Treatment of Maxillary Sinusitis of Odontogenic Origin: A Case Series
Jenna L. Starkey, DMD; and Rory E. Mortman, DDS
Odontogenic sinusitis is associated with periodontal disease and/or endodontic infection in close proximity to the floor of the sinus.1 Posterior maxillary dentition that presents with periapical infection has been shown to affect the maxillary sinus mucosa even without perforation of the cortical bone, with the infection spreading to the sinus via blood vessels, lymphatics, and bone marrow.2 Teeth with apices in close proximity to the maxillary sinus floor have a higher association with sinusitis.1,3,4 Patients may present with variable sinonasal symptoms such as recurrent sinus infections, headaches, anterior maxillary tenderness, nasal congestion, and discharge with or without a postnasal drip. Dental symptoms can range from no symptoms to sensitivity on endodontic testing such as thermal, percussion, and palpation tests.3 On a routine radiograph, normal sinus mucosa is typically not visualized, but when affected by infection or allergy it may become thicker and, therefore, more visible on images.5-9 The utilization of radiographs, clinical examination, and pulpal testing is essential in determining the etiology of maxillary sinusitis.
Panoramic and intraoral radiographs are standard for use in evaluation of apical pathology. However, these 2-dimensional (2D) imaging modalities are limiting in that they do not allow accurate assessment of root canal morphology, sinus pathology, or the relationship of roots and periapical infection to the sinus floor. Cone-beam computed tomography (CBCT) allows for a 3-dimensional (3D), higher-quality image and better visualization of the bone and soft tissues.10 CBCT is currently the choice of imaging for treatment of most endodontic procedures according to the American Association of Endodontists (AAE) and the American Academy of Oral and Maxillofacial Radiology.11 CBCT imaging can help with diagnosis and determining the course of treatment for patients with maxillary odontogenic sinusitis.8,10,12-14
Longhini and Ferguson published an extensive review of the otolaryngologic literature and found very few guidelines that list dental infection as a potential cause of sinusitis. Only three of the 85 sinusitis guidelines studied recommended a dental examination, and none mentioned referral to endodontic specialists.15 In past studies, it was found that only about 10% to 12% of maxillary sinusitis cases had odontogenic origin16; however, more recent studies suggest the incidence of odontogenic maxillary sinusitis cases could be as high as 25% to 40%.3,8,17-19 Odontogenic sources of infection in relation to sinusitis are frequently missed on routine dental examination.17 This results in odontogenic sinusitis being underdiagnosed among otolaryngologists, dentists, and radiologists. Otolaryngologists are then faced with patients whose symptoms persist after medical and surgical sinusitis therapy.15,20 A collaboration among otolaryngologists, dentists, and dental specialists is required for accurate diagnosis and treatment of maxillary sinusitis.
The following three case reports show examples of maxillary sinusitis with odontogenic etiology and how the use of CBCT improved assessment, diagnosis, and management with appropriate odontogenic treatment.
Case 1
A 64-year-old Caucasian woman was referred for endodontic evaluation of a porcelain-fused-to-metal (PFM) three-unit fixed partial denture from Nos. 12 through 14. Her chief complaint was dull, throbbing pain in the upper left quadrant. Her medical history was significant for hypertension, heart murmur, diabetes, recent weight loss, hay fever, bronchitis, and allergy to codeine. Her current medication regimen included metformin, rosuvastatin (Crestor®), cetirizine (Zyrtec®), ibuprofen (Advil®), clopidogrel (Plavix®), and amlodipine/benazepril (Lotrel®). The patient reported having mild seasonal rhinitis with persistent cough and sinusitis.
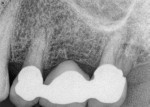
On clinical evaluation, teeth Nos. 12 and 14 (Figure 1) were negative to thermal testing, palpation, mobility, percussion, and biting. Periodontal probing depths were within normal limits. An intraoral swelling at the apices of No. 14 was noted. An intraoral periapical radiograph revealed no signs of periapical pathology.
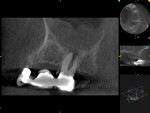
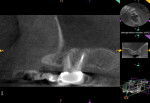
The patient underwent a CBCT study (Kodak 9000, Carestream Dental, carestreamdental.com) for further evaluation of the area (Figure 2). The 3D scan revealed thickening of the mucous membrane of the maxillary sinus, indicating severe chronic sinusitis and a large periradicular radiolucency at the apices of No. 14 (Figure 2). The pulpal diagnosis of tooth No. 14 was necrotic and the periapical diagnosis was chronic apical periodontitis.
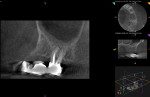
Endodontic treatment was determined to have a favorable prognosis, and such treat-ment was initiated using 2% lidocaine 1:100,000 epinephrine for anesthesia. Rubber dam isolation was achieved, and the tooth was accessed through the occlusal of the crown. The mesiobuccal (MB), mesiobuccal second (MB2), distobuccal (DB), and palatal (P) canals were located and pulpectomy was completed. The canals were filled with gutta-percha and root canal sealer (AH Plus®, Dentsply Sirona, dentsplysirona.com) using a warm vertical compaction technique (Figure 3).
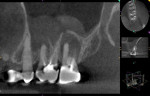
The patient returned 6 months later for a follow-up CBCT scan (Figure 4). The scan revealed near-complete resolution of the periapical lesion and mild residual mucosal thickening of the sinus floor. At this follow-up visit the patient reported her dental and sinus symptoms had resolved.
Case 2
A 72-year-old man was referred for endodontic evaluation of teeth Nos. 14 and 15. He complained chiefly of intermittent, dull pain in the upper left quadrant that had persisted for 2 weeks. His medical history was significant for hypertension, and he was currently taking the medications allopurinol and amlodipine/benazepril (Lotrel). Tooth No. 14 had been previously root canal treated and restored with a core and a PFM crown. Tooth No. 15 had been previously root canal treated and restored with a post, core, and crown. Teeth Nos. 13 and 14 were negative to thermal, percussion, and palpation tests. Tooth No. 15 had class I mobility and was negative in response to thermal, percussion, and palpation tests. Periodontal probing measurements for all teeth were within normal limits except for tooth No. 15, which had pinpoint probing to the apex on the mesial root. Clinically, tooth No. 15 had no opposing tooth.
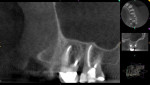
The radiographic examination with digital 2D radiographs revealed a diffuse radiolucency at the apices and a widened lamina dura for tooth No. 15 (Figure 5). The patient underwent a CBCT study (Kodak 9000) for further evaluation of the area. The CBCT scan revealed two dome-shaped radiopacities of soft-tissue density superior to teeth Nos. 14 and 15 and a large 8 mm x 8 mm periapical lesion associated with the palatal root of No. 15 with penetration through the cortical bone into the sinus. Tooth No. 14 revealed a periapical radiolucency at the MB root due to an unobturated mesiolingual (ML) canal (Figure 6).
Recommended treatment comprised extraction of tooth No. 15 by an oral surgeon followed by retreatment of tooth No. 14. No. 14 was determined to have a pulpal diagnosis of previously treated and a periapical diagnosis of symptomatic apical periodontitis. Endodontic retreatment was performed on tooth No. 14. The tooth was anesthetized with 2% lidocaine 1:100,000 epinephrine and 4% Septocaine® 1:100,000 epinephrine (Septodont, septodontusa.com), isolated with a rubber dam, and access was initiated through the occlusal of the crown. The canals were re-instrumented, irrigated with 6% sodium hypochlorite, and medicated with calcium hydroxide. A Cavit™ (3M Oral Care, 3m.com) temporary restoration was then placed. Two weeks later, the patient returned for completion of the root canal via the use of warm vertical compaction of gutta-percha, and a composite restoration was placed.
The patient returned 24 months later, and his dental symptoms had resolved (Figure 7). The follow-up CBCT scan revealed resolution of the periapical lesion and complete reduction of the sinus mucosal thickening (Figure 8).
Case 3
A 73-year-old Caucasian woman was referred for endodontic evaluation of the upper left quadrant. Her chief complaint was dull, throbbing pain in this area that had developed gradually in the past week. Her medical history was significant for thyroid nodules, persistent sinusitis, and allergy to penicillin and sulfa drugs. Her medication regimen included Excedrin®, ibuprofen (Advil), and metoprolol succinate (Toprol®).
Teeth Nos. 14 and 15 had been previously root canal treated and restored (Figure 9). On the clinical examination, tooth No. 13 was negative to palpation, percussion, and biting and had within-normal response to thermal testing. Tooth No. 14 was positive to palpation, positive to percussion and biting, and had no response to thermal testing. Tooth No. 15 was negative to palpation, percussion and biting, and thermal testing. Periodontal probing and mobility were all within normal limits.
The intraoral periapical film revealed no evidence of periapical pathology. A CBCT study (Kodak 9000) revealed a large periapical radiolucency at the apex of the MB root of tooth No. 14 with evidence of perforation through the cortical bone and into the sinus. The CBCT also disclosed two dome-shaped radiopacities of soft-tissue density superior to teeth Nos. 14 and 15 (Figure 10). The pulpal diagnosis for No. 14 was previously treated and the periapical diagnosis was acute apical abscess.
Endodontic retreatment of No. 14 was started with 2% lidocaine 1:100,000 epinephrine for anesthesia and isolation with a rubber dam; access was initiated through the occlusal of the crown. The core and gutta-percha were removed, the canals were re-instrumented, and calcium hydroxide was placed into the canals as a medicament. This was followed by placement of a Cavit temporary restoration.
At the follow-up examination 2 weeks later, the tooth was asymptomatic, and the sinus congestion was resolved. The canals were then filled with gutta-percha and root canal sealer (AH Plus), and composite was placed. The patient returned 12 months later for a follow-up visit (Figure 11), which included a CBCT scan that showed partial resolution of the periapical lesion and resolution of all sinus pathology (Figure 12).
Discussion
Many factors and conditions can contribute to the development of odontogenic sinusitis. These include spread of endodontic infection in the maxilla, periapical cysts, granulomas, and displacement of foreign bodies into the sinus such as endodontic materials, tooth fragments, implants, or augmentation grafts.3,19,21,22 The AAE recently published a position statement distinguishing the difference between maxillary sinusitis of dental origin (MSDO) and maxillary sinusitis of endodontic origin (MSEO), indicating that the treatment and management of the two may differ. MSEO has been characterized as sinusitis that is secondary to endodontic periradicular disease and excludes other dental etiologies of odontogenic sinusitis. Patients with MSEO frequently present without dental symptoms or complaints and typically seek care from their primary care physician or ear/nose/throat (ENT) physician due to their sinonasal symptoms. Therefore, if mucosal abnormalities exist or there is obstruction of the sinus, physicians and dentists must not rule out an odontogenic source of infection.20 Otolaryngologists and dentists should always suspect an odontogenic origin for sinusitis cases and refer to an endodontic specialist if needed.
Biofilms involved in odontogenic sinusitis are generally characterized as polymicrobial. Acute bacterial sinus infections of non-odontogenic sources typically involve nasal cavity aerobic commensals, including Staphylococcus aureus, Haemophilus influenzae, Moraxella catarrhalis, and others.3,12,22-25 In odontogenic sinusitis, the sinonasal environment changes to that characteristic of chronic sinus infections with predominance of anaerobic bacteria.12,22-25 Puglisi et al studied the microbiology of specimens taken from 59 patients with a history of chronic maxillary sinusitis; of the bacteria cultured, all were polymicrobial and most were anaerobic.24 Saibene et al studied 28 patients with sinus infections whose symptoms had not resolved after sinonasal surgery. The most common isolates found were oropharyngeal flora that were also predominate in periodontal and endodontic infections. These included Peptostreptococcus, Fuso-bacterium, Prevotella spp., and Porph-yromonus spp.24,25 The differences in microbial communities and source of infection explains why patients with odontogenic sinusitis require different approaches to treatment.
The direct extension of dental disease into the maxillary sinus was first discovered in a 1943 cadaver study by Bauer. The areas of infection showed disruption of the cortical bone that separates maxillary roots from the floor of the sinus. Other findings included inflammation, mucosal hypertrophy, cyst formation, and granulation tissue.2 In a CBCT study evaluating the maxillary sinuses of 243 patients, 60% showed mucosal thickening, and those that involved periapical lesions were 9.75 times more likely to have abnormalities.6 In a study by Nascimento et al maxillary sinus mucosal thickening presented in more than 90% of 400 sinusitis patients.5 In the present case series, all the patients presented with maxillary sinus mucosal thickening, which is consistent with past studies.4-9
The use of CBCT imaging significantly improved the ability to diagnose the source of infection in these cases. CBCT is frequently used in endodontics because of its ability to provide a higher-quality image with thin slices for better visualization of the bone and soft tissues.10 In the cases presented in this study, intraoral radiographs did not show evidence of dental pathology and led to initial inaccurate diagnosis of the source of infection. Melén et al conducted a study that found 55% of the 99 cases of odontogenic maxillary sinusitis studied were missed on routine dental examination.17 Cymmerman et al compared 1014 images taken from 596 patients and found that CBCT imaging was 54% more accurate in detecting apical lesions compared to intraoral radiographs.14 In a study by Lofthag-Hansen, sinus mucosal thickening was four times more likely to be identified on CBCT imaging than with traditional intraoral films.26
The increased availability of CBCT in dental offices in recent years has allowed for improved recognition of odontogenic sinusitis. In all three of the cases in this study, periapical infection was missed on routine dental examination and was not discovered until CBCT imaging was performed. Once the source of infection was established and the appropriate treatment was performed, the patient's dental and sinonasal symptoms resolved. Collectively, the literature strongly supports interdisciplinary action among physicians, dentists, and dental specialists to provide a patient-centered approach for treatment and management of maxillary odontogenic sinusitis.
Conclusion
This case series presented three patients with odontogenic maxillary sinusitis. After appropriate odontogenic treatment, the accompanying sinusitis resolved relatively quickly. In each of these cases, dental etiology was not evident until CBCT imaging and endodontic clinical examination were performed. Collaboration among dentists, dental specialists, and otolaryngologists is needed for successful treatment of sinusitis of dental origin.
About the Authors
Jenna L. Starkey, DMD
Private Practice, Jacksonville, Florida
Rory E. Mortman, DDS
Private Practice specializing in Endodontics, West Palm Beach, Florida; Diplomate, American Board of Endodontics
References
1. de Lima CO, Devito KL, Baraky Vasconselos LR, et al. Correlation between endodontic infection and periodontal disease and their association with chronic sinusitis: a clinical-tomographic study. J Endod. 2017;43(12):1978-1983.
2. Bauer WH. Maxillary sinusitis of dental origin. Am J Ortho Oral Surg. 1943;29(3):133-151.
3. Mehra P, Murad H. Maxillary sinus disease of odontogenic origin. Otolaryngol Clin North Am. 2004;37(2):347-364.
4. Nunes CA, Guedes OA, Alencar AH, et al. Evaluation of periapical lesions and their association with maxillary sinus abnormalities on cone-beam computed tomographic images. J Endod. 2016;42(1):42-46.
5. Nascimento EH, Pontual ML, Pontual AA, et al. Association between odontogenic conditions and maxillary sinus disease: a study using cone-beam computed tomography. J Endod. 2016;42(10):1509-1515.
6. Shanbhag S, Karnik P, Shirke P, Shanbhag V. Association between periapical lesions and maxillary sinus mucosal thickening: a retrospective cone-beam computed tomographic study. J Endod. 2013;39(7):853-857.
7. Lee KC, Lee SJ. Clinical features and treatments of odontogenic sinusitis. Yonsei Med J. 2010;51(6):932-937.
8. Maillet M, Bowles WR, McClanahan SL, et al. Cone-beam computed tomography evaluation of maxillary sinusitis. J Endod. 2011;37(6):753-757.
9. Lu Y, Liu Z, Zhang L, et al. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: a retrospective study. J Endod. 2012;38(8):
1069-1074.
10. Low KM, Dula K, Bürgin W, von Arx T. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery. J Endod. 2008;34(5):557-562.
11. Special Committee to Revise the Joint AAE/AAOMR Position Statement on use of CBCT in Endodontics. AAE and AAOMR joint position statement: use of cone beam computed tomography in endodontics 2015 update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(4):508-512.
12. Brook I. Microbiology and antimicrobial management of sinusitis. Otolaryngol Clin North Am. 2004;37(2):253-266.
13. Nair UP, Nair MK. Maxillary sinusitis of odontogenic origin: cone-beam volumetric computerized tomography-aided diagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(6):e53-e57.
14. Cymerman JJ, Cymerman DH, O'Dwyer RS. Evaluation of odontogenic maxillary sinusitis using cone-beam computed tomography: three case reports. J Endod. 2011;37(10):1465-1469.
15. Longhini AB, Ferguson BJ. Clinical aspects of odontogenic maxillary sinusitis: a case series. Int Forum Allergy Rhinol. 2011;1(5):409-415.
16. Maloney PL, Doku HC. Maxillary sinusitis of odontogenic origin. J Can Dent Assoc (Tor). 1968;34(11):591-603.
17. Melén I. Chronic sinusitis: clinical and pathophysiological aspects. Acta Otolaryngol Suppl. 1994;515:45-48.
18. Bomeli SR, Branstetter BF 4th, Ferguson BF. Frequency of a dental source for acute maxillary sinusitis. Laryngoscope. 2009;119(3):580-584.
19. Abrahams JJ, Glassberg RM. Dental disease: a frequently unrecognized cause of maxillary sinus abnormalities? AJR Am J Roentgenol. 1996;166(5):1219-1223.
20. Tataryn RW, Lewis MJ, Horalek AL, et al. Maxillary sinusitis of endodontic origin. AAE Position Statement. 2018:1-11.
21. Legert KG, Zimmerman M, Stierna P. Sinusitis of odontogenic origin: pathophysiological implications of early treatment. Acta Otolaryngol. 2004;124(6):655-663.
22. Taschieri S, Torretta S, Corbella S, et al. Pathophysiology of sinusitis of odontogenic origin. J Investig Clin Dent. 2017;8(2).
23. Ahovuo-Saloranta A, Borisenko OV, Kovanen N, et al. Antibiotics for acute maxillary sinusitis. Cochrane Database Syst Rev. 2008;(2)CD000243.
24. Puglisi S, Privitera S, Maiolino L, et al. Bacteriological findings and antimicrobial resistance in odontogenic and non-odontogenic chronic maxillary sinusitis. J Med Microbiol. 2011;60(Pt 9):1353-1359.
25. Saibene AM, Vassena C, Pipolo C, et al. Odontogenic and rhinogenic chronic sinusitis: a modern microbiological comparison. Int Forum Allergy Rhinol. 2016;6(1):41-45.
26. Lofthag-Hansen S, Huumonen S, Gröndahl K, Gröndahl HG. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.2007;
103(1):114-119.