You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Hand instrumentation kits used when performing dental hygiene recare maintenance as well as for patients requiring more complex scaling and root planing (SRP) can contain as many as 12 instruments. These instruments are well-established for the efficient and complete removal of plaque biofilm, extrinsic stain, and calculus deposits. Whether the selected instrumentation is for recare maintenance or complex scaling and root planing, instruments are used in a sequential order for patient treatment (i.e., examination and diagnosis, initial therapy, SRP, etc.).1 However, most dental hygienists only use two to four instruments from either the recare maintenance or the SRP kit during an entire treatment procedure. Dental hygienists often continue using the same instruments and tip designs they were taught to use in dental hygiene school (Figure 1), despite recent handle design innovations and metallurgy advancements that have been designed in an extremely competitive dental hand instrumentation marketplace.
Reasons cited by dental hygienists for not evaluating or incorporating new instruments or tip designs include limited time to experiment with and explore newer options and budgetary constraints. Limited budget allocation to the dental hygiene department must be prioritized to purchase instruments that are critical for dental hygiene procedures. If a new instrument is added, something has to be removed from the kit. Cost concerns that prevent scheduled replacement of critical instruments contribute to retention of instruments that are not sufficiently sharp, tip blades that are too thin, and ultrasonic inserts and equipment that are not functioning optimally. Consequently, dental hygienists experience ergonomic-related exhaustion at the end of the workday.
Because dental hygiene hand instruments are commodity products in the dental office, the need to replace them is inevitable. Sickle scalers and curettes have a limited-use life due to the fact that they must be sharpened to remain effective. Leading hand instrument manufacturers suggest that the use life of a quality scaler or curette is between 6 and 12 months, which could equate to 600 to 1,200 uses. Ironically, frequent sharpening preserves an instrument’s working design while ensuring optimal clinical results from the dental hygiene treatment.2,3 Combined with care during handling and sterilization, maintenance sharpening can prolong instrument-use life. When working ends become too thin, instruments must be discarded, making inspection paramount. The industry-suggested use life of scalers and curettes may be significantly longer depending on the frequency of ultrasonic use by the dental hygienist. Increased use of ultrasonics (magnetostrictive and piezo) can reduce the amount of time that the dental hygienist uses hand instruments during treatment procedures, resulting in less frequent sharpening and wear of scalers and curettes. Regardless of whether the dental hygienist uses hand instruments or an ultrasonic for scaling procedures, the office must budget for periodic replacement. Common clinical concerns a dental hygienist may encounter related to using hand instruments and ultrasonic inserts/tips that have exceeded use life are: burnished calculus, inadequate deposit removal, patient and clinician discomfort, and instrument tip breakage.
Unfortunately, opting for cheaper instruments to save money is often not cost-effective, because such instruments wear quickly and are more likely to break and require more frequent replacement. It is more advantageous for dental hygienists to maximize their allocated budgets by purchasing only high-quality instruments when promotions are offered. Investigate promotions offered at state and national dental and dental hygiene conferences or ask company representatives who visit the office. If a monthly dental hygiene budget has not been established, discuss the benefit of making smaller, more frequent purchases instead of large annual purchases. Negotiate a hand instrument replacement budget between $125 and $150 monthly for replacing worn or broken instruments or evaluating newer designs. The amount will vary depending on how many dental hygienists are in the practice. It is also important to maintain an instrument replacement budget that is separate from the practice’s consumable products (i.e., prophy angles, gloves, paste, toothbrush, etc.) budget.
Evaluating Hygiene Hand Instrumentation Options
Interestingly, simplifying dental hygiene instrumentation for different types of patient appointments is among the ways that the challenges associated with budgetary constraints and outdated hand instruments can be minimized. Cassettes containing fewer and more innovative instruments require less of an initial investment and are less costly to maintain. Better quality instruments may be more durable and, therefore, require less frequent sharpening and replacement. Additionally, instruments manufactured with new innovative designs and metallurgy can work more efficiently, effectively with improved ergonomics. In fact, to minimize the risk of the musculoskeletal disorders that are common among dental hygienists, selecting instrumentation with different weights, metallurgy compositions, and handle designs (Figure 2) has been advocated.4
Many instruments available from leading hand instrument manufacturers demonstrate features and benefits that can be desirable for dental hygiene treatment procedures. Ultimately, dental hygienists must consider all relevant product information to determine which instruments will fit their needs in practice and budget.
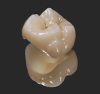
For example, Ever Edge 2.0 (Hu-Friedy, www.hu-friedy.com) is reported by the manufacturer to be 72% sharper out of the box than the next closest competitor.5 Similarly, the manufacturer of XP® Instruments (American Eagle Instruments Inc., http://am-eagle.com) claims that its scaling instrument—which features a very fine, sharp, and smooth edge designed for more efficient root planing—never needs to be sharpened. Corporate information about PDT instruments (Paradise Dental Technologies, www.pdtdental.com) states that the company’s instruments last two to seven times longer than competitive products as a result of innovative heat-treating and cryogenic processes that create a uniform and smooth molecular grained steel structure.6 The manufacturer of the Next Generation handle (Brasseler USA, www.brasselerusadental.com) notes that this instrument’s tips are tempered to 52 to 56 Rockwell C hardness, which produces a long-lasting, sharper instrument that is easy to sharpen. The Next Generation handle is ultralight at 16.4 g with an elongated handle neck to ensure proper finger placement for better ergonomics (Figure 3).
Before going through the exercise of simplifying hand instrumentation, priority should be given to ensuring that power equipment (e.g., magnetostrictive and piezo ultrasonic scalers) work properly. Ultrasonic scaling devices are increasingly being used as adjuncts to hand scaling. A blended approach combining hand and ultrasonic instrumentation is considered ideal for optimal clinical efficacy in patients requiring SRP treatment.7,8 A combined manual and ultrasonic SRP approach can successfully control subgingival bacterial populations, remove calculus, establish root smoothness, reduce probing depths, increase attachment levels, and reduce bleeding on probing and gingival inflammation.7,8 Piezo ultrasonic devices are also gaining in popularity among hygienists for SRP based on the smooth surface they produce.9
Reviewing and Simplifying Common Instrumentation
The first step in simplifying dental hygiene instrumentation is determining which instruments are critical to improve treatment outcomes and then removing instruments that are not important or used. This evaluation affects patient care in terms of effectively removing biofilm, calculus, and stain, as well as both patient and clinician comfort during treatment. The significant savings that can be realized from this task alone can then be re-allocated for instrument replacement and/or incorporating new instrument designs.
Typical dental hygiene cassettes purchased at most dental hygiene schools include sickle scalars (Figure 4), universal curettes (Figure 5), and Gracey curettes (Figure 6), in addition to extended-reach Graceys, periodontal files, diamond finishing files, and various diagnostic instruments (Table 1). In the average dental practice, however, hygiene instruments typically can be organized into recare/maintenance cassettes and periodontal SRP cassettes.
Recare/maintenance cassettes can contain a mirror handle and face, a probe (e.g., single-ended probe or combined with an explorer tip), anterior sickle and posterior sickle, anterior curette, and one to two universal curettes. The cassette may also contain a universal ultrasonic insert. Including the costs of the ultrasonic insert and the cassette itself, this entire set-up (Figure 7) might retail for approximately $488, although most companies would offer a quantity discount, lowering the cost as much as 25% to approximately $366. Practices that see eight to 10 patients a day should have eight to 10 dental hygiene maintenance treatment cassettes available to easily facilitate a full day of scheduled patients. Access to the ideal number of dental hygiene treatment cassettes prevents using the same instruments repeatedly throughout the day. Availability of the ideal quantity of dental hygiene treatment cassettes could be cost-prohibitive; therefore, it is important to determine which instruments are necessary based on the dental hygiene examination and which instruments are actually used on every patient, as well as how the instruments will be contained (i.e., pouches or cassettes). Cassettes are ideal for containment because they are safer, require less instrument handling, and provide greater protection against instrument damage.
Diagnostic instruments are critical; therefore, the mirror handle and mirror face must be included. An explorer and probe are also needed, but an instrument that combines both (e.g., EXPRO, which combines an explorer and probe with preferred mm markings) can be selected. Dental hygienists typically rely on an anterior sickle scaler, a posterior sickle scaler, and universal curettes. However, whether two universal curettes are necessary for all patients is questionable. An alternative is to include a hybrid instrument that combines an anterior sickle and a curette (Figure 8), along with a posterior sickle and a medium posterior universal curette, both of which are available in a variety of new designs that have become popular among dental hygienists (Table 2). A universal ultrasonic insert can also be included.
By reducing the number of instruments in this cassette set-up by two, the size of the cassette itself can also be reduced, bringing the total cost down to $366 versus $488. An additional cost reduction could also be achieved by removing the ultrasonic insert and storing it in a separate cassette or pouch, ultimately realizing a discounted cost of $271.
Patients with periodontal disease, on the other hand, require treatments that are performed using more advanced instruments in an SRP cassette. These cassettes typically contain a mirror handle and mirror face, explorer and probe, Graceys with a longer terminal shank (e.g., buccolingual, mesial, and distal Gracey curettes), anterior sickle, posterior sickle, a medium posterior universal curette (e.g., Barnhart 1/2; Columbia 4R/4L), and two ultrasonic inserts (e.g., 100 slim for finishing and a triple bend for difficult calculus removal). This ideal SRP cassette set-up (Figure 9) might retail for as much as $700. If a quantity discount of 25% is offered by the instrument supplier, the cost can be reduced to approximately $528 for one procedure cassette.
Simplifying the SRP instrumentation can be accomplished in a manner similar to streamlining the recare/maintenance cassette. First, determine the desired method of containment (e.g., cassette or pouch) and then identify the instruments that are critical for achieving successful treatment outcomes. For diagnostic purposes, a mirror handle and mirror face will be selected, along with a thin explorer to ensure no residual calculus remains on tooth surfaces (e.g., ODU 11/12). An explorer and probe are also needed, so a similar hybrid instrument that combines both (e.g., EXPRO, this time combining a shepherd’s hook with a UNC 12-mm marking probe) can be included.
The instruments included in the SRP cassette that are necessary for treatment of every patient can also be streamlined based on those used most frequently for all patients, such as an SH6/H7 anterior scaler and the 204S. However, the dental hygienist is selecting more useful, innovative posterior sickle scaler designs for the SRP cassette (e.g., Savannah 3 [Brasseler USA], Nevi® 3 [Hu-Friedy], or Montana Jack® [PDT]) (Figure 10). For Gracey curettes, only those that are actually used (e.g., Gracey 1/2, mesial, distal, Gracey 11/12, Gracey 13/14) should be included; the Gracey 7/8, which is used less frequently, can be removed. Additionally, the 100 slim ultrasonic insert can be removed because SRP patients are more difficult to treat and will likely require a more robust instrument, like the triple bend. The triple bend’s tip is very narrow and thin and functions well with SRP patients.
The new, simplified SRP cassette (Figure 11), which contains three fewer instruments, carries a reduced cost of approximately $473 compared to the original $700. With a 25% discount, the final cost is approximately $355 per SRP treatment cassette, which is more financially manageable.
Concluding Recommendations
As dental hygienists begin simplifying and updating the instrumentation necessary for their recare/maintenance and SRP treatment cassettes, important considerations include their choice of instrumentation provider, the company’s history and length of time in business, reputation in terms of quality products, and whether the company is an ISO-certified medical device company. Additionally, scrutinizing where the instruments are manufactured and assembled (i.e., United States or overseas), the metallurgy composition of the instrument tip and the metallurgy claim, and the company’s product warranty period can also help determine which products will best meet the practice’s needs. Comparing the cost of individual instruments across providers is also beneficial, though emphasis should be placed on selecting high-quality instruments that are critical to achieving successful treatment outcomes.
REFERENCES
1. Hohlfeld M, Wachtel HC. Instrumentation for periodontal treatment. Parodontol. 1990;1(3):230-248.
2. Zimmer SE. Instrument sharpening—sickle scalers and curettes. Dent Hyg (Chic). 1978;52(1):21-24.
3. Matsui K, Onaka K. Assessing significance of sharpening brand-new scaler. Bull Tokyo Dent Coll. 2013;54(1):1-8.
4. Migliario M, Franchignoni M, Soldati L, et al. Ergonomic analysis of the handle of manual instruments for dental hygiene. G Ital Med Lav Ergonj. 2012;34(2):202-206.
5. EverEdge 2.0. Hu-Friedy website. www.hu-friedy.com/TheUnocoatedTruth#Science. Accessed March 13, 2017.
6. The PDT Difference. Paradise Dental Technologies website. www.pdtdental.com/the-pdt-difference/. Accessed March 13, 2017.
7. Krishna R, De Stefano JA. Ultrasonic vs. hand instrumentation in periodontal therapy: clinical outcomes. Periodontol 2000. 2016;71(1):113-127.
8. Cobb CM. Clinical significance of non-surgical periodontal therapy: an evidence-based perspective of scaling and root planing. J Clin Periodontol. 2002;29 suppl 2:6-16.
9. Solis Mereno C, Santos A, Nart J, et al. Evaluation of root surface microtopography following the use of four instrumentation systems by confocal microscopy and scanning electron microscopy: an in vitro study. J Periodontal Res. 2012;47(5):608-615.