Digitally Designed Ovate Pontic as a Predictable Procedure to Improve Accuracy, Hygiene, Esthetics
Zev Kaufman, DDS; and Klenise S. Paranhos, DDS, MS
Abstract: The implant-retained fixed partial denture, or bridge, is a highly efficient restorative modality. The primary challenge with this restoration, however, lies in achieving the optimal design of the pontic, which needs to be esthetic, comfortable, and easily cleansable by the patient, a factor that can directly enhance prosthesis longevity. An ovate design is desirable for the pontic area. The simplest, most efficient approach to producing an ovate pontic is to do so at the time of tooth extraction. However, usually the clinician is presented with a well-healed, rounded ridge that requires additional modification in order to create a proper ovate pontic. This article describes a simplified protocol for digital and surgical fabrication of a highly hygienic, esthetic implant bridge pontic. Using a digital design workflow, a provisional restoration is fabricated in the laboratory to ideal contours. This provisional is then utilized for a simple surgical procedure to create predictable hard- and soft-tissue contours for the pontic area. The protocol produces an extremely resilient tissue around the pontic, which also translates to an enhanced esthetic, hygienic, and functional design.
The primary goal of fixed prosthodontics is replacement of missing teeth with a fixed, immovable, hygienically cleansable prosthesis. Prior to the common use of single, standalone implant restorations, a missing tooth or teeth was typically replaced using a conventional fixed partial denture (FPD), commonly referred to as a bridge. But even as the use of implants has become increasingly prevalent in the past 40 years, clinicians and researchers have noted that a tooth-by-tooth replacement is not always necessary and can present difficulties in design, fabrication, hygiene, and cost. In many situations, the use of a fixed partial prosthesis (ie, bridge) supported by implants is not only a more economical way to restore the patient to proper form and function, but may be the more hygienic and comfortable restorative solution for the patient.1 One simple question, however, persists: What is the optimal design for the pontic area that will maximize hygiene and comfort?
Pontic Design
While there are numerous types of pontic designs, most clinicians and laboratory technicians have been trained in five main designs, depicted in Table 1. As esthetic demands have increased over time, the use of an ovate pontic has become more predominant, especially in critically esthetic areas. The assertion has been made that a properly placed implant and a pontic next to it can yield a more esthetic result then two adjacent implants.1 Yet the use of an ovate pontic requires proper understanding of prosthodontics, surgery, and laboratory procedure. In addition, the communication between the clinician and laboratory technician regarding the shape and depth of the pontic is crucial, as both parties must be in unison regarding the case.1 As with any procedure, the greater the complexity, the greater the challenge to perform it.
The simplest way of producing an ovate pontic is to do so at the time of tooth extraction.2 This approach, however, does require careful coordination involving the extraction of the tooth and the fabrication of the ovate pontic. It necessitates the cooperation of the surgeon with the restorative dentist, unless one clinician performs both procedures. Either way, it is a time-consuming technique, requiring the time commitment for both the surgical extraction portion of the procedure as well as the prosthetic portion. Regardless, most often dentists are presented not with a fresh extraction site, but with a rounded, well-healed ridge that entails much more work to create a proper ovate pontic (Figure 1).
Digital dentistry has revolutionized treatment planning and has afforded considerable time savings surgically and prosthetically. This article demonstrates proper ovate pontic design and its communication to the laboratory side using a digital workflow that results in a comfortable, hygienic, esthetic restoration achieved in an efficient, economical manner.3
Case Presentation
A 65-year-old woman with no contributory medical history was referred by her general dentist for the restoration of the mandibular right quadrant with an implant-supported fixed restoration. Using 3D planning and a surgical guide, implants Nos. 29 and 31 were placed. After a healing period of 8 weeks, as recommended by the manufacturer, the two implants were ready for restoration (Figure 1 and Figure 2).
A recommended optical scanning procedure was followed.3-6 Scan bodies were connected, and the area was scanned (Figure 3); also, an interocclusal record was obtained and the opposing arch scanned. The restoration and pontic area were carefully digitally designed in the following manner: Mesiodistally, the pontic was extended as if tooth No. 30 was present and designed as an ideal cross-section of tooth No. 30 at the site. Buccolingually, the pontic was extended from the buccal aspect to the lingual aspect as if it was designed as a conventional ridge-lap design. The pontic was rounded and was extended 3 mm into the virtual ridge.
The delivery of the provisional is critical for the proper shape of the pontic area. Infiltration and crestal anesthesia are adequate. A try-in of the modified provisional confirmed the ovate design of the pontic and the fact that it exerted pressure on the tissue and could not be seated (Figure 4).
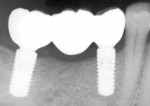
A full-thickness incision was made at the crest of the ridge, splitting the keratinized gingiva. A full-thickness flap was reflected buccally and lingually to allow exposure of the crestal bone. The polymethyl methacrylate (PMMA) provisional was then placed onto the implants, and the contact with the crestal bone was noted. Using a large #8 round diamond bur, the bone was contoured to fit 1 mm below the pontic surface to allow for appropriate soft-tissue thickness under the pontic after healing (Figure 5).7 The provisional was seated again (Figure 6) and verified with a radiograph (Figure 7). As the provisional was seated in place, the buccal and lingual soft tissues were retracted and left supported by the contours of the pontic.8
After a 2-week healing period, the patient was recalled for a postoperative visit, and excellent healing by secondary intention was noted. At this stage, the patient should be comfortable and functional with the provisional restoration as if it was the definitive restoration. Minor contour changes may be noted as the patient adjusts to the restoration.
In another month's time, soft-tissue maturation and bone stabilization will be noted. The patient, thus, is now ready to receive the final restoration. Once the provisional restoration is removed, the supported soft tissues will start to collapse immediately. Conventionally, the provisional is placed on the laboratory cast, and a soft-tissue spacer matrix is applied in order to register the emergence profile and the pontic contours.9 To demonstrate the difference, scanning of those tissues after removal of the provisional was performed (Figure 8), and the provisional was physically indexed on the cast and the cast was scanned (Figure 9). In these two images, note the remarkable difference between the scanned, unsupported tissues versus the tissue matrix physically transferred to the cast by using the provisional in a conventional manner.
The conventional procedure as described above is time-consuming. The chairside digital scanner, however, allows the clinician to shorten the procedure and easily transfer all the information directly to the laboratory. Once tissue healing is complete and minor contour changes to the provisional are noted and performed, all that is required is removal of the provisional and scanning it with the intraoral scanner. Technically, one side of the provisional is held with college pliers and the provisional is scanned. The scanned portion is then outlined on the screen with the lock-protect scan tool and the provisional is then grabbed on the other side to allow the rescanning of the side that was held originally. The provisional is then re-placed into position, and the patient will return to receive the final restoration once it is completed.10,11
Since the original scan has already been verified with the provisional, there is no need to repeat the scan or to index the tissue side of the provisional. In the present case, strictly for the sake of demonstration, a redundant scan was performed to show the tissue development as well as the discrepancy between simply scanning the tissue versus scanning the modified provisional as it is designed to support that tissue properly.
Results
This technique results in a restoration that is both esthetic and highly hygienic,11,12 because the partially keratinized tissue under the pontic (Figure 10) essentially attaches itself to the smooth surface of the ceramic or zirconia restoration11-14 and food impaction is prevented.12-15 However, if plaque and debris does get under the pontic, it can be readily removed using floss, which can be introduced through the interproximal papillary area and swept from out under the pontic. Functionally, to the patient's tongue, the papillae mesially and distally to the pontic feel like natural papillae. They prevent food impaction between the teeth, which is a common complaint with posterior tooth-by-tooth replacement restorations, which also typically possess a flat ridge lacking the characteristic soft-tissue scallop of a natural dentition.
Esthetically, this procedure creates a band of keratinized tissue to the buccal and lingual aspects of the pontic (Figure 10), creating a much more lifelike final restoration. There is no period of accommodation to the final restoration because it is an exact duplicate of the provisional (Figure 11 through Figure 13). In addition, upon recall, as in the present case, typical gingival marginal plaque was noted around the provisional, yet the pontic area was remarkably clean and shiny (Figure 11).
Discussion
The development of digital dental technology has improved precision, accuracy, esthetics, and efficiency of dental procedures.6 In addition, digital applications have increased the ease of sharing and processing patient imaging data. 3D technology with digital scanning and CAD/CAM can be used to produce an ovate pontic in a predictable manner and achieve a satisfying treatment outcome, especially in significantly impaired patients. Conversely, traditional methods of prosthetic treatment are lengthier, require more chairtime, and allow more chance for error.10,11
Additionally, traditional impressions are subject to dimensional distortion at multiple points between impression-taking and model pour-up, and bacterial-viral cross-contamination to the laboratory technician can be an issue. 3D technologies have made digital impression-taking faster, easier, and very accurate. Visualization of imaging data allows for better understanding of treatment outcomes while enabling a more hands-on approach to prosthetic design-both of which contribute greatly toward accuracy and precision of the treatment result. Finally, sending impressions digitally eliminates the time for transport of physical impressions and allows the lab to fabricate a prosthesis immediately. It also not only reduces the potential of cross-contamination to laboratory technicians, but eliminates it altogether.
The technique demonstrated in this article is designed to work in all pontic area cases in differential degrees and levels, because the technique is especially aimed at improving oral hygiene. In general, if a patient cannot properly clean the prosthesis, a case will have no long-term success. A design modification, such as this one, that can positively affect the long-term success of a prosthesis is beneficial.
There may be a perception that this technique could not work in narrow resorbed ridges because of a limited amount of pontic area width with which to work. However, on the contrary, this is actually a highly suitable application for this technique. Resorbed, narrow ridges typically have a thin band of keratinized gingiva spanning the top of the ridge. After a full-thickness crestal incision and reflection of a minor full-thickness flap buccolingually, the narrow ridge is exposed. This narrow ridge can then readily be reduced to accommodate the proper contours of the ovate pontic. The flaps are then allowed to approximate the contours and are left without suturing for proper secondary intention healing. Within 2 weeks, excellent healing of the tissues can be expected and the physical parameters of the pontic area improved.
It is important to re-emphasize that in resorbed ridges this procedure is not meant to improve esthetics. It is performed strictly to improve hygiene and biological tissue response. Regardless of location, whether in the dental arch or apicogingivally, an ovate tissue pontic area will create a superior environment for oral hygiene as well as excellent keratinized tissue and gingival response.
This method is also beneficial economically considering that the procedure requires only a simple crestal incision, and the rest of the protocol is done digitally, rather than by traditional means. A digital impression can be made at any stage, be it at implant placement, at implant uncovering, or following implant integration. A digitally designed and fabricated provisional restoration with a properly designed ovate pontic can be delivered with a simple pontic area surgical procedure.
A secondary benefit is that the PMMA provisional is used not only to produce soft- and hard-tissue contours but also to verify fit prior to fabrication of the final zirconia restoration. In addition, chairtime is considerably reduced because the proper contour of the pontic is designed and fabricated prior to working with the patient.
Regardless of the clinician's level of experience and expertise, this method can result in a superior outcome, is more convenient and cost effective, and saves considerable chairtime compared to conventional techniques.
Conclusion
This technique can be incorporated into any type of restorative procedure that includes pontic areas, be it a single pontic or a full-arch restoration. The surgical procedure can be performed by either the surgeon or the restorative dentist since it does not require major prosthodontic chairtime, and rather than attempting to modify the restoration to the physiological conditions in the mouth, the restoration is prepared in the laboratory to ideal contours and the oral anatomy is adjusted to it. The result is a superior restoration that is hygienic because it prevents food impaction underneath the pontic. Cleansability and maintenance are also enhanced. This approach creates a much more resilient tissue around the pontic, which translates to a more esthetic and comfortable result and should lead to high patient satisfaction.
About the Authors
Zev Kaufman, DDS
Clinical Assistant Professor, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Private Practice limited to Prosthodontics and Implant Surgery, New York, New York
Klenise S. Paranhos, DDS, MS
Clinical Assistant Professor/Assistant Group Practice Director, Department of Cariology and Comprehensive Care, NewYork University College of Dentistry, New York, New York; Diplomate, International Congress of Oral Implantologists; Private Practice, Chappaqua, New York
References
1. Dylina TJ. Contour determination for ovate pontics. JProsthetDent. 1999;82(2):136-142.
2. Bakshi M, Tarnow D, Bittner N. Changes in ridge dimension with pontics immediately placed at extraction sites: a pilot study. Int J PeriodonticsRestorative Dent. 2018;38(4):541-547.
3. Oberoi G, Nitsch S, Edelmayer M, et al. 3D printing - encompassing the facets of dentistry. Front Bioeng Biotechnol. 2018;6:172.
4. Alharbi N, Osman RB, Wismeijer D. Factors influencing the dimensional accuracy of 3D-printed full-coverage dental restorations using stereolithography technology. Int J Prosthodont. 2016;29(5):503-510.
5. Yang Y, Cui FJ, Liu XQ, et al. Effect of provisional restorations with ovate pontics on preservation of the ridge after tooth extraction: case series. Chin J Dent Res. 2019;22(3):181-188.
6. Lee JH, Lee CH. Completely digital approach to an ovate pontic. J Prosthet Dent.2016;115(6):792-794.
7. Narayan SJ, Singh PK, Devarhubli AR, Keerthi R. Soft tissue development around pontic site: a case series. J Indian Prosthodont Soc. 2016;16(3):298-302.
8. Guruprasada. Creating natural gingival profiles of missing anterior teeth using ovate pontic. Med J Armed Forces India. 2015;71(suppl 1):
S124-S126.
9. Jambhekar SS, Kheur MG, Matani J, Sethi S. Easy accurate transfer of the sculpted soft tissue contours to the working cast: a clinical tip. JIndianProsthodontSoc. 2014;14(suppl 1):337-340.
10. Raigrodski AJ, Schwedhelm ER, Chen YW. A simplified technique for recording an implant-supported ovate pontic site in the esthetic zone. JProsthetDent. 2014;111(2):154-158.
11. McArdle BF. Creating natural gingival profiles using the ovate pontic technique. Dent Today. 2004;23(7):97-101.
12. Schield HW. The influence of bridge pontics on oral health. J Mich State Dent Assoc. 1968;50(4):143-147.
13. Cavazos E Jr. Tissue response to fixed partial denture pontics. JProsthetDent. 1968;20(2):143-153.
14. Silness J, Gustavsen F, Mangersnes K. The relationship between pontic hygiene and mucosal inflammation in fixed bridge recipients. JPeriodontalRes. 1982;17(4):434-439.
15. Tolboe H, Isidor F, Budtz-Jörgensen E, Kaaber S. Influence of oral hygiene on the mucosal conditions beneath bridge pontics. Scand J DentRes. 1987;95(6):475-482.