Management of Recurrent Gummy Smile After 7 Years: A Case Report
Yu-Ting Yeh, DDS, MSD; and Steven B. Blanchard, DDS, MS
Abstract: Esthetic crown lengthening is a periodontal surgical procedure to correct excess gingival display (ie, "gummy smile"). The procedure may require soft-tissue excision only, osseous resection, or a combination of both. However, the long-term healing responses, such as soft-tissue relapse or recession and hard-tissue regrowth and resorption, have not been fully reported in the literature. This case report describes the management of a patient with esthetic concerns about a gummy smile. The patient stated that the maxillary anterior area had been previously treated with periodontal surgery 7 years earlier but the condition had slowly recurred over time. The authors highlight the possible reasons for the recurrence and the keys to successfully managing the case.
Esthetic crown lengthening (ECL) is a periodontal surgical procedure to correct excess gingival display (ie, "gummy smile") that can require soft-tissue excision only, osseous resection, or a combination of both.1 Different soft- and hard-tissue healing patterns after ECL procedures have been reported.2-5
After surgical crown lengthening, some soft-tissue rebound is to be expected within the first 6 months before tissue stability is fully established due to the restoration of the dimensions of the supracrestal tissue attachment (SCTA). Brägger et al observed that 2.5% of sites receiving functional crown lengthening surgery showed that the gingival margin shifted 1 mm coronally from baseline to 6 weeks, and 33% of the sites demonstrated coronally displacement of gingival margin from 6 weeks to 6 months postsurgically.2 Deas and colleagues demonstrated that the position of the sutured gingival margin relative to the bone crest affects the amount of tissue rebound and that the closer the flap margin is placed relative to the alveolar crest, the greater the tissue rebound is expected.3 Wilderman et al studied the human histological response of bone after osseous surgery and found that 1 year after osseous resection, there was a mean of 0.8 mm bone resorption.4 On the other hand, a 45-day study on dogs by De Sanctis et al showed an average of 0.24 mm bone gain after osseous resection.5
While these different short-term healing responses, including soft-tissue relapse or recession and hard-tissue regrowth or resorption, have been documented, there appears to be limited information available on long-term tissue relapse following ECL procedures. The aim of this case report is to describe the management of a patient with recurrent excess gingival display after an ECL procedure performed 7 years earlier.
Case Report
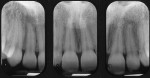
A 25-year-old African American female patient first presented to Indiana University School of Dentistry Graduate Periodontics Clinic in December 2010 for assessment of her chief complaint that, "I don't like how much my gums show when I smile." The patient was a nonsmoker, systemically healthy, and taking no medications. Clinically, there was excessive gingival display of maxillary teeth with approximately 6 mm to 8 mm of keratinized tissue on the facial aspect of teeth Nos. 6 through 11 (Figure 1 and Figure 2). The probing depths were 1 mm to 3 mm, and radiographic interdental bone levels were at the level of the adjacent cementoenamel junctions (CEJs) (Figure 3). After discussion with the patient about treatment options, the patient agreed to proceed with ECL surgery.
For the initial ECL procedure, a submarginal incision approximately 1 mm to 2 mm away from the gingival margin was made from teeth Nos. 6 through 11 as determined by a customized surgical template. After mucoperiosteal flap reflection, the bone level of teeth Nos. 6 through 11 was at the level of the CEJs (Coslet type 1B case6) (Figure 4). Ostectomy and osteoplasty were done until the crestal bone level was approximately 2 mm apical to the CEJs (Figure 5). The flap was sutured at the level of the CEJs (Figure 6).
After the surgery, the patient was advised to use nonsteroidal anti-inflammatory drugs for postsurgical discomfort and rinse with a chlorhexidine mouthrinse. Healing at 1 week was good with mild papillary inflammation, and sutures were removed (Figure 7 and Figure 8). The patient neglected to return for subsequent follow-up visits and was lost for additional follow-up.
Seven years later (August 2017), the patient returned to the Graduate Periodontics Clinic for evaluation stating that she wanted "to have the gum surgery again." This time, the patient was seen by a different clinician (YTY). The patient's clinical presentation showed relapse of the gingival tissue among the maxillary anterior teeth, reverting toward her initial presentation in 2010 (Figure 9); otherwise, the rest of the teeth presented in good clinical gingival health. With an exaggerated smile, the patient displayed 6 mm to 7 mm of gingiva from the lower border of the lip to the CEJ of the anterior teeth. Based on the vertical maxillary excess classification on gingival and mucosal display by Garber and Salama,7 this was a degree II case for which the combination of periodontal surgery and orthognathic surgery would be indicated to correct the excessive gingival display.
Treatment options were discussed with the patient and included the initial ECL procedure with the intention of showing the original anatomic crown length and shape of the teeth and subsequent orthognathic treatment to correct the length of the maxilla gingiva. After the clinician demonstrated to the patient a diagnostic wax-up (Figure 10) and clinical mock-up that restored the original anatomic crown length with a coronal gingival tissue removal of 2 mm, the patient was satisfied with the tooth-gingiva display and, thus, was only interested in a revision of the ECL procedure. She refused to receive orthodontic therapy and subsequent orthognathic treatment after the ECL procedure considering the potential surgical complications and longer healing time.
After flap reflection, an additional 2 mm of radicular bone was removed, as the diagnostic wax-up (Figure 10) and clinical mock-up, as previously alluded to, had revealed that an additional 2 mm of tooth exposure was required for optimal tooth dimensions (Figure 11 and Figure 12). The flap was positioned at the level of the CEJs and sutured using simple interrupted 4-0 Vicryl® sutures (Ethicon, Johnson & Johnson, jnjmedicaldevices.com) (Figure 13).
At 1 week, the patient reported only mild postsurgical discomfort. There was minimal inflammation with slight erythema of the interdental papillae of teeth Nos. 6 through 11. Three months after the surgery, the gingiva was healthy and the gingival margin was at the CEJs of teeth Nos. 6 through 11, which allowed clinical display of proper tooth length (Figure 14 and Figure 15). The patient was satisfied with the improved esthetic outcome during smiling.
Discussion
Several possible patient- and surgery-related factors likely led to the patient's relapse after the initial surgery. The most probable reason for relapse was insufficient bone removal at the initial surgery. At the second surgery in 2017 additional bone removal was completed to rectify this (Figure 5 and Figure 12). While Gargiulo et al described the average dimension of the dentogingival junction (now termed SCTA based on the American Academy of Periodontology/European Federation of Periodontology 2017 classification8) to be 2.04 mm,9 other studies found a wide range of SCTA dimensions between 0.75 mm and 4.33 mm in cadavers and 0.5 mm and 3.5 mm in patients.10,11
The created distance of 2 mm between the CEJ and bone crest may have been an insufficient dimension for the SCTA for this patient resulting in soft-tissue rebound. Given the relapse noted 7 years later, it was decided that an additional 2 mm of bone removal was required since an additional 2 mm of tooth exposure was needed for optimal esthetics. The additional bone reduction helped to re-establish the normal SCTA for this patient, reducing the potential for future soft-tissue rebound. It is the authors' philosophy that the dimensions of the SCTA are predetermined and the amount of bone reduction (ostectomy) needed for most cases of ECL (given no planned alteration of the incisal edges of the teeth) should equal the amount of additional tooth length exposure desired to accommodate the dimension of the SCTA and to minimize risk of relapse.12
Another possible surgery-related factor in this case might have been that the thick marginal bone was not sufficiently reduced at the time of the initial surgery. In a cadaver study, on average, the buccal plate thickness over the maxillary arch ranged from 1.6 mm in the anterior region to 2.2 mm in the posterior.13 In other studies, the thickness of buccal bone was associated with overlying gingiva tissue thickness; this might be because of greater blood supply to the gingival tissue.14,15 During the second surgical procedure in this case, the buccal bone was thinned on the facial and interdental areas for better soft-tissue adaptation, and this helped reduce the thickness of the gingival tissue.
The patient's tissue phenotype also may have played a role in the relapse. Pontoriero and Carnevale reported that patients with thick gingival phenotype demonstrated more coronal shift of gingival tissue compared to thin phenotype after surgical crown lengthening.16 They reported that the average relapse of the soft tissue was 1.2 mm 1 year postsurgery and patients with thicker tissue tended to have an additional 0.5 mm of soft-tissue relapse. Arora et al also observed that the mean tissue regrowth in patients with a thick-flat gingival architecture was significantly greater than in those with a thin-scalloped type.17
Several keys can be attributed to the successful management of a case like this one. First, during the presurgical evaluation, bone sounding can help identify bone crest position. The treatment options of gingivectomy or apically positioned flap alone or in combination with osseous surgery would be based on the bone margin to CEJ or the future crown margin. If it is less than 3 mm, osseous surgery will be necessary. Second, the surgical template fabricated based on the diagnostic wax-up can help determine the initial incision position to expose the ideal tooth contour. Third, after gingivectomy and flap reflection, the amount of bone reduction (ostectomy) should equal the amount of additional tooth length exposure desired to accommodate the dimension of the SCTA to minimize risk of relapse.
Conclusion
Preoperative evaluation of the periodontal phenotype and dimensions of the supracrestal tissue attachment along with sufficient identification of the etiologies of excessive gingival display are keys to successful management of a recurrent gummy smile. The dimensions of the supracrestal tissue attachment are likely to be predetermined and, given no planned alteration of the position of the incisal edges, the amount of bone reduction (ostectomy) should equal the amount of additional tooth exposure that is desired to accommodate dimensions for SCTA to minimize relapse.
Acknowledgment
The authors thank Samira Toloue, DDS, MSD, and Meenarin Panittaveekul, DDS, MSD, for their expertise and assistance throughout the documentation of this case report.
About the Authors
Yu-Ting Yeh, DDS, MSD
Assistant Professor, Department of Periodontology, Creighton University School of Dentistry, Omaha, Nebraska
Steven B. Blanchard, DDS, MS
Professor, Department of Periodontology, Indiana University School of Dentistry, Indianapolis, Indiana
References
1. Ong M, Tseng SC, Wang HL. Crown lengthening revisited. Clin Adv Periodontics. 2011;1(3):233-239.
2. Brägger U, Lauchenauer D, Lang NP. Surgical lengthening of the clinical crown. J Clin Periodontol.1992;19(1):58-63.
3. Deas DE, Moritz AJ, McDonnell HT, et al. Osseous surgery for crown lengthening: a 6-month clinical study. J Periodontol. 2004;75(9):1288-1294.
4. Wilderman MN, Pennel BM, King K, Barron JM. Histogenesis of repair following osseous surgery. J Periodontol. 1970;41(10):551-565.
5. De Sanctis M, Cortellini P, Clauser C, Pini Prato GP. Coronal displacement of the junctional epithelium and attachment gain following apically positioned flap with bone resective surgery in dogs. Int J Periodontics Restorative Dent. 1988;8(4):64-76.
6. Coslet JG, Vanarsdall R, Weisgold A. Diagnosis and classification of delayed passive eruption of the dentogingival junction in the adult. Alpha Omegan. 1977;70(3):24-28.
7. Garber DA, Salama MA. The aesthetic smile: diagnosis and treatment. Periodontol 2000. 1996;11:18-28.
8. Jepsen S, Caton JG, Albandar JM, et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89 suppl 1:S237-S248.
9. Gargiulo AW, Wentz FM, Orban B. Dimensions and relations of the dentogingival junction in humans. J Periodontol. 1961;32(3):261-267.
10. Vacek JS, Gher ME, Assad DA, et al. The dimensions of the human dentogingival junction. Int J Periodontics Restorative Dent. 1994;14(2):154-165.
11. Hamasni FM, El Hajj F. Comparison of the clinical biological width with the published standard histologic mean values. J Int Soc Prev Community Dent. 2017;7(5):264-271.
12. Smukler H, Chaibi M. Periodontal and dental considerations in clinical crown extension: a rational basis for treatment. Int J Periodontics Restorative Dent. 1997;17(5):464-477.
13. Katranji A, Misch K, Wang HL. Cortical bone thickness in dentate and edentulous human cadavers. J Periodontol. 2007;78(5):874-878.
14. Fu JH, Yeh CY, Chan HL, et al. Tissue biotype and its relation to the underlying bone morphology. J Periodontol. 2010;81(4):569-574.
15. Kennedy JE. Effect of inflammation on collateral circulation of the gingiva. J Periodontal Res. 1974;9(3):147-152.
16. Pontoriero R, Carnevale G. Surgical crown lengthening: a 12-month clinical wound healing study. J Periodontol. 2001;72(7):841-848.
17. Arora R, Narula SC, Sharma RK, Tewari S. Evaluation of supracrestal gingival tissue after surgical crown lengthening: a 6-month clinical study. J Periodontol. 2013;84(7):934-940.