You must be signed in to read the rest of this article.
Registration on AEGIS Dental Network is free. Sign up today!
Forgot your password? Click Here!
Critical Factors for Successful Restorations: Light-Curing, Light-Energy Monitoring, and Matrices
Howard E. Strassler, DMD; and Nisha F. Ganesh, DDS
The clinical success of light-cured adhesive composite resin restorations depends heavily upon attention to detail in each of the steps required to diagnose, prepare, and restore. While much attention has been given to the intricacies of diagnosis and preparation and the development of improved adhesives and resins, light-curing is often taken for granted. Various factors must be taken into account when light-curing resin adhesives, resin-based composites, resin cements, and other light-activated restorative materials to ensure optimal polymerization of the restoration. Proper use of curing lights and matrix systems, as well as correctly measuring the effectiveness of the curing light, all contribute to the successful outcome of light-cured composite resin restorations.
Dental Light-Curing Devices
Clinicians have choices in the light-curing units (LCUs) they use. Factors such as spectra wavelength, power density and energy delivered to the tooth and light-activated restorative being placed, timing for use, availability of accessories, configuration of curing probes/tips, energy source to power the device, and others vary with different LCUs.1,2 While the earliest light-cured composite resins were photoinitiated with ultraviolet light (wavelength 10 nm to 400 nm), current composite resins are photopolymerized predominantly with blue light (wavelength ~ 420 nm to 480 nm). Use of a blue light source and a camphoroquinone (CQ) photoinitiator enabled the opportunity to achieve a greater depth of cure for more efficient restoration placement.3
The earliest LCUs compatible with CQ-photoinitiated composite resin used quartz halogen (QTH) light sources; the light emitted was very broad spectrum, ranging between violet and red. Typically, these curing lights adequately polymerized all composites. Currently, the most popular curing lights use high-energy blue light-emitting diodes (LEDs). LED curing lights provide the benefits of being lightweight, battery-powered, and, in many cases, quieter by eliminating noisy fans required by QTH curing lights.
Though CQ is a highly efficient chemical initiator, concerns arose that until these composites were light-cured they had inherent yellow coloration as a result of the CQ.3 Fortunately, in most cases, once they were light-cured the yellowish-colored CQ-based composites bleached to the desired shade. In response to this concern some manufacturers controlled the yellow coloration of CQ and enhanced the ability of their brand of composite to light-cure by adding a clear photoinitiator—either monoacylphosphine (TPO) or phenylpropanedione (PPD)—that was sensitive to the violet spectrum (wavelength ~ 320 nm to 420 nm).3 One manufacturer addressed this issue by developing its own proprietary photoinitiator (Ivocerin®, Ivoclar Vivadent, ivoclarvivadent.com) that has an extended wavelength of violet to blue (370 nm to 460 nm).
Because considerable variations exist in the chemical formulations, shade filler types, and light transmission characteristics of composite resins,4,5 clinicians often may be unsure if their light-curing device will adequately cure the material they are placing. Most LED curing lights use only blue wavelength emitters (single-peak), but some also have violet LED emitters (polywave). Currently, there is no clear evidence of the effect of using a polywave light with a CQ-only composite or of using a blue LED with a composite with a CQ and TPO or other photoinitiator. One recommendation is for clinicians to select a curing light with a spectral irradiance (light output) that is matched to the light-cured composite they are using.5,6
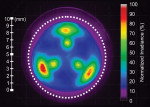
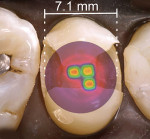
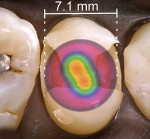
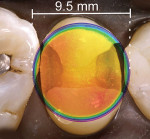
Not all light-curing devices are equivalent.1,2,7 Irradiance values ranging from at least 600 mW/cm2 to 1000 mW/cm2 have been recommended.2 Also, LED LCUs can vary considerably in their light output and emission spectra.2 While irradiance values are the most common benchmark used when comparing curing lights, they do not provide a complete picture of the critical factors that need to be considered when choosing a curing light.2,6 With the use of a laser-beam analyzer, one can now measure the irradiance value and power distribution across the entire surface of a LCU. Power distribution is also referred to as beam profiling of a curing light across the surface of the light tip.6,8,9 A beam profile demonstrates the locations and radiant intensities on the surface of the light tip where energy is being delivered. For some lights, the power is uniformly distributed over the entire surface of the light tip, which is referred to as a “top hat” appearance, while for others the power is predominantly delivered only in the center of the tip with a rapid fall-off at the edges of the light guide. In other lights, the profile may appear to be like hills and valleys, with inconsistent and uneven radiant energy dispersion (Figure 1).6,8,9
The clinical implication of a beam profile is that if an overlay of the beam profile was placed on a tooth preparation it would demonstrate the regions of the preparation that are not receiving adequate radiant exposure to cure a dental resin (Figure 2 through Figure 4).10 When selecting a new LCU or to better understand the light-curing capacity of their current LCU, clinicians can request this information from the manufacturer.
Curing-Light Effectiveness and Safety
Manufacturers provide an irradiance value to describe the energy a curing light delivers at its tip. But, how can dentists monitor the irradiance of their curing light? In-office curing-light measurement systems, or radiometers, can be used to measure the light energy at the tip of the light guide. Using these devices and maintaining a weekly or monthly log of the values will provide a baseline for changes in a LCU. Unfortunately, though they are useful for monitoring change, most radiometers are inaccurate in providing actual irradiance values.6,11,12
Understanding irradiance values alone does not ensure adequate photopolymerization. While irradiance multiplied by the duration of light-curing equals total energy in joules/cm2 that a composite would need for curing appears to be a correct formula, it has been found that there is a reciprocity factor when curing composites.13 Some manufacturers provide the information regarding the energy required for polymerization in their instructions. For all LCUs an energy drop-off occurs over distance that decreases the amount of energy delivered to the restoration. The gingival margin of a Class II restoration, for example, will require additional curing time.14,15
Good clinical techniques also must be followed to assure optimal polymerization. These include holding the light in a stable position during the curing cycle, accessing the tooth being restored at right angles with the light guide for straight line access for curing, air-cooling the tooth to prevent overheating during the curing cycles, and paying close attention when light-curing.16
As for curing-light safety, orange light shields on curing lights offer protection from the blue light hazard. The dentist and staff are at risk for ocular damage from blue light radiation.17,18 High levels of blue light radiation may cause accelerated retinal aging and age-related macular degeneration.19 The operator and chairside assistant should wear protective orange eyeglass lenses when light-curing.6,20
Matrix Systems for Posterior Composite Resins
While the routine placement of Class I composite resin restorations does not present significant challenges, placing a Class II restoration and achieving proximal contact can be daunting. Composite resin, unlike dental silver amalgam, is not packable and cannot move a matrix band to achieve an anatomic proximal contact. Composite resin by its chemistry is a viscous liquid that may be moved and displaced but is not made to be more dense during placement.21,22
To address this problem, specialized matrix systems have been designed that allow the clinician to achieve an anatomic proximal contact. Thin, dead-soft, stainless-steel matrices (0.001-inch thickness) for use with a Tofflemire retainer and sectional matrices (0.001-inch) to be used with metal, spring-like rings provide advantages over thicker, more rigid stainless-steel matrices (0.002-inch and 0.0015-inch) used for dental silver amalgam placement. These ring systems, some of which feature enhanced silicone or composite wings, have the advantages of providing additional wedging of teeth to create separation to compensate for the thickness of the matrix band to ensure good proximal contact; enabling better contouring on the facial and lingual surfaces, especially when the preparation extends beyond the tooth line angles; and delivering a more anatomic contour. They are particularly useful for single proximal surface placement when compared to use of a circumferential band.22,23
References
1. Price RB, Ferracane JL, Shortall AC. Light-curing units: a review of what we need to know. J Dent Res. 2015;94(9):1179-1186.
2. Rueggeberg FA. State-of-the-art: dental photocuring – a review. Dent Mater. 2011;27(1):39-52.
3. Santini A, Gallegos IT, Felix CM. Photoinitiators in dentistry: a review. Prim Dent J. 2013;2(4):30-33.
4. Shortall AC. How light source and product shade influence cure depth for a contemporary composite. J Oral Rehabil. 2005;32(12):906-911.
5. Price RB, Fahey J, Felix CM. Knoop hardness of five composites cured with single-peak and polywave LED curing lights. Quintessence Int. 2010;41(10):e181-e191.
6. Strassler HE, Price RB. Understanding light curing, part 1. Delivering predictable and successful retorations. Dent Today. 2014;33(5):114-118.
7. Ferracane J, Watts DC, Barghi N, et al. Effective use of dental curing lights: a guide for the dental practitioner. ADA Professional Product Review. 2013;8(2):2-12.
8. Price RB, Rueggeberg FA, Labrie D, Felix CM. Irradiance uniformity and distribution from dental light curing units. J Esthet Restor Dent. 2010;22(2):86-101.
9. Michaud PL, Price RB, Labrie D, et al. Localised irradiance distribution found in dental light curing units. J Dent. 2014;42(2):129-139.
10. Palin WM, Senyilmaz DP, Marquis PM, Shortall AC. Cure width potential for MOD resin composite molar restorations. Dent Mater. 2008;24(8):1083-1094.
11. Price RB, Labrie D, Kazmi S, et al. Intra- and inter-brand accuracy of four dental radiometers. Clin Oral Investig. 2012;16(3):707-717.
12. Shimokawa CA, Harlow JE, Turbino ML, Price RB. Ability of four dental radiometers to measure the light output from nine curing lights. J Dent. 2016;54:48-55.
13. Feng L, Carvalho R, Suh BI. Insufficent cure under the condition of high irradiance and short irradiation time. Dent Mater. 2009;25(3):283-289.
14. Felix CA, Price RB. The effect of distance from light source on light intensity from curing lights. J Adhes Dent. 2003;5(4):283-291.
15. Xu X, Sandras DA, Burgess JO. Shear bond strength with increasing light-guide distance from dentin. J Esthet Restor Dent. 2006;18(1):19-27.
16. Price RBT. Light curing in dentistry. Dent Clin North Am. 2017;61(4):751-778.
17. Labrie D, Moe J, Price RB, et al. Evaluation of ocular hazards from 4 types of curing lights. J Can Dent Assoc. 2011;77:b116.
18. Price RB, Labrie D, Bruzell EM, et al. The dental curing light: a potential health risk. J Occup Environ Hyg. 2016;13(8):639-646.
19. Ham WT Jr, Mueller HA, Sliney, DH. Retinal sensitivity to damage from short wavelength light. Nature. 1976;260(5547):153-155.
20. Price RB. Light curing guidelines for practitioners: a consensus statement from the 2014 symposium on light curing in dentistry, Dalhousie University, Halifax, Canada. J Can Dent Assoc. 2014;80:e61.
21. Strassler HE, Trushkowsky RD. Predictable restoration of Class 2 preparations with composite resin. Dent Today. 2004;23(1):93-99.
22. Loomans BA, Opdam NJ, Roeters JF, et al. Influence of composite resin consistency and placement technique on proximal contact tightness of Class II restorations. J Adhes Dent. 2006;8(5):305-310.
23. Hilton TJ, Broome JC. Direct posterior esthetic restorations. In: Summitt JB, Robbins JW, Hilton TJ, Schwarts RS, eds. Fundamentals of Operative Dentistry. 3rd ed. Hanover Park, IL: Quintessence Publishing;2006:289-339.