A One-Stage Procedure to Achieve Predictable Implant Placement and Guided Bone Regeneration
Robert J. Miller, DMD
Abstract: Advancements in implant dentistry have led to increased predictability in bone augmentation procedures, resulting in fewer complications and larger bone yields. As demonstrated in this case report, one such innovation, the Straumann® AlloGraft Ring, enhances the clinician's ability to place a dental implant in a restoratively driven fashion with simultaneous guided bone regeneration.
It is estimated that more than 40% of all dental implants placed require some form of hard-tissue augmentation to ensure predictable osseointegration and a restoratively driven placement.1 As a result, several innovations in guided bone regeneration have been introduced. These range from advances in barrier membranes; to changes in the type, size, and preparation of bone and particulate; to the use of biologics; and enhancements in implant surface technology.2,3 These innovations have made augmentation procedures far more predictable resulting in fewer complications and larger bone yields.
The Straumann® AlloGraft Ring (Straumann, straumann.com) is an advancement that has led to an increase in predictability and the ability to place a dental implant in a restoratively driven fashion with simultaneous guided bone regeneration.4,5 Use of this novel technique has been successful from both a procedural standpoint and a practice management perspective.6 Patients are far more likely to consent to a single surgery versus two surgical procedures, which is typical for sites demonstrating advanced horizontal or vertical ridge defects.
Case Report
Clinical Presentation
The patient was a 69-year-old wo-man who presented with mild systemic disease, including hypertension and thyroid disease. She was taking amlodipine and levothyroxine (Synthroid®) to control these issues. Also, she was currently smoking more than a pack of cigarettes per day and was classified as ASA II.
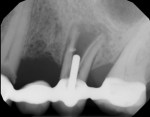
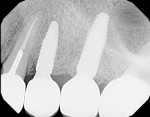
The patient's chief concern was a failing bridge in the upper left posterior sextant. Tooth No. 11 was severely decayed, necessitating endodontic treatment, post, and crown to salvage. Tooth No. 13 had a vertical fracture, which left it with a hopeless prognosis (Figure 1). The treatment plan included the extraction of tooth No. 13 and placement of dental implants in position Nos. 12 and 13. Traditionally, the clinician would have considered a two-stage approach for tooth No. 13, which typically would require 3 to 6 months of hard- and soft-tissue maturation prior to implant placement.
Medical clearance was obtained from the patient's physician, and the patient and clinician had a lengthy discussion about the higher failure rate of dental implants as well as reduced yield with guided bone regeneration in smokers versus nonsmokers before she consented to proceed with the treatment.
Implant Surgery
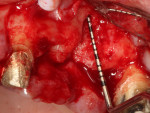
The surgery was performed using the standard aseptic surgical protocol. Full-thickness flap elevation from teeth Nos. 11 through 14 was necessary to expose position No. 12, enable extraction of tooth No. 13, and adequately debride the socket, with removal of any soft-tissue remnants (Figure 2). A large buccal dehiscence lesion was noted, which was a result of the fractured bicuspid (Figure 3).
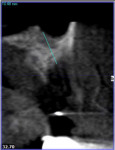
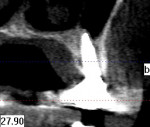
The area was irrigated with 0.12% chlorhexidine gluconate, and a cone-beam computed tomography (CBCT) was exposed to determine if implant placement using an allograft ring was an option. The scan revealed that an implant could be placed in a restoratively driven fashion utilizing the apical native bone, which would stabilize the fixture and allograft ring (Figure 4). Sinus involvement was ill-advised due to the patient's smoking addiction. It was decided to use a Narrow Connection Straumann® Bone Level Tapered Implant in position No. 12 and a Regular Connection Straumann® Bone Level Tapered Implant in position No. 13, necessitating the use of a 7-mm diameter Straumann® AlloGraft Ring. Standard surgical protocol was followed in the preparation of the osteotomy for the allograft ring and implant. This included identifying the appropriate site, marking it with round burs, and drilling to depth with a 2.2-mm diameter twist drill. A 7-mm trephine with copious irrigation was used to create the osteotomy, and a planator was used to flatten the floor.
The allograft ring fit snugly into the osteotomy site (Figure 5) and was further stabilized by the apical threads of the dental implant (Figure 6). Good initial stability was attained, giving the clinician confidence that a successful outcome would be achieved (Figure 7). Straumann® Particulate XenoGraft was placed on the buccal aspect of the allograft ring (Figure 8), and a Straumann® Membrane Flex™ collagen membrane was used to cover the site to ensure osseointegration and maximize the graft yield. Tension-free primary closure was attained using a vertical release and horizontal mattress suturing (Figure 9).
Post-surgery
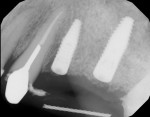
Healing was uneventful. A full 6 months was allowed for hard- and soft-tissue maturation (Figure 10). An implant stability quotient (ISQ) value (Osstell, osstell.com) of 68 for the grafted site was noted at stage II, which is very good for type IV bone (Figure 11). The final restorations were fabricated, consisting of four individual units for teeth Nos. 11 through 14 (Figure 12). The periapical x-ray taken shortly after delivery of the prosthetics depicted osseointegrated implants in position Nos. 12 and 13 (Figure 13). The CBCT revealed that the implant in position No. 13 was well positioned and demonstrated complete regeneration of the buccal plate (Figure 14).
Conclusion
The Straumann® AlloGraft Ring provides clinicians with the unique opportunity to perform-and patients the opportunity to receive-simultaneous implant placement and guided bone regeneration predictably as a one-stage procedure in sites in which this would not be possible using many of the conventional techniques available. Patient acceptance and success have been gratifying.
About the Author
Robert J. Miller, DMD
Private Practice, Plantation, Florida; Fellow, International Team for Implantology (ITI)
References
1. Bornstein MM, Halbritter S, Harnisch H, et al. A retrospective analysis of patients referred for implant placement to a specialty clinic: indications, surgical procedures, and early failures. Int J Oral Maxillofac Implants.2008;23(6):1109-1116.
2. Schwarz F, Herten M, Sager M, et al. Bone regeneration in dehiscence-type defects at chemically modified (SLActive) and conventional SLA titanium implants: a pilot study in dogs. J Clin Periodontol. 2007;34(1):78-86.
3. Wilson TG Jr, Miller RJ, Trushkowsky R, Dard M. Tapered implants in dentistry: revitalizing concepts with technology: a review. Adv Dent Res. 2016;28(1):4-9.
4. Giesenhagen B, Martin N, Donkiewicz P, et al. Vertical bone augmentation in a single-tooth gap with an allogenic bone ring: clinical considerations. J Esthet Restor Dent. 2018;30(6):480-483.
5. Benlidayi ME, Tatli U, Salimov F, et al. Comparison of autogenous and allograft bone rings in surgically created vertical bone defects around implants in a sheep model. Clin Oral Implants Res. 2018. doi: 10.1111/clr.13379.
6. Miller RJ, Korn RJ, Miller RJ. Use of the Straumann® AlloGraft Ring with simultaneous implant placement: a novel approach. Compend Contin Educ Dent. 2017;38(11):1-7. https://www.aegisdentalnetwork.com/cced/2017/11/use-of-the-straumann-allograft-ring-with-simultaneous-implant-placement-a-novel-approach. Accessed May 8, 2019.