Achieving Predictable Hydraulic Sinus Condensing Using an Innovative Functional Sinus Implant: A Case Report
Leon Chen, DMD, MS; and Jennifer Cha, DMD, MS
Abstract: Inadequate alveolar bone height/volume and sinus anatomy can complicate the predictable placement of conventional implants and subsequent restoration in posterior maxillary sites. A variety of sinus lift and vertical bone height augmentation materials and techniques have been utilized for this purpose; however, generally they are clinically challenging, demand well-trained surgical proficiency, and require the use of multiple armamentaria. Simultaneously, clinicians must meticulously handle the sinus membrane to achieve elevation without perforation, attain successful bone grafting, and ensure predictable implant osseointegration. The hydraulic sinus condensing (HSC) technique via the osteotomy site is designed to be less invasive than conventional sinus lift techniques, reduce trauma to patients, improve implant osseointegration into grafted alveolar bone, prevent sinus membrane perforation, and enhance the overall efficiency of the associated surgical process. This article briefly reviews the evolution of sinus lift and posterior maxillary implant insertion procedures and presents a case in which the HSC technique and a uniquely designed sinus implant were used.
The placement of dental implants in posterior maxillary sites has considerable potential for multiple complications resulting from the anatomical features that are characteristic of this area. First, posterior maxillary tooth loss from extraction or natural processes can cause sinus pneumatization and a resorbed osseous ridge, which impedes implant insertion in this area. Second, edentulous sites also can compromise the quality and quantity of available bone in this area, which is typically thin, porous, and lacking in volume.1 As a result, inadequate alveolar bone height/volume and maxillary sinus anatomy can complicate predictable placement of conventional implants and subsequent restoration.2
Additionally, although numerous studies substantiate an overall maxillary implant survival rate of more than 91%, invasion by dental implants into the maxillary sinus cavity is another frequent complication.3 The severity of the perforation (ie, separation between the soft Schneiderian membrane and the hard, bony sinus floor) is determined by its size and extent and dictates the remedial action needed and potential negative sequalae (eg, wound infection, implant failure, poor osseointegration, etc).4
Therefore, to enhance the likelihood of stable osseointegration and long-term predictability of implant treatments in the posterior maxilla and to overcome the challenges mentioned above, a variety of sinus lift and vertical bone height augmentation materials and techniques have been introduced and utilized during the past 20 years.5 For example, open sinus lift procedures, in which autogenous cancellous bone is used for sinus augmentation, have been the accepted standard when placing implants in the edentulous posterior maxillary area. However, despite enabling unencumbered access and clear visualization of the surgical site, open sinus lift procedures are highly invasive and traumatic, leading to postoperative swelling, pain, and discomfort, and even possible disability, for the patient.1 These procedures are also clinically demanding, requiring well-trained, proficient surgeons and a wide-ranging armamentarium.
In particular, open sinus lift procedures require meticulous handling of the sinus membrane to achieve elevation, prevent perforation, and avoid subsequent complications (eg, sinusitis, mucosal infections, drainage, surgical intervention).1,3 Other factors influencing the outcome of this technique include but are not limited to the stability of the bone graft material and preoperative infection management.1,6
Eventually, the alternative and slightly less traumatic closed sinus lift technique was introduced.7 This technique requires the clinician to first condense the alveolar bone using a mallet in order to improve the bone density surrounding the proposed implant site; then an osteotome technique may be performed to place bone grafting material into the sinus if the area is still deficient. Drawbacks of this technique, however, include difficulty lifting the sinus membrane as well as a requisite minimum ridge height.5
Subsequent attempts to reduce the invasiveness of sinus lift techniques were undertaken with the intent of reducing trauma to patients, improving implant osseointegration into grafted alveolar bone, preventing sinus membrane perforation, and simplifying the surgical process.1 Accessing the area via a lateral window to elevate the sinus membrane using a balloon and performing the sinus membrane balloon elevation and bone grafting through the osteotomy site in a closed techniquehave been cited in the literature for reducing complications, yielding acceptable results, and shortening procedure time.8,9 Facilitating even greater minimal invasiveness and more predictability of these procedures has been the introduction of modified closed sinus lift surgical techniques, an assortment of enhanced bone grafting materials that enable simultaneous grafting and immediate implant placement, and streamlined armamentaria that reduces the number of surgical steps and materials and amount of equipment required to place implants in deficient posterior maxillary sites.1,10
Hydraulic Sinus Condensing Technique
Since it was first described in 2005, a hydraulic sinus condensing technique (HSC™, Dental Implant Institute) performed through the implant osteotomy site has demonstrated favorable results and been shown to enable predictable, minimally invasive prosthetic rehabilitation of maxillary anterior and posterior areas where anatomical restrictions to implant placement are present.1,2,11,12 Although not ideal for all dental implant candidates, HSC is indicated for patients with advanced periodontitis in whom insufficient cortical bone at the alveolar ridge of the posterior maxilla impedes effective implantation; patients who have blood disorders or medication sensitivity (eg, vasoconstrictors); and patients lacking sufficient bone quantity and density in localized sinus floor areas.12
When first introduced, the HSC technique was performed using small round burs to access the sinus by creating a pinhole, through which constant hydraulic pressure from the handpiece during osteotomy drilling would inflate the sinus membrane. Once the membrane was loosened, a pliable atraumatic bone graft mixture would be packed and pushed using a combination of small sinus condensers of increasing width and hydraulic pressure from the surgical handpiece. An implant drill was then used to enlarge the osteotomy site, and the bone graft was condensed again by secondary lift. Upon completion of the sinus augmentation, the osteotomy site would be ready for immediate insertion.2,11,12
This type of two-stage internal crestal access approach (ie, first loosening the sinus membrane and then grafting bone particulate under the membrane) minimized the risk of membrane perforation. Threaded implants could then be placed during the same appointment and secured via primary closure.2,11,12
To further simplify sinus lifting procedures and enhance their predictability and success, additional modifications to bone grafting materials, handpieces, and the implants themselves have been introduced during the past 10 years. These changes have included but are not limited to the use of piezoelectric surgery, xenografts placed by hydraulic pressure, and specialized drilling systems to elevate the sinus membrane through a crestal approach and hydraulic pressure.13,14 Such advancements have been reported to increase procedural safety.14 Additionally, research has shown that for patients with a residual bone height of at least 3 mm, no implant failures, sinus membrane perforations, or adverse postoperative events occurred when the crestal sinus lift elevation, sinus grafts, and implant placement were conducted using these devices.15
Other novel procedures and implant devices have enabled simultaneous hydraulic elevation of the sinus membrane, placement of pliable bone graft materials, and dental implant insertion at the same appointment according to a closed sinus elevation technique.16 These innovations have helped dentists reduce patient discomfort, prevent intraoperative and postoperative adverse events (eg, sinus membrane tears, facial hematoma), and enhance treatment outcomes when the rehabilitation of atrophic edentulous posterior maxillary sites is required.17,18 Furthermore, one-stage piezosurgery for sinus elevation, bone grafting, and implant placement has been supplemented with the use of a combination of particulate bovine bone substitute and platelet-rich fibrin, and this approach has shown efficacy and good long-term prognosis without noteworthy complications during or after the same-day procedure.19
The following case demonstrates the most current evolution of the HSC technique, a posterior maxillary sinus lift, bone grafting, and implant insertion technique, using a combination of anorganic bovine bone grafting material, plasma-rich protein (PRP), and a specially threaded and cut implant.
Case Presentation
A 56-year-old woman presented with severe but localized periodontitis at tooth No. 16, and tooth No. 15 was missing. An intractable examination was performed, and panographic radiographs and computed tomography (CT) scans were obtained. The clinical and radiographic examinations revealed atrophic maxillary bone at the area of tooth No. 15, chronic sinusitis on the patient's left side, and a 1 mm sinus floor (Figure 1 through Figure 3). The patient also demonstrated a poor occlusal scheme between the left maxillary and mandibular teeth.
Treatment Plan
The proposed treatment plan would involve extraction of tooth No. 16 and immediate, minimally invasive hydraulic sinus floor elevation and bone augmentation at No. 15 via the HSC technique. This technique would incorporate placement of an implant (OsseoFuse Sinus implant, OsseoFuse, osseofuse.com)with anorganic bovine bone grafting material (Bio-Oss®, Geistlich Biomaterials, geistlich-na.com) as an osteoconductive filler combined with PRP into the sinus membrane space (ie, the space between the lining of the elevated Schneiderian membrane and bony maxillary sinus floor).4 In the author's experience, this particular osteoconductive bone grafting material is easy to handle in this situation.
Hydraulic sinus condensing enables dental implants to be placed at sites with as little as 2 mm of bone. The minimally invasive sinus augmentation procedure may also be performed when a severely sloping sinus floor or septum is present, and it produces minimal to no pain or swelling.4 With this technique, the full treatment of this area, including extraction, grafting/sinus lift, implant placement, and restoration, typically requires only 3 to 5 months.4
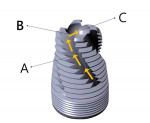
The selected implant was specifically chosen for this case based on its suitability for placement under the sinus membrane (Figure 4). In particular, the patented reverse helical side cut shaves the patient's own bone during insertion, after which the autogenous bone particles move apically from the helical side cut and are collected in a specially designed concave dish-like reservoir at the apex of the implant (Figure 5). A unique cutting design also at the apex of the implant functions as a built-in osteotome to effectively drill into the last 0.5 mm of sinus bony floor while simultaneously lifting the sinus membrane via the reservoir of excess bone and bone grafting material. Combined, these features are designed to ensure safety during the sinus augmentation procedure, contribute to enhanced build-up of the bone layer between the Schneiderian membrane and the sinus implant, and promote greater bone-to-implant surface contact.
As a result, enhanced stability following immediate placement in this problematic area may be achieved. Further, because the implant can be placed predictably using this technique, potential complications and/or sinus membrane perforation can be effectively managed, without the need to perform a separate osteotomy using additional armamentaria.
Additionally, the mount of the implant may subsequently be used either for a transfer coping for fixture-level impressions, a temporary abutment for preferred single-stage surgical techniques, or both. When appropriate, patients may be immediately provisionalized.
The risks and benefits of the proposed treatment were fully disclosed to the patient, who accepted the treatment and provided signed consent.
Surgical Procedure
The patient was anesthetized, and the implantation site was determined using the preoperative radiograph and CT scans of the area. A small hole was drilled into the crest of the alveolar ridge to less than 1 mm of the sinus floor using a high-speed sinus bur (OsseoFuse Sinus bur, OsseoFuse), after which a stream of water under hydraulic pressure was delivered to the site via a high-speed dental handpiece at the highest possible pressure setting until the sinus bur passed the cortex of the sinus floor.4 This served to loosen and gently lift the sinus membrane to accommodate bone density build-up for successful implant placement and osseointegration.1Because of the characteristics of the selected sinus implant, no widening of the osteotomy was required prior to placing the implant since the implant itself also functioned as an instrument to upfracture the sinus floor.
Next, 0.5 mg of the selected bone graft material (Bio-Oss) mixed with PRP was prepared (Figure 6) and placed onto the 5.25 mm x 10 mm sinus implant (OsseoFuse) (Figure 7). Using the same hole created to deliver the hydraulic pressure, the graft material and implant were placed (Figure 8), and the implant was torqued to 30 Ncm. In doing so, the graft material was simultaneously delivered and condensed into the bony sinus floor to further elevate the sinus membrane. Primary stability was noted. The condensation of the bone graft adapted the material to the slope and configuration of the sinus floor, all while a flapless procedure was utilized, which is conducive to enhanced patient recovery and a reduced likelihood of morbidity and complications.
After implant placement (Figure 9), primary closure was established, and a healing cap and cover screw were placed. In this case, primary closure, which typically refers to complete mucosal coverage over the surgical site, was necessary to contain the graft materials and prevent external pressure. CT scans were taken to verify proper implant placement and angulation and that there was an unperforated lift of the sinus membrane (Figure 10 and Figure 11).
The patient was provided with home care and oral hygiene instructions, which included taking amoxicillin 500 mg three times a day for 7 days and avoiding aggressive nose blowing and sneezing,and was dismissed. A 5-month period was allotted for osseointegration and healing prior to placement of a fixed single-unit implant crown restoration.
Eighteen months after the date of the original maxillary procedure, CT scan and radiographic evaluation confirmed the overall success of the HSC procedure using the novel sinus implant device to lift the sinus membrane and augment the maxillary bone in that area, as well as the predictable osseointegration of the maxillary implant and two subsequently placed mandibular implants (Figure 12 through Figure 14).
Conclusion
Although various sinus lift and vertical bone height augmentation materials and techniques have been used over the years to enhance the outcomes of posterior maxillary implant placement, treatment of deficient sites in this area has remained clinically challenging. In addition to demanding that clinicians demonstrate well-trained surgical proficiency, these procedures have also required the use of multiple instruments and devices. As demonstrated in this case report, as well as in a previously published report that documented 8-year success/survival of this procedure,4 techniques such as HSC through the osteotomy site have evolved and now afford clinicians the opportunity to achieve exceptional efficiency and predictability when performing posterior maxillary sinus lift and implant insertion procedures. By incorporating a simple armamentarium, efficient and efficacious materials such as anorganic bovine bone grafting material and PRP, and more streamlined devices (ie, a specially threaded and cut implant), the HSC technique offers an effective approach for minimally invasive sinus lifts, preventing sinus membrane perforation, reducing patient trauma, and improving implant osseointegration into grafted alveolar bone.
Disclosure
Dr. Chen is the developer of the patented Hydraulic Sinus Condensing (HSC™) technique. Drs. Chen and Cha are paid consultants for OsseoFuse International, Inc.
About the Authors
Leon Chen, DMD, MS
Founder and Chief Executive Officer, Dental Implant Institute, Las Vegas, Nevada; Fellow and Diplomate, International Congress of Oral Implantologists
Jennifer Cha, DMD, MS
President, Dental Implant Institute, Las Vegas, Nevada; Fellow and Diplomate, International Congress of Oral Implantologists
References
1. Ardekian L, Levit L, Michael L. Acute sinusitis and implant failure following novel minimally invasive hydraulic sinus lift: a case report. Clin Surg. 2018;3:1882.
2. Chen L, Cha J. An 8-year retrospective study: 1,100 patients receiving 1,557 implants using the minimally invasive hydraulic sinus condensing technique. J Periodontol. 2005;76(3):482-491.
3. Chen L, Cha J, Chen HC, Lin HL. Sinus perforation: treatment and classifications. J Implant Advanced Clin Dent. 2011;3(1):19-30.
4. Chen L, Cha J. Dental implant migration into two different maxillary sinus cavities. J Implant Advanced Clin Dent. 2012;4(4):21-25.
5. Stern A, Green J. Sinus lifts procedures: an overview of current techniques. Dent Clin North Am. 2012;56(1):219-233.
6. Almaghrabi BA, Hatton MN, Andreana S, Hoeplinger MA. Treatment of severe sinus infection after sinus lift procedure: a case report. Implant Dent. 2011;20(6):430-433.
7. Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15(2):152-158.
8. Soltan M, Smiler DG. Antral membrane balloon elevation. J Oral Implantol. 2005;31(2):85-90.
9. Kfir E, Kfir V, Mijiritsky E, et al. Minimally invasive antral membrane balloon elevation followed by maxillary bone augmentation and implant fixation. J Oral Implantol. 2006;32(1):26-33.
10. Del Fabbro M, Rosano G, Taschieri S. Implant survival rates after maxillary sinus augmentation. Eur J Oral Sci. 2008;116(6):497-506.
11. Chen L, Cha J, Chen HC. Two different clinical indications using hydraulic sinus condensing (HSC) technique: ten years follow-up. Dent Implantol Update. 2009;20(5):33-38.
12. Chen L. Correcting maxillary sinus deficiencies. Dent Implantol Update. 2008;19(10):65-70.
13. Li J, Lee K, Chen H, Ou G. Piezoelectric surgery in maxillary sinus floor elevation with hydraulic pressure for xenograft and simultaneous implant placement. J Prosthet Dent. 2013;110(5):344-348.
14. Kim YK, Cho YS, Yun PY. Assessment of dentists' subjective satisfaction with a newly developed device for maxillary sinus membrane elevation by the crestal approach. J Periodontal Implant Sci. 2013;43
(6):308-314.
15. Gatti F, Gatti C, Tallarico M, et al. Maxillary sinus membrane elevation using a special drilling system and hydraulic pressure: a 2-year prospective cohort study. Int J Periodontics Restorative Dent. 2018;38(4):593-599.
16. Better H, Slavescu D, Barbu H, et al. Minimally invasive sinus lift implant device: a multicenter safety and efficacy trial preliminary results. Clin Implant Dent Relat Res. 2014;16(4):520-526.
17. Tallarico M, Better H, De Riu G, Meloni SM. A novel implant system dedicate to hydraulic Schneiderian membrane elevation and simultaneously bone graft augmentation: an up-to 45 months retrospective clinical study. J Craniomaxillofac Surg. 2016;44(8):1089-1094.
18. Tallarico M, Meloni SM, Xhanari E, et al. Minimally invasive sinus augmentation procedure using a dedicated hydraulic sinus lift implant device: a prospective case series study on clinical, radiologic, and patient-centered outcomes. Int J Periodontics Restorative Dent. 2017;37
(1):125-135.
19. Barbu HM, Andreescu CF, Comaneanu MR, et al. Maxillary sinus floor augmentation to enable one-stage implant placement by using bovine bone substitute and platelet-rich fibrin. Biomed Res Int. 2018;2018:6562958. doi: 10.1155/2018/6562958.