Accuracy of Cone-Beam Computed Tomography Versus Periapical Radiography Measurements When Planning Placement of Implants in the Posterior Maxilla: A Retrospective Study
Takahito Kakumoto, DDS; Adam Barsoum, BDS, DMD; and Stuart J. Froum, DDS
ABSTRACT
Intraoral periapical (PA) radiography is commonly used for measuring the remaining crestal bone height when implants are treatment planned in the maxillary posterior region. A major drawback of conventional radiographs is that a 3-dimensional (3D) entity is compressed and superimposed on itself into a 2-dimensional (2D) image, which is often distorted. Conversely, 3D information can be extracted from computerized tomography. The purpose of this article is to evaluate and discuss limitations of intraoral PA radiography for the measurement of posterior maxillary alveolar bone height and describe the use of information obtained by means of 3D computerized tomography to help plan implant placement. Method: Clinical data in this study was obtained from the Implant Database (ID) at New York University College of Dentistry (NYUCD). The data set was extracted as de-identified information from the routine treatment of patients at the Ashman Department of Periodontology and Implant Dentistry at NYUCD. The ID is certified by the Office of Quality Assurance at NYUCD. This study is in compliance with the Health Insurance Portability and Accountability Act (HIPAA) requirements. Thirty-five sites were compared with both PA and cone-beam computed tomography (CBCT) images of the posterior region, including the anatomical relationship of the maxillary crest to the sinus floor. The values recorded from the CBCT were used as the standard to which PA was subtracted from. Results: Linear differences were consistently seen in which the remaining maxillary posterior crestal bone height appeared larger or smaller on the PA radiographs when compared to the measurements made of the same area on the CBCT images.Conclusion: CBCT imaging is a valuable adjunct in radio-anatomical and radio-diagnostic observations in the posterior maxillary region. Furthermore, in this study CBCT measurements were shown to be more accurate in assessing the remaining crestal ridge height apical to the sinus membrane when compared to PA radiographs. More research is necessary to verify these findings.
Intraoral periapical (PA) radiography is the primary diagnostic and most commonly used method for measuring the remaining crestal bone height while screening for implant treatment in the posterior maxillary area.1A significant drawback of conventional PA radiographs, however, is that 3-dimensional (3D) objects (eg, tooth or ridge) are compressed and superimposed into 2-dimensional (2D) images that are often distorted. While cone-beam computed tomography (CBCT) can be used to avoid this problem, not every patient in need of dental implants requires CBCT scan imaging. If the implant site is distant from critical anatomical structures and the alveolar ridge is of adequate buccolingual width and height, conventional intraoral radiographs usually are sufficient to assess the site for implant placement.2 Moreover, if they yield accurate measurements, the use of PA radiographs to assess alveolar ridge height can minimize cost and reduce radiation exposure compared with CBCT scans. However, a consensus of the American Academy of Oral and Maxillofacial Radiology (AAOMR) concluded, "For the preoperative diagnostic phase, the AAOMR reaffirms that cross-sectional imaging be used for implant site assessment. Furthermore, the AAOMR recommends CBCT imaging as the current method of choice for cross-sectional imaging in that it provides the greatest diagnostic yield at an acceptable radiation dose risk."3
Historically, the use of periapical radiographs, calibrated panoramic radiographs, and bone sounding has provided acceptable information to allow for treatment planning and implant placement.4 To evaluate the discrepancy between the radiographic and true bone dimensions a periodontal probe, mechanical calipers, CBCT, and periapical radiographs can be useful. Larheim et al reported that from a clinical point of view the mean difference between periapical radiographic measurements for tooth lengths before extraction and real lengths measured with calipers after extraction was not significant. Their study reported that in 95% of cases the actual alveolar ridge height was approximately the observed radiographic height ±1 mm.5 Another study measured implant length using mechanical calipers, CT scans, panoramic radiographs, linear tomograms, and PAs at variable vertical angulations. The findings demonstrated that at a 90-degree angulation the measurement error of PAs was 0.3 mm to 0.6 mm, which was similar to the CT measurement error of 0.2 mm to 0.8 mm.6
More recently, however, the introduction of CBCT to determine measurements has caused a paradigm shift in examination, treatment planning, and surgeries in implant dentistry.7 Cross-sectional imaging offers segmental viewing of the alveolar ridge and exploration of an individual's anatomy, enabling high predictability and success rates in the placement of implants. The purpose of this retrospective study was to compare periapical radiography to CBCT scans for the measurement of alveolar ridge height in edentulous posterior maxillary areas.
Materials and Methods
Clinical data for this study was obtained from the Implant Database (ID) at New York University College of Dentistry (NYUCD). The data set was extracted as de-identified information from the routine treatment of patients at the Ashman Department of Periodontology and Implant Dentistry at NYUCD. The ID is certified by the Office of Quality Assurance at NYUCD, and this study is in compliance with the Health Insurance Portability and Accountability Act (HIPAA) requirements. Twenty patients with 35 sites in total that had combined periapical and CBCT images of the posterior maxilla were selected from the database for analysis of the distance from the alveolar crest to the sinus floor. Two examiners independently evaluated the cross-sectional images.
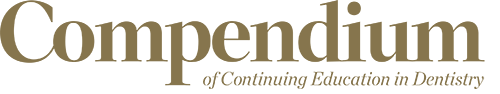
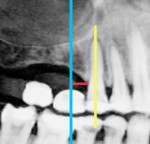
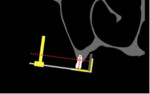
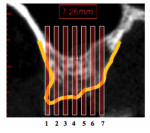
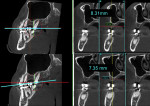
The distance from the crest of the ridge to the floor of the maxillary sinus was measured at the same distance from the mesial or distal of the natural tooth or implant adjacent to the selected edentulous ridge. Using the same distance from an adjacent tooth or implant allowed precise site orientation with both imaging systems. CBCTs were measured with Simplant® software version 18.0 (Dentsply Sirona, dentsplysirona.com), and PAs were measured with MiPACS® software v.3.1.1404 (Medicor Imaging, medicorimaging.com). CBCT scan measurements were recorded on the cross-sectional view. A straight line perpendicular to a tangent at the crest of the ridge was extended to the floor of the maxillary sinus. The length of the line was measured and used as the CBCT ridge height (Figure 1 and Figure 2). Periapical measurements of the same area were recorded by extending a straight line parallel to the long axis of the adjacent natural tooth or implant from the alveolar crest to the floor of the maxillary sinus. The length of the line was measured and recorded as the PA ridge height (Figure 3).
Two examiners (AB and TK) recorded the measurements, performing them independently of each other. Each examiner measured the CBCT scan images and digital PA images. To control for inter-examiner variability, both sets of measurements on both radiographic systems were averaged. To minimize intra-examiner and inter-examiner variability, the examiners were calibrated in both radiographic imaging systems to recognize and agree on what they would identify as the floor of the maxillary sinus. Both examiners independently re-evaluated the images until agreement was reached.
Results
Differences in measurements were consistently seen when the remaining crestal height was measured on PA radiographs and CBCT images. Results from the sites are listed in Table 1. When the threshold was set to 1 mm, the discrepancy observed was 34% in 12 sites. PA radiographs overestimated the measurements 66% of the time in 23 sites. The average discrepancy was 0.75 mm, and discrepancies ranged from -1.69 mm to +2.1 mm when PA minus CBCT distance measurements were calculated.
Discussion
As dental implants have emerged as a popular treatment option for replacement of missing teeth, the availability and acquisition of CBCT machines in private practice has increased.8 An estimated 20 million teeth are extracted in the United States each year, with 40% of the population over 60 years of age having one or more edentulous sites.9 Thus, the need to optimize treatment planning is essential for the continued evolution of treatment techniques.
Following tooth extraction or loss, the posterior maxilla is susceptible to vertical bone loss from sinus pneumatization and/or alveolar ridge resorption; oftentimes sinus augmentation is required.10 Accurate measurement of the residual ridge height during implant treatment planning in the posterior maxilla is critical, as precise control of the length of the osteotomy is vital to avoid inadvertent sinus complications following sinus perforation. Such complications may include sinusitis, nasal bleeding, nasal obstruction, nasal secretion, headache, pain or tenderness in the sinus region, and decreased sense of smell.11,12
Inaccuracy of Periapical Radiographs
In the past, to obtain PA radiographs clinicians often used the bisecting technique in which the central ray was directed at a line bisecting the long axis of both the tooth and film holder. Currently, the paralleling technique is popular because it provides inherently less distortion and greater accuracy in measurement than the bisecting technique.13 This is especially critical in the field of endodontics for root length determination. However, this characteristic is not applicable in implant dentistry because there is an absence of key identifiers or measurement points such as incisal edge or root apex (Figure 4 and Figure 5), making it difficult to measure the ridge height and eliminating any repeatability in measurements, and, thus, introducing error.
Similarly, when a tooth is extracted, the operator may insert the x-ray sensor erroneously, and oftentimes the remaining teeth and alveolar ridge may have a dissimilar long axis (Figure 6 through Figure 8), preventing the operator from attaining true parallelism for accurate use of the measurement tool.
In addition, to accommodate patient comfort, oftentimes periapical films are bent or crimped when they are positioned intraorally. However, this is not the case in disarticulated mandibles that often are used in research studies and which lack soft tissue, muscular activation, and patient tolerance. Thus, the observations of PAs measured on cadavers should be regarded as difficult if not impossible to reproduce in live patients.6
While there is reported discrepancy between conventional film and sensor periapical radiography,14 this study relied solely on digital radiographs for periapical exposures.
Anatomical Considerations
A review by Sharan and Madjar discussed multiple variations of the shape of the maxillary sinus floor in relation to teeth roots.15 The shape of the floor may affect the prevalence of over- or underestimation on PA based on the degree of superimposition or lack thereof.
If the sinus extends between the roots in a triangular shape, this often creates insufficient radiolucency for detection on periapical radiographs, similar to incipient decay on buccal/lingual surfaces of teeth. This, therefore, can cause an overestimation when measuring the alveolar ridge height.
Also, alveolar ridge height may appear longer on a PA radiograph than in a cross-sectional image (Figure 9), as superimposition will show the height to be as high as the highest point of the ridge (see #1 in Figure 9). In reality, however, the area of interest for implant placement (see #4 in Figure 9) may have inadequate ridge height for conventional surgical placement.
Accuracy of CBCT
Voxel size of the CBCT should be considered to optimize the accuracy of the linear measurements. Although CBCT scans employing a larger voxel size offer lower radiation exposure, they are associated with decreased spatial resolution compared to CBCT scans with a smaller voxel size. This factor makes repeatability and reproducibility of measuring points more challenging.16,17 In the present study, the smallest available voxel size setting (0.2 mm) was used.
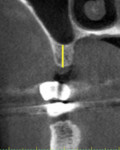
The orientation of reference plane settings also impacts linear measurements.18 This can be seen in Figure 10, which shows an example of different linear measurements obtained from a reference plane setting by +/- 12 degrees. In the present study, the reference plane setting was controlled to have the cross-sectional line parallel to the adjacent tooth as seen in Figure 1, Figure 2, and Figure 3.
To obtain measurements that are as accurate as possible the authors recommend always using cross-sectional imaging while treatment planning implant sites in the maxillary posterior region, following the manufacturer's recommendations for adjusting reference planes and panoramic curvature when used. Intraoperative PA radiographs should be captured using extension cone paralleling (XCP) to ensure proper long cone paralleling technique. After the initial osteotomy (2 mm twist drill) is performed, a direction indicator should be used to confirm positioning, and the radiographic measurement could confirm whether there is any distortion in the radiograph as the length of the indicator is predetermined from the implant manufacturer.
Conclusion
CBCT imaging is a valuable adjunct in radio-anatomical and radio-diagnostic observations in the posterior maxillary region. Furthermore, CBCT measurements were shown in the present study to be more accurate in assessing the remaining crestal ridge height apical to the sinus membrane when compared to PA radiographs. More research is necessary to verify the findings in this study.
Disclosure
The authors declared no conflicts of interest.
About the Authors
Takahito Kakumoto, DDS
Implant Resident, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York
Adam Barsoum, BDS, DMD
Implant Resident, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York
Stuart J. Froum, DDS
Clinical Adjunct Professor and Director of Clinical Research, Ashman Department of Periodontology and Implant Dentistry, New York University College of Dentistry, New York, New York; Private Practice New York, New York
References
1. Juodzbalys G, Kubilius M. Clinical and radiological classification of the jawbone anatomy in endosseous dental implant treatment. J Oral Maxillofac Res. 20131;4(2):e2.
2. Harris D, Horner K, Grondahl K, et al. E.A.O. guidelines for the use of diagnostic imaging in implant dentistry 2011. A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin Oral Implants Res. 2012;23(11):1243-1253.
3. Tyndall DA, Price JB, Tetradis S, et al. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113(6):817-826.
4. Flanagan D. A nonradiologic method for estimating bone volume for dental implant placement in the completely edentulous arch. J Oral Implantol. 2001;27(3):115-117.
5. Larheim TA, Eggen S. Determination of tooth length with a standardized paralleling technique and calibrated radiographic measuring film. Oral Surg Oral Med Oral Pathol. 1979;48(4):374-378.
6. Gher ME, Richardson AC. The accuracy of dental radiographic techniques used for evaluation of implant fixture placement. Int J Periodontics Restorative Dent. 1995;15(3):268-283.
7. Jaju PP, Jaju SP. Clinical utility of dental cone-beam computed tomography: current perspectives. Clin Cosmet Investig Dent. 2014;6:29-43.
8. Thomas SL. Application of cone-beam CT in the office setting. Dent Clin North Am. 2008;52(4):753-759.
9. Marcus SE, Drury TF, Brown LJ, Zion GR. Tooth retention and tooth loss in the permanent dentition of adults: United States, 1988-1991. J Dent Res. 1996;75(spec no):684-695.
10. Ariji Y, Kuroki T, Moriguchi S, et al. Age changes in the volume of the human maxillary sinus: a study using computed tomography. Dentomaxillofac Radiol. 1994;23(3):163-168.
11. Pjetursson BE, Rast C, Bragger U, et al. Maxillary sinus floor elevation using the (transalveolar) osteotome technique with or without grafting material. Part I: implant survival and patients' perception. Clin Oral Implants Res. 2009;20(7):667-676.
12. Ragucci GM, Elnayef B, Suárez-López Del Amo F, et al. Influence of exposing dental implants into the sinus cavity on survival and complications rate: a systematic review. Int J Implant Dent. 2019;5(1):6.
13. Forsberg J. Radiographic reproduction of endodontic "working length" comparing the paralleling and the bisecting-angle techniques. Oral Surg Oral Med Oral Pathol. 1987;64(3):353-360.
14. Kullendorff B, Petersson K, Rohlin M. Direct digital radiography for the detection of periapical bone lesions: a clinical study. Endod Dent Traumatol. 1997;13(4):183-189.
15. Sharan A, Madjar D. Correlation between maxillary sinus floor topography and related root position of posterior teeth using panoramic and cross-sectional computed tomography imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(3):375‐381.
16. Sherrard JF, Rossouw PE, Benson BW, et al. Accuracy and reliability of tooth and root lengths measured on cone-beam computed tomographs. Am J Orthod Dentofacial Orthop. 2010;137(4 suppl):S100-S108.
17. Maret D, Telmon N, Peters OA, et al. Effect of voxel size on the accuracy of 3D reconstructions with cone beam CT. Dentomaxillofac Radiol. 2012;41(8):649‐655.
18. Nikneshan S, Aval SH, Bakhshalian N, et al. Accuracy of linear measurement using cone-beam computed tomography at different reconstruction angles. Imaging Sci Dent. 2014;44(4):257-262.