Resin Bonding of a Lithium-Disilicate Crown Using a Ligated Rubber Dam: A 2-Year Case Report
Mario F. Romero, DDS; Jacqueline Delash, DMD, MPH; Roger M. Arce, DDS, MS, PhD; Courtney S. Babb, DMD; and William W. Brackett, DDS, MSD
Abstract: Enduring glass-ceramic restorations greatly depend on the quality of adhesion of the crown to enamel and dentin. Proper isolation is vital to the success of bonded ceramic restorations. The rubber dam has long been considered the primary method of preventing contamination of the operating field, a crucial requisite for adhesion. However, many dentists do not use rubber dam isolation due to its penchant for slowing down procedures. The authors present a case report that describes a technique for the indirect bonding of a ceramic restoration to a maxillary first molar using rubber dam isolation in conjunction with a floss ligature, a method that is aimed at optimizing operator effectiveness and efficiency.
Dental adhesive technology has evolved significantly in recent years. This modality is dependent on the dental substrate, the adhesive system used, and the clinician's ability to isolate the tooth and perform the bonding procedure.1 The success of glass-ceramic restorations relies heavily on the quality of adhesion of the crown to enamel and dentin, the latter being more complex due to the variability in hard tissue of the tooth.2 Adhesion to either dentin or enamel cannot occur in the presence of contamination, therefore proper isolation is a key aspect in the success of bonded ceramic restorations.3 A systematic review on the longevity of ceramic onlays found that the second most common cause of failure was debonding of restorations, and one of the main factors that complicated retention of ceramic restorations was poor isolation.4
For many years, the rubber dam has been considered the optimal method of preventing contamination of the operating field, but it is not widely used. Gilbert et al found that most dentists (63%) did not use a rubber dam for any restoration, while 33% stated that rubber dam isolation is too slow for use in a busy practice.5
This case report describes a technique to indirectly bond a ceramic restoration to a maxillary first molar using rubber dam isolation in conjunction with a floss ligature to optimize operator effectiveness and efficiency.
Case Report
A 36-year-old female patient presented to the faculty practice group at the Dental College of Georgia at Augusta University with the chief complaint of "pain on the upper left side while chewing." The patient's medical history was noncontributory. Clinical examination revealed the presence of a fractured Class II amalgam restoration in the maxillary left first molar (Figure 1) accompanied by gingival inflammation of the mesial interproximal papilla. The patient had discontinued flossing the area due to discomfort.
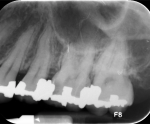
Periapical (Figure 2) and bitewing radiographs were obtained, and an extensive recurrent carious lesion beneath the mesial restoration was observed. Although the caries was in close proximity to the pulp chamber, the tooth exhibited no radiographic periapical pathology and had no past history of spontaneous pain. Evaluation of the pulp via cold test (Endo-Ice®, Coltene/Whaledent, Inc, coltene.com) elicited a hypersensitive response without lingering pain upon removal of the stimulus, yielding an endodontic diagnosis of reversible pulpitis.
After the clinician presented both direct and indirect restorative options for this tooth, the patient weighed the risks versus benefits of each and chose an indirect full-coverage restoration that would offer the most predictable longevity and was also the only indirect option covered by her dental plan. Verbal and written consent for an all-ceramic crown was obtained from the patient.
Local anesthesia was attained with articaine 4% with 1:100,000 epinephrine (Septocaine® HCl 4%, Septodont, septodontusa.com) and the fractured amalgam was removed. Caries removal and crown preparation extended apically, revealing that both proximal margins entered the periodontal attachment and impinged on biologic width (Figure 3). A bis-acryl (Integrity®, Dentsply Sirona, dentsplysirona.com) provisional crown was fabricated and the patient was referred for periodontal crown lengthening.
Three months after the surgical procedure, the crown preparation was refined, with proximal margins located at the new gingival crest. Fine braided retraction cord (Ultrapak™ #00, Ultradent Products, Inc, ultradent.com) was placed (Figure 4), the preparation was scanned (PlanScan®, Planmeca, planmeca.com), and files were sent to the dental laboratory for the designing, milling, and glazing of a lithium-disilicate crown (IPS e.max® CAD, Ivoclar Vivadent, ivoclarvivadent.com).
Prior to try-in, the patient was anesthetized the same as at the preparation appointment, the crown was seated, and marginal fit and interproximal contacts were verified. Rubber dam isolation was completed using a floss ligature to invert the dam apical to the preparation margins and expose a clean rim of enamel (Figure 5). Adjacent teeth were protected from etching with polytetrafluoroethylene (PTFE) tape. Selective etching of enamel margins was completed using 32% phosphoric acid (Uni-Etch®, BISCO, bisco.com) (Figure 6), and then the preparation was rinsed and lightly air-dried. Next, the primer of a two-step self-etching dental adhesive (OptiBond™ XTR, Kerr, kerrdental.com) was applied to the preparation for 20 seconds, then completely air-dried. Lastly, the adhesive of the same system was applied, thinned with a microbrush, and light-cured with an LED curing light (Valo™, Ultradent Products, Inc) for 20 seconds at 1000 mW/cm2 (Figure 7).
The intaglio surface of the all-ceramic restoration had been previously cleaned and etched with 4% hydrofluoric acid (Porcelain Etchant, BISCO) for 20 seconds; this was followed by the application of two coats of pre-hydrolyzed silane primer (Porcelain Primer, BISCO), each of which was thoroughly air-dried. A dual-cured resin cement (NX3 Nexus™, Kerr) was mixed according to the manufacturer's instructions and applied on the walls and margins of the intaglio surface of the crown, and the crown was seated using finger pressure. Excess cement at the crown margins was tack-cured for 2 seconds and removed using the tip of the explorer, then full polymerization was achieved using the same curing light and setting used for the adhesive layer. The curing light was applied to facial, lingual, and occlusal surfaces for 20 seconds each (Figure 8).
Removal of excess cement from all margins was verified and the rubber dam was removed. Occlusal adjustment was completed using ultrafine finishing diamonds under water coolant, and the crown was polished with diamond-impregnated rubber points (Komet USA, kometusa.com) (Figure 9).
At a 2-year follow-up appointment, clinical and radiographic examination revealed well-adapted margins and no caries (Figure 10 and Figure 11). The patient reported no postoperative sensitivity after cementation and no sensitivity or other symptoms during the intervening 2 years.
Discussion
All-ceramic restorations have become a popular option among restorative dentists due to their esthetic and optical properties, along with 5- to 10-year survival rates ranging from 91% to 98%.4 Although the crown preparation of the tooth in the present case would have adequately retained a cemented zirconia crown, a more esthetic lithium-disilicate restoration was selected because the tooth was visible when the patient smiled. This choice of restorative material in a molar and the relatively minimal occlusal reduction dictated the use of resin bonding to reinforce the long-term success of the crown.6,7
Resin bonding requires multiple steps and demands fairly long intervals of isolation, which can be readily attained with a rubber dam. All-ceramic crowns that require resin bonding are mostly indicated when enamel margins can be placed at or coronal to the gingival crest as in the case presented, and usually the use of a dental floss ligature is needed to invert the rubber dam along restoration margins. The authors recommend using unwaxed floss secured with a noose-style knot (Figure 12) that fits tightly around the tooth. To do this, it is recommended that an assistant secure the ligature apical to the preparation margin on the lingual with a cord-packing instrument while the dentist tightens the ligature and ties the floss knot along the facial margin (Figure 5). Given that periodontal crown lengthening made the application of the floss ligature simpler due to the location of the supragingival margins, the authors wish to point out that this technique is viable for patients with normal tissue height (Figure 13). Other isolation methods also are available, such as the use of retraction clamps like a B4 or modified 212. Practitioners must achieve accessible and clean margins if adhesive cementation is the goal.
A system employing a mild self-etching primer (pH = 3.3) followed by an adhesive was selected for dentin bonding of the restoration to minimize the risk of over-etching and subsequent extravasation of dentinal fluid that could compromise the bond.8 This system is thus considered to produce a better dentin bond than single-component self-etching adhesives or self-adhesive resin cements.9 A selective enamel etch technique was used because self-etching resins are too mild in pH to produce optimal enamel bonding.10
A technique where dentin bonding for an indirect restoration is initiated at the time of the preparation appointment is termed immediate dentin sealing.11 It has demonstrated improved resin bonding to dentin in in vitro studies. The authors considered the implementation of immediate dentin sealing as a contraindication for this case because most of the dentin preparation was done several months before final crown delivery, and the effects of such a long delay are unknown. Rather, the authors opted to seal the dentin at the time of crown delivery, known as delayed dentin sealing.
When it comes to the decision-making process of what type of isolation to use, the authors recommend rubber dam isolation when: (1) bonding indirect restorations, (2) the margins are accessible, and (3) the margins are deeper and floss ligature or a retraction clamp can be used. If these criteria cannot be met, the use of a non-etchable ceramic combined with a resin-modified glass-ionomer (RMGI) cement is suggested.
At the time of this writing, the restoration and adhesion protocol presented in this case report has been both stable and effective for more than 2 years. The patient, who initially presented with cold sensitivity and reversible pulpitis, has been symptom-free since seating of the crown. Although this is only one sample case, and other studies regarding the pulpal effects of immediate and/or delayed dentin sealing are needed, the implication is that there is little downside to delayed dentin sealing with optimal isolation, which is consistent with the clinical experience of the authors who had completed many all-ceramic restorations bonded at the time of the seating appointment.
Conclusion
All-ceramic restorations are a common choice in today's restorative practices. When delivering these restorations, clinicians have the option of bonding them using a combination of adhesive materials and resin cements. Lack of moisture control around deep margins can affect the bonding process, which is why rubber dam isolation in combination with a floss ligature is suggested for use as an aid to control contamination of the operating field.
About the Authors
Mario F. Romero, DDS
Associate Professor, Department of Restorative Sciences, Director, Advanced Education in General Dentistry Residency, Dental College of Georgia, Augusta University, Augusta, Georgia
Jacqueline Delash, DMD, MPH
Instructor, Department of Restorative Sciences, Dental College of Georgia, Augusta University, Augusta, Georgia
Roger M. Arce, DDS, MS, PhD
Associate Professor, Department of Periodontics and Oral Hygiene, University of TexasHealth Science Center at Houston (UTHealth), School of Dentistry, Houston, Texas
Courtney S. Babb, DMD
Instructor, Department of General Dentistry, Dental College of Georgia, Augusta University, Augusta, Georgia
William W. Brackett, DDS, MSD
Professor, Department of Restorative Sciences, Dental College of Georgia, Augusta University, Augusta, Georgia
References
1. Summitt JB, Robbins JW, Hilton TJ, et al, eds. Fundamentals of Operative Dentistry: A Contemporary Approach. 3rd ed. Quintessence Publishing; 2006:516-518.
2. Summitt JB, Robbins JW, Hilton TJ, et al, eds. Fundamentals of Operative Dentistry: A Contemporary Approach. 3rd ed. Quintessence Publishing; 2006:186-187.
3. Park JW, Lee KC. The influence of salivary contamination on shear bond strength of dentin adhesive systems. Oper Dent. 2004;29(4):437-442.
4. Abduo J, Sambrook RJ. Longevity of ceramic onlays: a systematic review. J Esthet Restor Dent. 2018;30(3):193-215.
5. Gilbert GH, Litaker MS, Pihlstrom DJ, et al. Rubber dam use during routine operative dentistry procedures: findings from the Dental PBRN. Oper Dent. 2010;35(5):491-499.
6. Yazigi C, Kern M, Chaar MS. Influence of various bonding techniques on the fracture strength of thin CAD/CAM-fabricated occlusal glass-ceramic veneers. J Mech Behav Biomed Mater. 2017;75:504-511.
7. Vargas MA, Bergeron C, Diaz-Arnold A. Cementing all-ceramic restorations: recommendations for success. J Am Dent Assoc. 2011;142(suppl 2):20S-24S.
8. Hebling J, Castro FL, Costa CA. Adhesive performance of dentin bonding agents applied in vivo and in vitro. Effect of intrapulpal pressure and dentin depth. J Biomed Mater Res B Appl Biomater. 2007;83(2):295-303.
9. Brackett WW, Ito S, Tay FR, et al. Microtensile dentin bond strength of self-etching resins: effect of a hydrophobic layer. Oper Dent. 2005;30(6):733-738.
10. Brackett WW. The importance of enamel adhesion. Pract Proced Aesthet Dent. 2007;19(2):78.
11. Magne P, Kim TH, Cascione D, Donovan TE. Immediate dentin sealing improves bond strength of indirect restorations. J Prosthet Dent. 2005;94(6):511-519.