Possible Complications With Implant Site Development Utilizing Orthodontic Extrusion: Three Case Reports
Philip Y. Kang, DDS; and Ramy Habib, DDS, MPH
Abstract: Orthodontic extrusion or forced eruption has been a treatment modality used to improve future implant sites. A controlled force exerted on a tooth in a coronal direction can enhance both soft-and hard-tissue dimensions of implant recipient sites. However, this seemingly simple and effective treatment may, in fact, result in the loss of bone rather than gain if orthodontic mechanics are used improperly. Such unfavorable outcomes have been discussed in the literature along with various proposed techniques to overcome these poor results. This article is intended to evaluate these techniques and their results by elucidating possible reasons for complications in orthodontic extrusion cases. Also, mechanical aspects of orthodontic extrusion, such as various methods of bracket positioning and wire usage, will be discussed through a report of three clinical cases.
The first report of the use of an orthodontic eruption dates back to 1940 when Oppenheim performed an artificial elongation procedure through the eruption with concomitant apposition of bone.1 A series of key articles in orthodontic literature by Reitan showed that as a tooth erupts, there is a continual apposition of bone at the root apex and around the alveolar crest as the periodontal ligament fibers are stretched.2-5 In a case of orthodontic movement into an area of periodontal defect, Brown showed reduced pocket depths, increased attachment apparatus, and change in both hard- and soft-tissue architecture.6
Another important discovery came in the 1970s when Batenhorst and others confirmed that as the soft tissue follows the erupting tooth, an increase in the width of attached gingiva occurs without the location of the mucogingival junction changing.7 Around this time, Ingber published a series of classic articles on the efficacy of forced eruption, showing it could be used to eliminate intrabony osseous defects,8 improve crown-to-root ratio of teeth when combined with crown lengthening surgery,9 or enhance cosmetic results by correcting irregular gingival margin locations.10
In terms of implant site development, in 1993 Salama and Salama proposed the concept of "orthodontic extrusive remodeling" in which hopeless teeth were extruded to gain bone around the area where implants would later be placed.11 In the late 1990s, the term "orthodontic extraction" was introduced, whereby teeth were extruded to the point of extraction.12 Other peer-reviewed publications on forced eruption/orthodontic extrusion and implant site development soon followed.13-16
Subsequently, in a systematic review by Korayem et al, 18 articles were studied, and all showed clinical significant gain in alveolar bone and gingival tissue. The authors concluded that orthodontic extrusion of hopeless teeth prior to implant placement appears to be a viable alternative to conventional surgical augmentation procedures.17
Some detrimental complications as a result of improper use of orthodontic mechanics, however, have been observed clinically. Hochman et al discussed such unfavorable outcomes and proposed different techniques to overcome these results.18 Therefore, the intent of this article is to evaluate the results of the Hochman study by elucidating possible reasons for complications in orthodontic extrusion cases. This article also will discuss the mechanical aspects involved in this treatment modality, such as various methods of bracket positioning and wire usage, through a report of three clinical cases in which forced eruption was utilized. The first case involves implant site development, and the other two cases illustrate increasing clinical crown length.
Case 1
The patient presented with a chief complaint that her "front crown is loose" and she wanted "to fix it." Tooth No. 8 had a defective porcelain-fused-to-metal (PFM) crown with an underlying post that had loosened during function. The remaining root under the defective PFM had an intrabony pocket of 6 mm mesially. Based on clinical and radiographic examinations, tooth No. 8 was given a nonrestorable, hopeless prognosis.
The patient had a relatively high lip line with a midline discrepancy and a diastema between her central incisors. She said the diastema had been present her entire life and that an attempt by a previous dentist to correct it with a composite veneer about 4 years prior had a relatively unsuccessful outcome. She desired that the diastema be closed and had a high expectation for a good esthetic outcome.
First, a provisional restoration was fabricated on tooth No. 8 and composite build-up was placed on tooth No. 9 to close the diastema. Considering the periodontal status and position of tooth No. 8, along with the patient's high esthetic expectations, a decision was made to orthodontically extrude the remaining root of No. 8 in order to eliminate the osseous defect and gain additional soft and hard tissue in an effort to enhance future implant placement.
The case is depicted from baseline to post-stabilization in Figure 1 through Figure 5. Figure 1, taken at the initial phase of orthodontic extrusion, shows a composite build-up on the mesial aspect of tooth No. 9 and a new provisional restoration on tooth No. 8 to mimic final restorations with the diastema closed. Brackets were placed and 0.016 nitinol wire was used to activate the movement (Figure 2). After 1 week, the tooth started to move about 1 mm (Figure 3), and the movement became more obvious at 1 month and 2 months post-activation (Figure 4). Incisal reduction on the provisional restoration was performed to create sufficient inter-incisal clearance. Following orthodontic movement the tooth was stabilized for an additional 2 months to facilitate tissue maturity (Figure 5).
Radiographic changes during the tooth movement are shown in Figure 6. During the first 2 weeks, the periodontal ligament space widened and the coronal advancement of the root became more apparent when comparing the level of the root apex with that of the adjacent teeth. At the end of the forced eruption period, a complete resolution of the mesial osseous defect was observed and, furthermore, a reverse bony architecture was created interproximally.
In a comparison of Figure 1 (at initial phase) and Figure 5 (at stabilization phase) a gain of 3 mm of gingival tissue can be seen at tooth No. 8. Also, the radiographs confirmed coronal growth of interproximal bone around the tooth. There was a concern, however, regarding root prominence (Figure 7), which had become apparent at about 1-month post-activation. A bone-sparing extraction was performed atraumatically, carried out carefully with a periotome. Upon evaluation of the socket, clinical observation revealed that the facial alveolar wall was absent (Figure 8). Thus, the procedure was aborted and a ridge preservation procedure was performed instead.
Case 2
The patient presented for a crown lengthening procedure from teeth Nos. 6 through 11 to improve overall esthetics. Upon examination it was noted that only a small amount of natural tooth structure was present above the alveolar crest on tooth No. 8 and the future restoration would not have had enough ferrule. To achieve a successful esthetic outcome, the remaining root was orthodontically extruded for 3 mm using a round 0.018 nitinol wire. Figure 9 and Figure 10 show the initial and post-orthodontics radiographs, respectively, after 2 months of movement. After stabilization, a crown lengthening surgery was performed, during which the facial plate of tooth No. 8 was able to be evaluated. Figure 11 depicts an obvious lack of facial alveolar bone on No. 8. Additionally, as can be seen in the occlusal view in Figure 12, the position of the remaining root was far facial compared with the adjacent teeth.
Case 3
In this case, tooth No. 9 was orthodontically extruded using a different mechanism (Figure 13 through Figure 16). A palatal access hole was created in the acrylic provisional prosthesis through which a metal post was inserted into an endodontically treated root (Figure 14 and Figure 15). Then, an elastic was utilized to activate movement by connecting it to both the metal post from the root and a stainless-steel post that was attached at the coronal third of the crown (Figure 16). After 2 months of extrusion, a crown lengthening surgery was performed, and as can be seen in Figure 17, on the facial aspect of tooth No. 9 there was a coronal deposition of alveolar bone along the extruded root. Unlike the previous cases, when the tooth was extruded with an elastic attached to the post, the movement was parallel to the long axis of the tooth without any facial or palatal movement and the loss of facial bone was prevented.
Loss of Alveolar Facial Plate
There are several possible scenarios to consider when determining whether or not orthodontic extrusion causes the loss of alveolar bone. First, it may be that there was no bone present initially before the extrusion was attempted. In maxillary anterior regions, fenestrations or dehiscences occur frequently, especially in thin gingival biotypes.19 Second, in patients with a history of periodontal disease or orthodontic treatment, it is not uncommon to find areas with thin or missing bone. Also, during the eruption phase, if an infection develops or an inflammatory response occurs, this may damage the surrounding periodontium. Pulpal disease can also result in loss of supporting tissues, which may include facial bone. Lastly, use of improper orthodontic mechanics could be another reason for loss of facial plate after orthodontic extrusion.
Eruption Patterns
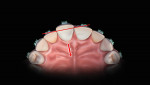
Figure 18 illustrates an ideal pattern of eruption in which the tooth emerges from the alveolus along its long axis without compressive forces in either facial or palatal vectors. However, when working around a u-shaped maxillary anterior arch with different crown positions and contours, replicating this ideal pattern of eruption is quite challenging. For example, in order to extrude a central incisor, a bracket should be positioned more apically near the cementoenamel junction (CEJ) than the brackets on anchorage teeth (Figure 19 and Figure 20). Anatomically, as can be seen from the sagittal view in Figure 19, this is where the greatest height of crown contour is located. Thus, an exaggerated occlusal view (Figure 21) illustrates how the position of the bracket is far more facial than those on the adjacent teeth, which will result in a significant anterior-posterior (A-P) discrepancy (indicated by the red line in Figure 21) between the tooth being erupted and the anchorage teeth. As a tooth is being extruded, its natural movement also will be toward the palatal direction as depicted by the arrow in Figure 21.
Often, after an initial coronal movement of a tooth (Figure 22 and Figure 23), the clinician may change the bracket position more apically to erupt the tooth even further (Figure 24). During this second phase of eruption, a bracket is actually placed onto a narrower part of the root that has been positioned palatally (Figure 25). As further eruption takes place, the reverse A-P between the tooth and anchorage teeth drive the root facially, which could result in destruction of facial plates.
From the sagittal plane (Figure 26), it is apparent that a tooth moves both coronally and palatally as the A-P discrepancy increases with the position of the bracket on the cervical bulge. Moreover, during the initial phase of eruption, the torque created around the center of resistance will exert compressive forces on the apico-facial and corono-palatal regions of the root that cause bone resorptions, as identified in the red circled areas in Figure 26. Due to the more resilient nature of palatal tissues, the root torque created at the center of resistance is accentuated facially, and simultaneously there is a continual apposition of bone around the root apex, as identified in the blue circled area in Figure 27. As mentioned previously, often times in order to erupt the root further the bracket position will be moved more apical to the narrower part of the root that had been positioned palatally. At this point, the new reverse A-P discrepancy that has been created will drive the remaining root facially, resulting in further destruction of the facial plate (Figure 28).
To summarize these events, phases of eruption patterns responsible for facial bone resorption can be divided into early, middle, and late phases. During an early phase, a facial-palatal root torque around the center of resistance results in compressive forces on apico-facial and corono-palatal regions of the root. Later, in the middle phase, as the tooth is being erupted, the apical part of the root is driven toward the facial bone. Finally, during late phase, with the bracket at a more apical position, a reverse A-P discrepancy will result in further facial movement of the root with concomitant loss of facial bone.
Proposed Mechanics
To replicate the ideal pattern of eruption, unfavorable lateral movements must be prevented. Most importantly, clinicians need to evaluate tooth position and crown contours carefully before initiating any movement. Then when a bracket is bonded, instead of it being placed too apically around the cervical bulge, it may be placed at a more coronal position for activation that reduces the A-P discrepancy. Minor enameloplasty around the area may sometimes help. The type of wire used is also crucial in terms of controlling the amount of forces exerted on the tooth being erupted. Initially, use of a soft, flexible wire is recommended to minimize lateral forces as much as possible. Rectangular wires may help control unwanted torques while simultaneously providing auxiliary torques with bends and/or loops, depending on the situation. However, the latter technique will require far more skill than using round wire, and the authors highly recommend that clinicians work with orthodontists for those types of complex situations.
Elastics also may be used to extrude the tooth out of the alveolus if there are no compressive forces created on adjacent tissues. Hooks or buttons may be used in conjunction with elastics, and sometimes a Hawley-type appliance can be worn to extrude the tooth along its long axis. Whichever mechanics are used, careful frequent re-evaluation of tooth roots while movement is in the active phase of therapy is a critical aspect of orthodontic treatment.
Conclusion
Forced eruption is a safe and effective treatment to improve a future implant recipient site. However, a careful evaluation of the tooth position, crown, and contours before any movement occurs is critical for optimal results. Appropriate use of mechanics and materials such as brackets, wires, and elastics is also essential for successful orthodontic treatments. Referral to an expert in orthodontics should always be considered.
About the Authors
Philip Y. Kang, DDS
Assistant Professor, Division of Periodontics, Section of Oral, Diagnostic and Rehabilitation Sciences, Columbia University College of Dental Medicine,
New York, New York
Ramy Habib, DDS, MPH
Former Resident in Postgraduate Periodontics, Division of Periodontics, Section of Oral, Diagnostic and Rehabilitation Science, Columbia University College of Dental Medicine, New York, New York
References
1. Oppenheim A. Artificial elongation of teeth. Am J Orthod Oral Surg. 1940;26(10):931-940.
2. Reitan K. The initial tissue reaction incident to orthodontic tooth movement as related to the influence of function; an experimental histologic study on animal and human material. Acta Odontol Scand Suppl. 1951;6:1-240.
3. Reitan K. Tissue rearrangement during retention of orthodontically rotated teeth. Angle Orthod. 1959;29(2):105-113.
4. Reitan K. Effects of force magnitude and direction of tooth movement on different alveolar bone types. Angle Orthod. 1964;34(4):244-255.
5. Reitan K. Clinical and histologic observations on tooth movement during and after orthodontic treatment. Am J Orthod. 1967;53(10):721-745.
6. Brown IS. The effect of orthodontic therapy on certain types of periodontal defects. I. Clinical findings. J Periodontol. 1973;44(12):742-756.
7. Batenhorst KF, Bowers GM, Williams JE Jr. Tissue changes resulting from facial tipping and extrusion of incisors in monkeys. J Periodontol. 1974;45(9):660-668.
8. Ingber JS. Forced eruption. I. A method of treating isolated one and two wall infrabony osseous defects-rationale and case report. J Periodontol. 1974;45(4):199-206.
9. Ingber JS. Forced eruption: part II. A method of treating nonrestorable teeth-periodontal and restorative considerations. J Periodontol. 1976;47(4):203-216.
10. Ingber JS. Forced eruption: alteration of soft tissue cosmetic deformities. Int J Periodontics Restorative Dent. 1989;9(6):416-425.
11. Salama H, Salama M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: a systematic approach to the management of extraction site defects. Int J Periodontics Restorative Dent. 1993;13(4):312-333.
12. Celenza F. The development of forced eruption as a modality for implant site enhancement. Alpha Omegan. 1997;90(2):40-43.
13. Mantzikos T, Shamus I. Case report: forced eruption and implant site development. Angle Orthod. 1998;68(2);179-186.
14. Mantzikos T, Shamus I. Forced eruption and implant site development: an osteophysiologic response. Am J Orthod Dentofacial Orthop. 1999;115(5):583-591.
15. Buskin R, Castellon P, Hochstedler JL. Orthodontic extrusion and orthodontic extraction in preprosthetic treatment using implant therapy. Pract Periodontics Aesthet Dent. 2000;12(2):213-219.
16. Zuccati G, Bocchieri A. Implant site development by orthodontic extrusion of teeth with poor prognosis. J Clin Orthod. 2003;37(6):307-311.
17. Korayem M, Flores-Mir C, Nassar U, Olfert K. Implant site development by orthodontic extrusion: a systematic review. Angle Orthod.2008;78(4):752-760.
18. Hochman MN, Chu SJ, Tarnow DP. Orthodontic extrusion for implant site development revisited: a new classification determined by anatomy and clinical outcomes. Semin Orthod. 2014;20(3):208-227.
19. Ochsenbein C, Ross S. A reevaluation of osseous surgery. Dent Clin North Am. 1969;13(1):87-102.