Implant-Supported Vs. Tissue-Supported Prosthesis: Biomechanical Principles for Fixed Full-Arch Restorations
Edmond Bedrossian, DDS; and Edmond Armand Bedrossian, DDS, MSD
In the edentulous alveolus, the lack of internal loading of the maxillary and/or mandibular alveolar bone results in its resorption vertically, posteriorly, and medially. Tallgren documented the resorption pattern of the edentulous alveoli and clinically observed over two decades that the greatest amount of alveolar bone atrophy/resorption occurs within the first year of edentulism.1 The bony atrophy affects the overlying facial soft tissues, as they are supported in part by the maxillary or mandibular alveolar bone and the anterior-posterior (A-P) positioning of the patient's dentition. With the loss of teeth and subsequent atrophy of the maxillary and mandibular alveoli, changes in the jaw relationship and facial musculature ensue, leading to deformation in facial form and morphology.2
To prevent changes resulting from alveolar atrophy, treatment of the edentulous alveolus with dental implants to re-establish form and function has become well accepted. During the past decade, a clear trend has emerged toward techniques that attempt to accommodate patients by reducing the postoperative morbidity associated with traditional surgical procedures.3
Interest in minimally invasive treatment is notably growing in the field of oral implantology.4 Although the use of grafting procedures to modify resorbed residual alveolar bone is still practiced, the graftless approach, in which implants are adapted to existing bony volume, has become quite popular.5-7 The acceptance of the graftless approach is due primarily to shortened treatment time, less postoperative morbidity, reduced cost, less bleeding and inflammation, and decreased postoperative pain.8-13 A reduced number of implants used as well as the placement of tilted implants have allowed treatment of patients who in the past were considered untreatable without associated grafting procedures.14-16
For clinicians to predictably adopt these treatment protocols, when evaluating edentulous patients or patients with terminal dentition, having a systematic treatment-planning protocol to follow is most beneficial. When treating these patients, use of an implant-supported prosthesis is advantageous to preserving the remaining alveolar bone.
Implant- Vs. Tissue-Supported Prosthesis
Several prosthetic treatment options are available for the reconstruction of missing dentition in fully edentulous patients. These include conventional complete dentures; implant-retained, tissue-supported removable overdentures (IRTS); and implant-retained, implant-supported fixed prostheses (IRIS).17 Presently, the IRIS fixed prosthesis is very common and a well-accepted treatment for the physiologic rehabilitation of completely edentulous patients. The IRIS fixed prosthesis reintroduces internal loading of the alveolus, thereby halting its further atrophy.
In contrast, the IRTS overdenture does not load the edentulous alveolus, because the implant components are designed to only engage and prevent the "lifting off" of the overdenture from the edentulous ridge. Patients with IRIS prostheses report higher levels of satisfaction in terms of esthetics, phonetics, and functionality compared to patients with conventional or IRTS removable prostheses.18-21
To treat patients with IRIS prostheses, the anatomic limitations of the edentulous maxilla and mandible must be taken into consideration. Understanding these anatomic limits allows the clinician to determine the optimal A-P distribution of implants, minimizing cantilever length and thereby achieving favorable force distribution of the fixed implant-supported prosthesis.22,23
Anatomic Limitations
The edentulous maxilla has a unique anatomic presentation that may limit the installation of the appropriate number and distribution of implants within the alveolar ridge. The maxillary sinuses bilaterally and the position of the nasal floor in the premaxillary region often limit the vertical volume of alveolar bone available for placement of axial implants for a fixed, implant-supported prosthesis. Typically, large pneumatized sinuses in this group of patients require extensive bone grafting with conventional implant placement. On the other hand, tilted implants may be used to avoid grafting procedures, serving as a predictable treatment option, especially for patients seeking a fixed provisional prosthesis immediately following surgery.5,7
To aid in the treatment planning of the edentulous maxilla, radiographic evaluation of the presence or lack of radiographic zones 1, 2, and 3, as described by Bedrossian et al,24,25 should be cconsidered. The surgical and restorative team can devise a preliminary treatment plan based on analysis of these radiographic results. In complex or near-complex situations, 3-dimensional (3D) radiographic evaluation may also be necessary to confirm the preliminary conclusions.
In the resorbed edentulous mandible, limitations for implant placement are due to the presence of the mental foramina as well as the minimal height of bone available over the inferior alveolar nerve in the posterior. The fixed mandibular prosthesis, therefore, has traditionally been supported by osseointegrated implants placed in the intraforaminal edentulous alveolus of the mandibular symphysis, a technique that was first described by Brånemark et al in the early 1980s.26
In 2011, in their finite element paper Fazi and colleagues described the various intraforaminal positions for placement of implants in the reconstruction of the edentulous mandible.27 Based on the results of their study, four implants, including two distal implants tilted by 34 degrees, yielded the best distribution of occlusal forces under loading because the A-P distribution of the implants allowed for the prosthesis with the shortest cantilever.
To immediately load a full-arch prosthesis, it is recommended that the osteotomy be undersized to allow for insertion torque of 32 Ncm or greater.28 The progressive tapering of a self-cutting implant that enables lateral compression of the bone upon insertion of the implant is a major contributor to implant stability when implant loading is considered.29 The use of such an implant along with either a straight or angulated screw-retained abutment (SRA) can help facilitate the fabrication of an immediate-load provisional restoration for loading the implant at the time of placement.
Case 1: Edentulous Maxillary Fixed Treatment Concept
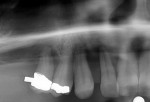
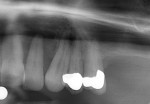
A 51-year-old woman presented with a nonrestorable terminal dentition in her maxillary arch (Figure 1 and Figure 2). After extensive clinical and radiographic evaluation, the decision was made to remove all of her remaining upper teeth and adopt a graftless approach (Straumann® Pro Arch, Straumann, straumann.com) with immediate loading of her maxillary arch. The treatment was planned accordingly.
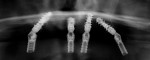
Planning the position and distribution of the implants along the length of the maxillary arch began with the evaluation of the zones of the maxilla. The presence of bone in zones 1 and 2 in the premaxilla and the bicuspid regions, respectively, along with the lack of bone in zone 3, the molar region (Figure 3 and Figure 4), directed the treatment team to consider the tilted Pro Arch concept. This is a concept that is synonymous with a "tilted" or "all-on-four" concept.
Radiographic evaluation also demonstrated significant loss of alveolar housing around the existing teeth. With this radiographic confirmation of bone loss the treatment team was able to anticipate that upon removal of the patient's teeth a composite defect (ie, lack of teeth and hard and soft tissues) would be present.24,25 Therefore, the final prosthetic design was a fixed hybrid prosthesis.
In preparation for the procedure, the patient was premedicated with 2 grams of amoxicillin 1 hour before the procedure. (Author's note: If the patient is allergic to penicillin, 600 mg of clindamycin may be administered instead). After administration of intravenous sedation and local anesthesia, an envelope flap was established exposing the underlying alveolar bone. The teeth were extracted atraumatically and the residual edentulous alveolar bone was recontoured to allow for a smooth, flat surface to establish complementary contact topography with the intaglio surface of the planned provisional fixed prosthesis. As treatment-planned, appropriate bone reduction was performed to allow for adequate interarch space for the planned hybrid prosthesis.
To aid in the proper trajectory of the anterior as well as posterior implants, this procedure entails performing a 2.2 mm osteotomy in the midline to stabilize the Pro Arch guide. Using the vertical lines on the guide, the 2.2 mm osteotomy was prepared and the guide pins placed. After confirmation of the proper depth and angulation of the premaxillary implants, the guide pins were removed and sequential drills were used to complete the preparation of the osteotomy to receive the planned 4.5 mm implants (Straumann® BLX, Straumann). Angled lines on the Pro Arch guide assisted the surgeon in preparing the posterior angled osteotomies to receive the tilted implants.
All four implants, at site Nos. 3, 7, 10, and 13, were placed with the drilling unit set at 20 Ncm and 800 RPM. Typically with this procedure, as the implant is inserted, with proper preparation of the undersized osteotomy, the handpiece will stall and the drilling unit then gets set at 40 Ncm. The continuous increase in the thread diameter of the BLX implant laterally compresses the cancellous bone and, at approximately 1 mm to 2 mm before complete insertion of the implant, the drilling unit should stall again indicating the implant is now placed at 40 Ncm. The remaining 1 mm to 2 mm of the implant is then inserted using a manual torque wrench, with close attention paid to maintaining the proper trajectory of the implant into the established osteotomy.
Creating an undersized osteotomy is critical to enabling the implant to be inserted at 40 Ncm. The progressive widening and thick thread design of the particular implant used in this case allows for the lateral compression of the cancellous bone and insertion of the implant with adequate initial stability for immediate loading. Additionally, the portfolio of this particular implant features a uniform implant platform dimension regardless of the thread diameter. This characteristic affords the surgeon flexibility when selecting the implant diameter to achieve initial stability, as the available angled and straight SRAs will fit the implant regardless of the thread diameter.
After placement of all four implants, the SRAs were attached. For the posterior implants, 30-degree SRAs were used and torqued to 35 Ncm (Figure 5 through Figure 7). For the anterior implants, straight SRAs were used and torqued to 35 Ncm. Protective caps were then screwed onto the SRAs, and the patient's full upper denture was relieved to allow it to be completely seated against the patient's palate. Once the denture was adequately relieved and its complete seating confirmed, registration paste was placed into the intaglio surface, the denture was reinserted into the patient's mouth, and its proper seating was confirmed by having the patient close in centric occlusion.
An acrylic bur was then used to create a hole through the denture following the indexed positions of the SRAs in the intaglio surface of the denture. The protective caps were then removed. Temporary abutments were attached to the SRAs, and the denture was seated back into the patient's mouth, with care taken to ensure 1 mm to 2 mm clearance around the temporary abutments prior to luting the cylinders to the patient's denture.
A fast-setting copolymer acrylic material (Qyk-Set, Holmes Dental, holmesdental.com) was used to attach the temporary abutments to the denture. After the acrylic cured completely, the denture was unscrewed from the SRAs. The palatal portion of the denture was removed, and the flange was beveled toward the soft tissue of the alveolar ridge, which allowed a cleansable contour for the provisional fixed prosthesis.
After the provisional was polished and all sharp edges removed, it was secured to the SRAs with prosthetic screws. The full upper denture, which was fabricated preoperatively, was at this point directly converted to a fixed, implant-supported provisional hybrid prosthesis. Teflon tape was placed into the screw-access channels and sealed using flowable composite. Bilateral equal occlusion was established in group function. The patient's provisional is represented in Figure 8; note that the transition line was hidden, and the occlusion was stable. Figure 9 through Figure 11 depict cone-beam computed tomography (CBCT) imaging of the final position of the implants.
At 1-week postoperative the patient's recovery was uncomplicated. For postoperative instructions, the patient should maintain a soft diet during the 6-month osseointegration period, avoiding any tearing motion and hard foods; and the patient should immediately report to the implant team if the prosthesis becomes loose. Good cross-arch stabilization of the implants by the prosthesis is critical for their osseointegration in immediate-load full-arch rehabilitations.15
With this protocol, for maxillary treatments patients are usually scheduled for stage II evaluation at 6 months; for mandibular cases, 3 months. The provisional is removed at the stage II appointment, and abutment screw stability is confirmed by gentle application of 35 Ncm torque. Lack of sensitivity and mobility confirms osseointegration, and now impression-taking and the initiation of the prosthetic protocol for fabrication of the final hybrid fixed prosthesis may begin.
Case 2: Edentulous Mandibular Fixed Treatment Concept
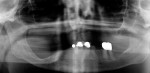
A 92-year-old woman presented with an ill-fitting mandibular partial denture and nonrestorable remaining mandibular teeth. She had a significant unilateral saddle deformity from having lost the dentition in her right posterior mandibular quadrant many years ago (Figure 12). Desiring a stable and nonremovable type of appliance, the patient was seeking treatment of the mandible with a fixed prosthesis.
After plans were made for the removal of the remaining teeth as well as an alveoloplasty to establish adequate interarch space for the planned fixed hybrid prosthesis, ie, enable better adaptation to the intaglio surface of the prosthesis, 4.5 mm implants (Straumann® BLX) were planned for intraforaminal placement. To minimize posterior cantilevers, the two distal implants were treatment-planned in the tilted, Pro Arch approach. The four implants were placed at site Nos. 21, 24, 26, and 29. The insertion torque on all four implants was at 40 Ncm following the same surgical protocol as used for the aforementioned maxillary case. Angulated SRAs were placed on the posterior implants and straight SRAs on the anterior implants and torqued to 35 Ncm.
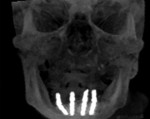
Intraoral, direct conversion of a newly fabricated full lower denture to a fixed provisional prosthesis was completed after placement of temporary abutments onto the SRAs (Figure 13). Upon completion of the conversion of the denture to a fixed, implant-supported provisional, bilateral equal occlusion was established and verified by clinical examination (Figure 14). Figure 15 and Figure 16 depict CBCT imaging of the final position of the implants.
Conclusion
These two cases demonstrated the science and properties of a contemporary dental implant system designed for achieving initial stability to facilitate immediate loading. The protocol enables fewer surgical appointments and allows the avoidance of bone grafting for a highly efficient and minimally invasive treatment of edentulous patients as well as those with terminal dentition. The approach used is favorable for achieving proper distribution of implants, establishing optimal A-P distribution to eliminate or minimize posterior cantilevers. Offering positive physiologic outcomes for patients, including maintenance of residual alveolar bone volume, an implant-supported fixed prosthesis may lend itself to higher treatment acceptance by edentulous and terminal dentition patients.
Disclosure
Dr. Edmond Bedrossian periodically lectures on behalf of Straumann but received no compensation for this article.
About the Authors
Edmond Bedrossian, DDS
Director, Implant Training, Alameda Medical Center, University of the Pacific, San Francisco, California; Honorary Member, American College of Prosthodontists; Private Practice, San Francisco, California
Edmond Armand Bedrossian, DDS, MSD
Masters in Prosthodontics, University of Washington School of Dentistry, Seattle, Washington; Private Practice, San Francisco, California
References
1. Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: a mixed-longitudinal study covering 25 years. 1972. J Prosthet Dent. 2003;89(5):427-435.
2. Cawood JI, Howell RA. Reconstructive preprosthetic surgery. I. Anatomical considerations. Int J Oral Maxillofac Surg. 1991;20(2):75-82.
3. Christensen GJ. The advantages of minimally invasive dentistry. J Am Dent Assoc. 2005;136(11):1563-1565.
4. Papaspyridakos P, White GS, Lal K. Flapless CAD/CAM-guided surgery for staged transition from failing dentition to complete arch implant rehabilitation: a 3-year clinical report. J Prosthet Dent. 2012;107(3):143-150.
5. Mattsson T, Köndell PA, Gynther GW, et al. Implant treatment without bone grafting in severely resorbed edentulous maxillae. J Oral Maxillofac Surg. 1999;57(3):281-287.
6. Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res. 2006;17 suppl 2:35-51.
7. Kim KS, Kim YL, Bae JM, Cho HW. Biomechanical comparison of axial and tilted implants for mandibular full-arch fixed prostheses. Int J Oral Maxillofac Implants. 2011;26(5):976-984.
8. Gibney JW. Minimally invasive implant surgery. J Oral Implantol. 2001;
27(2):73-76.
9. Scotti R, Pellegrino G, Marchetti C, et al. Diagnostic value of NobelGuide to minimize the need for reconstructive surgery of jaws before implant placement: a review. Quintessence Int. 2010;41(10):809-814.
10. Fortin T, Bosson JL, Isidori M, Blanchet E. Effect of flapless surgery on pain experienced in implant placement using an image-guided system. Int J Oral Maxillofac Implants. 2006;21(2):298-304.
11. Balshi SF, Wolfinger GJ, Balshi TJ. Surgical planning and prosthesis construction using computed tomography, CAD/CAM technology, and the Internet for immediate loading of dental implants. J Esthet Restor Dent. 2006;18(6):312-325.
12. Brodala N. Flapless surgery and its effect on dental implant outcomes. Int J Oral Maxillofac Implants. 2009;24 suppl:118-125.
13. Erickson DM, Chance D, Schmitt S, Mathis J. An opinion survey of reported benefits from the use of stereolithographic models. J Oral Maxillofac Surg. 1999;57(9):1040-1043.
14. Misch CE. Short dental implants: a literature review and rationale for use. Dent Today. 2005;24(8):64-68.
15. Krekmanov L, Kahn M, Rangert B, Lindström H. Tilting of posterior mandibular and maxillary implants for improved prosthesis support. Int J Oral Maxillofac Implants. 2000;15(3):405-414.
16. Schramm A, Gellrich NC, Schimming R, Schmelzeisen R. Computer-assisted insertion of zygomatic implants (Brånemark system) after extensive tumor surgery [in German]. Mund Kiefer Gesichtschir. 2000;4(5):292-295.
17. Raghoebar GM, Meijer HJ, Stellingsma K, Vissink A. Addressing the atrophied mandible: a proposal for a treatment approach involving endosseous implants. Int J Oral Maxillofac Implants. 2011;26(3):607-617.
18. Guckes AD, Scurria MS, Shugars DA. A conceptual framework for understanding outcomes of oral implant therapy. J Prosthet Dent. 1996;
75(6):633-639.
19. Att W, Stappert C. Implant therapy to improve quality of life. Quintessence Int. 2003;34(8):573-581.
20. Att W, Bernhart J, Strub JR. Fixed rehabilitation of the edentulous maxilla: possibilities and clinical outcome. J Oral Maxillofac Surg. 2009;67(11 suppl):60-73.
21. van Steenberghe D. A retrospective multicenter evaluation of the survival rate of osseointegrated fixtures supporting fixed partial prostheses in the treatment of partial edentulism. J Prosthet Dent. 1989;61(2):217-223.
22. Silva GC, Mendonça JA, Lopes LR, Landre J Jr. Stress patterns on implants in prostheses supported by four or six implants: a three-dimensional finite element analysis. Int J Oral Maxillofac Implants. 2010;25(2):239-246.
23. Bevilacqua M, Tealdo T, Menini M, et al. The influence of cantilever length and implant inclination on stress distribution in maxillary implant-supported fixed dentures. J Prosthet Dent. 2011;105(1):5-13.
24. Bedrossian E, Sullivan RM, Fortin Y, et al. Fixed-prosthetic implant restoration of the edentulous maxilla: a systematic pretreatment evaluation method. J Oral Maxillofac Surg. 2008;66(1):112-122.
25. Bedrossian E, Bedrossian EA. Systematic treatment planning protocol of the edentulous maxilla for an implant-supported fixed prosthesis. Compend Contin Educ Dent. 2019;40(1):20-25.
26. Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416.
27. Fazi G, Tellini S, Vangi D, Branchi R. Three-dimensional finite element analysis of different implant configurations for a mandibular fixed prosthesis. Int J Oral Maxillofac Implants. 2011;26(4):752-759.
28. Ottoni JM, Oliveira ZF, Mansini R, Cabral AM. Correlation between placement torque and survival of single-tooth implants. Int J Oral Maxillofac Implants. 2005;20(5):769-776.
29. Wang L, Aghvami M, Brunski J, Helms J. Biophysical regulation of osteotomy healing: an animal study. Clin Implant Dent Relat Res. 2017;
19(4):590-599.