Interdisciplinary Management of a Complex Esthetic Dilemma
David P. Mathews, DDS; and Vincent G. Kokich, DDS, MSD†
Abstract: Esthetic dilemmas often require an interdisciplinary approach to achieve an optimal result. This article describes such a case in which the patient presented with unesthetic porcelain crowns on structurally compromised maxillary anterior teeth. The maxillary incisors had failing root canals, advanced mobility, and deep periodontal pockets. In addition, there was a congenitally missing maxillary lateral incisor. The canine substitution created a severely canted appearance exacerbated by the patient's high smile line. A coordinated interdisciplinary treatment plan was put into action to satisfy the patient's chief complaints and achieve a successful outcome. In this instance, this approach involved a periodontist, orthodontist, and prosthodontist, as well as initial input from an endodontist.
As esthetics have taken on an increasingly important role in dentistry over the past two decades-with society placing an ever-greater emphasis on the value of a beautiful smile-oftentimes the independent dental disciplines must work together to satisfy both a patient's need for function and desire for an attractive appearance. A coordinated interdisciplinary approach is often needed to maximize the effectiveness of restorative dentistry when highly complex esthetic cases present.
Case Presentation
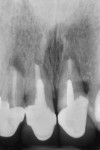
A 45-year-old female patient presented to a prosthodontist with a chief complaint that she had always disliked the slanted appearance of her upper front teeth (Figure 1). She had a congenitally missing maxillary left lateral incisor (tooth No. 10), and a very high smile line aggravated the esthetic situation. In addition, she was unhappy with the color of her porcelain crowns (Figure 2). She stated that she had multiple root canal treatments on her anterior teeth and endodontic surgery to try to save these teeth (Figure 3). The patient further stated that her general dentist had told her that the teeth could be crowned but that the prognosis was poor because of the failing root canals and periodontal bone loss and mobility. The general dentist had no plan to correct the slanted appearance of her teeth and referred the patient to the prosthodontist.
At the initial examination and consultation, the prosthodontist recommended an interdisciplinary approach. He told the patient that he would take her records and present her case to his interdisciplinary study group (Northwest Network for Dental Excellence) where he could obtain multiple opinions on how to best treatment-plan this complex case.
Interdisciplinary Diagnosis and Treatment Planning
The patient's records were presented to the interdisciplinary study group, which represented all dental specialties.1 Each pertinent specialist discussed his or her aspect of the treatment along with prognoses for each possible mode of therapy.
The endodontist felt that retreatment would be problematic because root canal therapy had been done multiple times and had included apical surgeries. Access to the canals on Nos. 8 and 9 would require removal of the crowns and posts. Additional apical surgery on Nos. 7 through 9 would most likely be needed.
The prosthodontist in the study group (not the original prosthodontist) suggested that teeth Nos. 8 and 9 were structurally and periodontally compromised even if endodontic retreatment could be successful. The periodontist was concerned about the 7 mm to 8 mm pocket depths and advanced mobility.2 It would be difficult to reduce the pockets and ameliorate the canted occlusal plane with osseous surgery.
The orthodontist proposed that eruption of teeth Nos. 7 through 9 and 11 would solve several of the problems. First, the canted occlusal plane could be significantly improved by erupting No. 11. This would also make the tooth appear more like a lateral incisor. Second, eruption of Nos. 7 through 9 would improve the crestal bone level and facilitate an implant treatment plan if these teeth were still deemed very guarded.3,4
The interdisciplinary group leader, a restorative dentist, led the discussion and generated a summary of all of the treatment possibilities and a sequence of treatment for each treatment plan and forwarded it to the study group prosthodontist. After consultation with the patient and acceptance of the treatment plan that the group had deemed ideal, referrals were made to the orthodontist and periodontist.
Treatment Plan and Sequence of Treatment
Among the treatment team there was much discussion about whether to try to save some of the anterior teeth despite the endodontic problems and 7 mm to 8 mm pocket depths and mobility. The overriding concern was the severe gingival cant, which was the patient's chief complaint. The group determined that trying to save teeth Nos. 7 through 9 was fraught with too many guarded prognoses with respect to endodontic retreatment, periodontal surgery, concern for mobility, and a compromised esthetic result. They believed the optimal treatment plan was to extrude teeth Nos. 7 through 9 to improve the bone level for implant placement,5-9 and also extrude tooth No. 11 to make it look like a lateral incisor. In addition, this would improve the severe canted appearance of the anterior gingival margins. After extrusion, teeth Nos. 7 through 9 would be extracted, and implants would be placed in either sites Nos. 7 and 9 for a fixed partial denture or sites Nos. 8 and 9 with a cantilevered No. 7.
Treatment
The patient first saw the periodontist for scaling and root planing and oral hygiene instruction and was kept on a quarterly maintenance schedule. Next, the prosthodontist removed the porcelain crowns on teeth Nos. 7 through 9. The preparations were shortened to allow for an ample amount of acrylic, which would simplify the task of reducing the provisional restorations as the teeth were erupted (Figure 4). The provisionals were bonded with permanent cement to ensure they would not loosen with the extrusive forces. The provisional on tooth No. 11 was left particularly short so that considerable extrusion could occur without the provisional being damaged (Figure 5).
The orthodontist began treatment that would entail eruption of the four involved teeth of approximately 0.5 mm to 1 mm per month.10 This would allow for optimal ridge development of the bone. At each visit, the orthodontist would shorten the length of the provisionals to allow for further extrusion. The orthodontist completed treatment in 5 months, and the teeth were stabilized with a rectangular archwire (Figure 6 and Figure 7). The patient was then referred to the periodontist for the extractions of teeth Nos. 7 through 9 and implant placement.
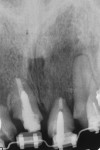
The plan was to place implants in either sites Nos. 7 and 9 or sites Nos. 8 and 9, whichever would prove to be the better option after the extractions. The teeth were extracted and the sites were evaluated (Figure 8 and Figure 9). One of the concerns before orthodontic extrusion was the apical lesions on teeth Nos. 7 through 9 and their potential effect on the amount of bone augmentation as the teeth erupted. Although site No. 7 had excellent bone, the presence of a large apical lesion would make it difficult to place a fixture there immediately. Sites Nos. 8 and 9 had excellent bone, and thus these sites were chosen for implant placement. Immediate implant placement was accomplished.11,12 Gaps between the implants and bone were filled with a mixture of particulate bone and calcium sulfate, and healing abutments were placed.
The large apical lesion on No. 7 was debrided, and the extraction socket was filled with a mixture of bone mineral substitute (BioOss®, Geistlich Biomaterials, dental.geistlich-na.com) and calcium sulfate and covered with a resorbable membrane (Figure 10).13 The patient left the periodontist's office and went to the orthodontist who placed a fixed wire temporary provisional to replace Nos. 7 through 9 and ligated it in place (Figure 11 and Figure 12). The patient healed uneventfully. The healing abutments and bone grafting in the gaps maintained a thick labial contour.
Five months after surgery, the sites, Nos. 7 through 9, had healed well (Figure 13), and the prosthodontist began provisionalization and tissue molding (Figure 14).14 The tissue partially covered the healing abutments, but no surgery was needed to uncover the fixtures. After 3 months, the tissue molding was completed and ideal gingival levels and papillae development were achieved (Figure 15 and Figure 16).
The final prosthesis was completed, and as shown in the 2-year follow-up photograph (Figure 17) the soft tissue had actually improved compared to the 3-month provisional photograph (Figure 16). It is interesting to note that the papillae were very close to ideal height at the 3-month provisional stage (Figure 16) despite there being adjacent implants, Nos. 8 and 9, that did not have medialized platforms.15,16In addition, the papilla between the implant at No. 8 and the No. 7 pontic was ideal.17-19 The patient's thick phenotype likely contributed to this optimal outcome.
At the 4-year follow-up, significant improvement of the canted appearance of the gingival margins, which had been the patient's chief complaint, was evident, as was the stability of the soft tissue and bone (Figure 18 through Figure 20).
Conclusion
This case demonstrated the effectiveness of a coordinated interdisciplinary approach when treating a patient with complex esthetic problems. The prosthodontist/restorative dentist was the "quarterback" in managing the sequence of treatment among the multiple specialists who contributed to the case. The critical element in this treatment was the correction of the patient's chief complaint, the severe cant of her gingival margins, which was accomplished by the orthodontist.
Acknowledgment
The authors thank Rodger A. Lawton, DMD, prosthodontist, for his help with the restorative dentistry in this case.
About the Authors
David P. Mathews, DDS
Specialist in Periodontics, Gig Harbor, Washington
Vincent G. Kokich, DDS, MSD†
Professor, Department of Orthodontics, School of Dentistry, University of Washington, Seattle, Washington
†Deceased
References
1. Spear FM, Kokich VG, Mathews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc. 2006;137(2):160-169.
2. Mathews DP, Kokich VG. Managing treatment for the orthodontic patient with periodontal problems. Semin Orthod. 1997;3(1):21-38.
3. Salama H, Salama M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: a systematic approach to the management of extraction defects. Int J Periodontics Restorative Dent. 1993;13(4):312-333.
4. Salama H, Salama M, Kelly J. The orthodontic-periodontal connection in implant site development. Pract Periodontics Aesthet Dent. 1996;8(9):923-932.
5. Hayashi J, Shin K. Implant site development by orthodontic extrusion and buccal root torque at a site showing severe gingival recession with periodontitis: a case report. Int J Periodontics Restorative Dent. 2019;39(4):589-594.
6. Ingber JS. Forced eruption: alteration of soft tissue cosmetic deformities. Int J Periodontics Restorative Dent. 1989;9(6):416-425.
7. Nozawa T, Sugiyama T, Yamaguchi S, et al. Buccal and coronal bone augmentation using forced eruption and buccal root torque: a case report. Int J Periodontics Restorative Dent. 2003;23(6):585-591.
8. Watanabe T, Marchack BW, Takei HH. Creating labial bone for immediate implant placement: a minimally invasive approach by using orthodontic therapy in the esthetic zone. J Prosthet Dent. 2013;110(6):435-441.
9. Hasson JN, Hasson B. Implant site development by orthodontic forced eruption for esthetic restoration of adjacent implants. Clin Adv Periodontics. 2016;6(3):146-152.
10. Spear FM, Kokich VG, Mathews DP. The esthetic management of a severe isolated periodontal defect in the maxillary anterior. Compend Contin Educ Dent. 2008;29(5):280-287.
11. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9
(5):332-343.
12. Lee J, Park D, Koo KT, et al. Comparison of immediate implant placement in infected and non-infected extraction sockets: a systematic review and meta-analysis. Acta Odontol Scand. 2018;76(5):338-345.
13. Horowitz RA, Mazor Z, Miller RJ, et al. Clinical evaluation alveolar ridge preservation with a beta-tricalcium phosphate socket graft. Compend Contin Educ Dent. 2009;30(9):588-594.
14. Potashnick SR. Soft tissue modeling for the esthetic single-tooth implant restoration. J Esthetic Dent. 1998;10(3):121-131.
15. Hsu YT, Lin GH, Wang HL. Effects of platform-switching on peri-implant soft and hard tissue outcomes: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2017;32(1):e9-e24.
16. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
17. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995-996.
18. Salama H, Salama MA, Garber D, Adar P. The interproximal height of bone: a guidepost to predictable aesthetic strategies and soft tissue contours in anterior tooth replacement. Pract Periodontics Aesthet Dent. 1998;10(9):1131-1141.
19. Choquet V, Hermans M, Adriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72(10):1364-1371.