposure balanced by changing the luminosity until the gray card read its known value (L*79) (Figure 8) in Adobe Lightroom. Using the Digital Color Meter software, the L*a*b* values of the cervical areas of teeth Nos. 23 and 24 were measured (Figure 9). These values were compared to Table 1 through Table 3 and based on these values, a block shade of A2 LT was selected. This block had a higher value and lower chroma than the target shade. After the e.max CAD crown was milled, a cut-back was performed on the crown. Additional porcelain and external staining was applied using the VITA VM 9 and VITA AKZENT Plus systems (VITA North America, vitanorthamerica.com). Throughout the layering/staining process, additional photographs were taken on a die material and the L*a*b* values of the crowns were compared to the reference photograph until a similar L*a*b value was achieved. At the time of try-in (Figure 10), the L*a*b* values of the crowns were compared to the original values of mandibular incisors (Figure 11).
When selecting the shade of the coping, it is desirable to select a material with a slightly higher L* value and lower a* and b* values as it will be easier to decrease value (lower L*) and add chroma (increase a* and b*) to the crown. For the shade of a central incisor based on a lateral incisor, it is recommended to choose a material with slightly lower a* and b* values, as the lateral incisors are slightly more chromatic than the central incisors.
Conclusion
The eLAB system is a standardized method for communicating shade between the clinic and the laboratory and selecting a shade of ceramic to match the neighboring teeth. This article provides a reference chart for selecting the shade of lithium disilicate coping using the eLAB system, accounting for the color of the tooth substructure.
About the Authors
Taylan Sari, CDT - MDC
Taylan Sari Dental Studio
Istanbul, Turkey
Nathaniel Lawson, DMD, PhD
Assistant Professor
University of Alabama Birmingham
Division of Biomaterials, School of Dentistry
Birmingham, Alabama
Chin-chuan Fu, DDS, MS, FACP
Associate Professor
University of Alabama Birmingham School of Dentistry
Birmingham, Alabama
Galip Gurel, DDS, MSc
Dentis Dental Clinic
Istanbul, Turkey
References
1. Bahannan SA. Shade matching quality among dental students using visual and instrumental methods. J Dent. 2014 Jan;42(1):48-52.
2. Bayindir F, Kuo S, Johnston WM, Wee AG. Coverage error of three conceptually different shade guide systems to vital unrestored dentition. J Prosthet Dent. 2007 Sep;98(3):175-85.
3. Lee YK, Yu B, Lee SH, Cho MS, et al. Shade compatibility of esthetic restorative materials-A review. Dent Mater. 2010 Dec;26(12):1119-26.
4.> McLaren EA, Figueira J, Goldstein RE. A Technique Using Calibrated Photography and Photoshop for Accurate Shade Analysis and Communication. Compend Contin Educ Dent. 2017 Feb;38(2):106-113.
5. Hein S, Tapia J, Bazos P. eLABor_aid: a new approach to digital shade management. Int J Esthet Dent. 2017;12(2):186-202.
6. white_balance Gray Reference Card Set (product description). Photomed Web site. https://www.photomed.net/white_balance.htm.