A Vibration Device to Control Injection Discomfort
Jeffry R. Shaefer, DDS, MS, MPH; Stephanie J. Lee, BS; and Nina K. Anderson, PhD
Abstract
Pain from local anesthesia injections can be reduced by distraction and counter-stimulation techniques. This study investigated the DentalVibe® Injection Comfort System (third-generation, DV3), developed to lessen anesthesia pain through pulsed vibration, a form of counter-stimulation. The aim of the study was to evaluate both the efficacy of DV3 in reducing pain and discomfort from intraoral long buccal (LB) and inferior alveolar nerve (IAN) injections and the time needed to achieve complete anesthesia during an IAN block. The study enrolled 60 subjects, 30 men and 30 women, aged 21 to 32 years, who rated both injection pain on a visual analog scale and discomfort, unpleasantness, and difficulty in enduring the injection on a modified symptom severity index. Each subject received bilateral LB injections and an IAN block. Using block design, the third-generation DV (DV3) was randomly assigned to either the first or second LB injection and to 30 subjects on their third injection, the IAN block. No topical anesthesia was applied. Subjects receiving DV3 reported significantly less pain, discomfort, unpleasantness, and difficulty in enduring LB and IAN injections (P < .05), regardless of whether DV3 was used on the first or second LB injection. Time to complete anesthesia was not significantly different (P > .05) when DV3 was used on IAN block injections. The DV3 significantly (P < .02) reduced pain/discomfort from anesthetic injections in this pilot study, in which many subjects were either dental or medical students familiar with performing and enduring injections. More studies are warranted on layperson populations.
Managing pain and controlling anxiety during dental treatment is critical to successful patient care. For patients, the pain and anxiety induced by the injection of local anesthetic agents can be reduced by topical analgesics, distraction techniques, counter irritation, limiting the speed of injection, buffering, and the use of vibration as a technique of counter irritation/stimulation.1-11 Vibration techniques are based on the gate-control theory of Melzack and Wall.12 This theory states that pain transmission through A delta (lightly myelinated nerves with impulse conduction speed of ~ 20 meters/second) and C nociceptive fibers (unmyelinated nerves with impulse conduction speeds of ~ 2 meters/second) is depressed at the secondary neuronal cell bodies in the dorsal horn if nerve impulses evoked by tactile sensation are simultaneously transmitted through A beta tactile fibers (thickly myelinated nerves with impulses traveling at ~ 75 meters/second).12-14 This effect is attributed to the stimulation of inter-neurons to block the transmission of sensation via A delta and C fiber neurons.12-14
Vibrating devices attached to the dental syringe to decrease pain from local anesthesia via a gate-control phenomenon, such as the syringe micro vibrator and the Vibraject (Vibraject EU, vibraject.eu), have been introduced in recent years with mixed results.15,16 Transcutaneous electrical nerve stimulation (TENS) devices have been reported to be effective in decreasing pain from maxillary buccal infiltration anesthesia but not during palatal injections.17 Hutchins and coworkers18 found no difference in the perception of pain by patients when using vibration to enhance the effectiveness of topical anesthesia. Nanitsos and colleagues investigated the effect of vibration of the local soft tissue on pain during local anesthesia injections and found that injections with vibration resulted in lower pain ratings by patients.19 The DentalVibe® Injection Comfort System (DV) (DentalVibe, dentalvibe.com) (Figure 1) uses pulsed vibration to reduce the perception of pain during local anesthesia administration.20 As large proprioceptive A beta fibers generally adapt rapidly to stimulation but are readily re-activated by a change in stimulus, the pulsed vibration of the DV maintains the A beta fiber activation and closure of the gate for perception of small pain fibers.12 The DV is a cordless and rechargeable handheld device that delivers pulsed, percussive micro-oscillations stimulating the sensory receptors within the oral mucosa at the site where an intraoral injection is being administered.21 Studies have shown the DV to be effective in reducing discomfort from maxillary infiltration anesthesia.21-24 Ching and coworkers21 investigated the effect of the DV device on adolescent patients. In their study, the patients were administered topical 20% benzocaine before each injection. One half of the patients in the study received injections with the DV turned on and the other half of the patients received injections with the device turned off (control group). All injections were supraperiosteal (infiltration) injections as the DV significantly reduced the pain from these injections. Anecdotal experience identifies the maxillary supraperiosteal injections done in the study by Ching as relatively easy for dental patients to tolerate when compared with inferior alveolar nerve (IAN), long buccal (LB), or palatal injections. In that study, the infiltration anesthesia was in the posterior areas of either the maxilla or mandible bilaterally, without distinction of how many subjects had anesthesia in the maxilla or mandible. No difference in the age or sex of the subjects or in the sequencing of injections was found. Elbay and coworkers,23 employing the first-generation DV device, used a split-mouth design in their study of supraperiosteal maxillary and mandibular injections in 60 adolescents. The study subjects received injections on one side of their mouths, then 5 days later, received injections on the opposite side. The investigators found no difference in pain reduction between the traditional supraperiosteal injections and those supplemented with the use of the DV. The DV device uses a lower frequency, amplitude, and pulse rate than the third-generation DV (DV3) model. In another study, Difelice and colleagues25 found a significant effect from the DV3 when anesthetizing 20 subjects presenting for same-day periodontal scaling procedures who received bilateral IAN blocks using topical anesthesia with or without the use of the DV3. They did not document whether the DV3 was used with the first or second injection. The goal of the present study was to evaluate the efficacy of DV3 in reducing pain/discomfort from same-day intraoral LB and IAN injections, and the time needed to achieve complete anesthesia during an IAN block without the concurrent use of topical anesthesia. The authors hypothesized that DV3 would reduce pain/discomfort caused by injections and the time necessary for complete anesthesia.
Specific Aims
This study had three specific aims. One was to measure the effectiveness of the mediation of injection discomfort by the DV3 device without using topical anesthetic during an intraoral LB block compared with routine operator manipulation (defined as the operator manipulating the subject's jaw with his fingers, stimulating regional proprioceptive fibers as much as possible, and providing a distraction stimulus). Secondly, the authors wanted to measure how the DV3 mediates injection discomfort without the use of topical anesthetic during an IAN block compared with routine operator manipulation. Finally, the study sought to measure how the DV3 affects time necessary to achieve complete anesthesia during an IAN block. No attempt was made to “hide” the use of the DV3, which is why the DV3 was used first with half of the subjects and second with the other half of the subjects.
Methods
Sixty volunteers were recruited from the Harvard University medical area community via medical and dental community-wide emails and poster advertisements in the medical center. Each subject had a 40-minute study appointment. On the study day, each subject was asked to complete a facial anxiety scale (FAS), which measures subjects' level of anxiety before receiving anesthetic injections; a zero rating indicates no anxiety, while a rating of 10 indicates extreme anxiety.26 Also, each subject's positive response to a cold test of tooth No. 22 (left mandibular canine) was recorded. If tooth No. 22 was missing or endodontically treated, then a positive response to a cold test on tooth No. 23 (left mandibular lateral incisor) was recorded instead. Each subject was then given bilateral LB injections with a 27-gauge needle of 0.5 cc of 3% mepivicaine (Polocaine®, Dentsply Sirona, dentsplysirona.com) without vasoconstrictor. The DV3 device was used during this study. Each subject received one injection while the DV3 was used and also received one injection without the DV3 being used. The use of the DV3 was randomized in the following manner: it was used with the first injection on the right mandible of the first study subject and then its use on either the right or left mandible was alternated for every other subsequent study subject thereafter.
For each injection with the DV3, the device was placed (Figure 2) on the tissue to be injected for approximately 10 seconds before the injection, and the needle was placed as close as possible to one of the vibrating tips of the DV3.20 After each injection, the contact and vibration of the DV3 was maintained on the tissue for an additional 5 seconds. For the LB injection, the tips of the DV3 were placed at the level of the occlusal plane distal to the second molar in the retromolar pad area between the external and internal oblique bony ridges. If the subject had a third molar present, the LB injection was given buccal to the third molar. After both LB injections, the subject was then given a left IAN block with a 27-gauge needle of 1.8 cc of 3% mepivicaine (Polocaine) without vasoconstrictor. Whether to use the DV3 with the IAN injection was decided by selecting a piece of paper from a box of 60 papers marked either with or without DV3. When the subject was injected without the use of the DV3 (the control injection), the operator manipulated the jaw with his fingers to stimulate regional proprioceptive fibers as much as possible and to provide a distraction stimulus. This is the routine operator manipulation referred to in the study's specific aims. After each injection, the subject was asked to rate the pain from the injection by using the visual analog scale (VAS) and to rate the intensity and intolerability of the injection by using a modified symptom severity index (SSI).
The length of time necessary for the subject to obtain complete mandibular anesthesia after the IAN injection was recorded by an investigator blinded from knowing if the DV3 was used concurrently with the injection. Complete mandibular anesthesia was confirmed by a negative response to a cold test on tooth No. 22 (or tooth No. 23 if tooth No. 22 was found to be missing or endodontically treated during study intake) after the subject reported a completely numb left lower lip. Post-injection surveys and time necessary for complete IAN anesthesia was recorded by the same evaluator who was blinded from knowing if the DV3 was used concurrently with the injection. The authors note that they prefer a cold test over electric pulp testing because they believe it is the more reliable clinical method to determine tooth responsiveness.
Outcome Measures
Visual Analog Scale
The VAS is used to subjectively measure the acute pain intensity felt by the subject from each injection. It allows patients to self-rate their pain on a visual horizontal grading scale of 0 to 10. The reliability of the VAS has been proven in multiple studies conducted with appropriate internal controls.27
Symptom Severity Index
The modified SSI is a global multidimensional measure of symptom severity and includes visual analog scales for sensory and affective intensity, frequency and duration of symptoms, tolerability of symptoms, and a symptom checklist to measure scope of symptomatology.28 Because the symptom checklist portion records a symptom as positive if a subject has had the symptom in the past 6 months, its score remained static throughout the post-injection evaluation period of this study and was, therefore, not included in the SSI scores. Also, for this study, because the frequency and duration of discomfort during the subject's injection experience was not pertinent to assessing the efficacy of the DV3, these two SSI measures were not recorded. Each SSI subjective measure has a line with 28 spaces anchored with “zero” pain intensity, unpleasantness, and effort to endure on the left and “worst imaginable” pain, unpleasantness, and effort to endure on the right (Figure 3). The subject is asked to mark the space on the line that corresponds to the level of that symptom that they experienced with the injection.
Time to Complete Anesthesia
Time was measured in minutes from when the IAN block anesthesia was administered to when the subject no longer felt a cotton pellet cooled by endodontic ice on tooth No 22 (or tooth No. 23 if No. 22 was missing or endodontically treated).
Sample Size Estimation
Sample size estimation was based on data from Nanitsos and coworkers19 from the result of a paired t test comparing the rating of pain by the subject with and without the addition of vibration to an anesthetic injection. Using the P value obtained from the t test with 61 degrees of freedom, the t statistic was calculated to be 4.365. From a mean difference of 9.3, the standard deviation was calculated as 16.66 for an effect size of 0.558. This effect size generated that a sample size of 44 subjects, each receiving two injections (one with DV3 and one without), is necessary to attain 95% power for a paired t test comparing the two pain measures at a two-tailed alpha level of 0.05.
No data was available on time to effect of the anesthetic injection; therefore, no reasonable sample size estimate for this hypothesis was possible. Statistical analyses were performed using statistical software SPSS v22 (IBM, ibm.com). Descriptive statistics included ranges, means, measures of dispersion (standard deviation, variance), parametric statistics (eg, analyses of variance, Pearson coefficient of association), and nonparametric chi-square. Two-tailed significance levels were set at P < .05. IRB approval for this study (IRB14-2778) was granted by the Harvard Medical School Institutional Review Board.
Results
Data was obtained from 60 subjects, 30 men and 30 women, aged 21 to 32 years (mean age, 25 ± 2.25). Forty-five (75%) were predoctoral dental students, with the remainder medical, art, and other students. There were no significant gender differences for any of the outcome measures.
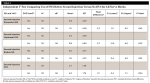
Independent T Test for Receiving DV3
For the group not receiving DV3 concurrently with the first injection, the mean scores for discomfort, unpleasant, endure, and VAS were higher than for subjects receiving DV3 (Table 1). Similarly, the subjects receiving DV3 concurrently with the second injection had significantly lower scores for discomfort, unpleasant, endure, and VAS (Table 2). There were no group differences in time to reach complete mandibular anesthesia (numb time). Half the subjects received DV3 concurrently with IAN, half did not. As expected, the subjects receiving DV3 had significantly lower scores for discomfort, unpleasant, endure, and VAS (Table 3).
Although there were no significant differences in the mean numb time between the groups receiving DV3 and not receiving DV3, there were significant differences in the pattern of associations among discomfort, unpleasant, endure, and VAS (Table 4). For the subjects who did not receive DV3 concurrently with the first injection, numb times were positively correlated with levels of discomfort, unpleasant, endure, and VAS.
Clinical recommendations for patients with high anxiety (having a low tolerance for dental pain and/or dental treatment) and/or compromised medical health are to schedule such patients for morning rather than afternoon appointments, keep appointments short, and ensure excellent control of pain and anxiety during their treatment. For this subject group, 17 participated in the morning and 43 in the afternoon. Independent t test did not reveal any significant difference in measures of injection (1, 2, or 3) discomfort, unpleasant, endure, VAS, numb time, or FAS based on time of day that the injection was given (P > .05). Also, there was no influence of the level of pretreatment anxiety on discomfort scores with or without the use of DV3. Independent t tests were used to determine if there were any differences across the dental students. Students from years one and two (D1/2) were compared with students from years 3 and 4 (D3/4).
Significant differences were found for FAS and first injection discomfort. The D1/2 students reported significantly higher FAS (2 ± 2.09 vs 0.95 ± 1.11; P = .046) than the D3/4 students. For first injection discomfort, the D3/4 scores were significantly higher than the D1/2 scores (8 ± 3.99 vs 5.8 ± 3.05; P = .055).
Discussion
This randomized single-blinded clinical trial assessed the use of vibration during the administration of dental anesthesia, which was given for the purpose of the study and not for dental treatment of the subject. The primary advantage of performing anesthetic injections that are not required for dental treatment of the subject is that bilateral LB infiltration injections (with and without the use of DV3) could be done on the same day, thereby reducing daily confounding factors, such as poor sleep, stress, etc, that could affect the response of the subjects to and assessment of the experience. The LB injection was chosen because it is a relatively quick and easy-to-perform injection that produces a local area of numbness, the effects of which can be assessed almost immediately by both the subject and investigator. The LB injection is also administered in a region where the tissues are difficult for dental anesthetists to manipulate to stimulate the injection area to reduce patient discomfort unless using a device such as the DV3. The subjects also were given an IAN block injection after the LB injections on just one side of their jaw (left side was used for all subjects). This was done unilaterally so that the subject experienced numbness only on one side of the jaw for the 60- to 90-minute duration of the anesthetic. A shorter-acting anesthetic was used for all injections to limit the length of time the subjects experienced numbness. The authors investigated the IAN block, as that is an injection that dentists have difficulty administering comfortably and effectively, with a success rate reported as low as 67%.29,30
Bilateral identical injections with and without the DV3 were given so as to allow the individual subject to immediately decide on the effectiveness of the DV3 compared with not using it. The single IAN injection (nerve block) given allowed an assessment on how the DV3 influences the time for onset of complete anesthesia and how effective the device is in reducing pain and discomfort in a group of subjects compared with another group who had an IAN injection without the use of the DV3. Standard identical injection techniques were used with and without the DV3. When used, the device was placed on the tissue at the location of the injection for approximately 10 seconds before the injection, and the needle was placed as close to one of the DV3 probes as possible. When the subject was injected without the use of the DV3, the operator manipulated the jaw with his or her fingers stimulating regional proprioceptive fibers as much as possible and to provide a distraction stimulus. This was done in a routine manner, typically performed by dentists administering anesthesia. The use of DV3 did not influence the time for complete anesthesia (P > .05), but the findings of this study clearly indicate that its usage can reduce discomfort from dental anesthesia. The reduction of anesthesia discomfort would possibly be more profound in a cohort of routine dental patients as compared with the subjects in this study who were primarily dental students.
Discomfort from an intraoral dental injection is related to both the prick of the needle penetrating the mucosa and distension pressure of the tissues as the anesthetic enters the submucosa. The standard method to reduce pain from dental injections is the pretreatment use of topical anesthetic. Benzocaine is a frequently used topical anesthetic agent in dental clinics.31 It has been shown to work well in supraperiosteal (infiltration) injections done in the maxilla; however, its anesthetic effect is not profound when used with an IAN block.32 Despite the ineffectiveness of topical anesthetic agents for IAN injections, most dental practitioners will use one when administering IAN injections to meet the patient's expectations for use of such an anesthetic. IAN injections are commonly considered the most difficult for dental patients to endure, so the use of the topical medication could help to modulate the patient's pre-anesthesia anxiety. A 2006 study by Al-Melh and coworkers showed that application of topical anesthesia before needle prick using a combination of 2.5% lidocaine and 2.5% prilocaine (L/P) as either a creamy mixture (EMLA, Akorn, akorn.com) or a gel (Oraqix, Dentsply Pharmaceutical, dentsply.com) was significantly (P < .05) more effective than 20% benzocaine gel in reducing pain from a palatal injection with a 27-gauge needle.31 Al-Melh and colleagues only measured needle insertion stimuli without injection of anesthetic (ie, the stimulation of anesthetic solution passing into the tissue, which has been recognized as being directly related to the patient's level of injection pain,33 was not present). An advantage to using an L/P topical anesthetic was found to be that it was less bitter tasting and was odorless,31 which are qualities that can increase the comfort of the patient during dental anesthesia. In the present study, topical anesthetic was not used, but the discussion of how pre-anesthesia anxiety affects how the patient perceives injection discomfort is important in the authors' analysis of the effectiveness of the DV3, especially for a patient with anxiety concerning dental treatment.
Rosivack and colleagues34 studied the pain experience during dental anesthesia of 109 adults who were treated at a dental phobia clinic, a large proportion of whom were found to be prone to injection fear. The researchers investigated the pharmacologic and psychological processes that play a role when topical anesthesia is used to reduce the pain of dental injections. Subjects were assigned to one of two belief conditions: half of the subjects were told they would receive a placebo, while the others were told they would receive the active agent. However, all subjects actually received two separate injections at contralateral sites, one preceded by a placebo and the other by a 20% benzocaine gel. The order in which injections were given was associated with differences in pain report. Second injections were more painful than first injections. The present authors also had similar findings for the second LB injections in the present study (Table 4). Rosivack and colleagues34 found that whether injections were preceded by an active agent or a placebo, the pain experienced by the subject was not altered. Likewise, their belief manipulation did not affect the pain report. Subjects who believed they would receive the active agent, however, had significantly less pain than subjects who thought they would receive a placebo. The widespread belief that topical anesthetics are effective at reducing injection pain may serve to reduce the anticipatory anxiety associated with an impending dental injection, thus making the injection experience more tolerable.35-37 van Wijk and Hoogstraten24 also found that when they used a standard injection technique, injection pain was significantly associated with their subjects' pre-anesthesia anxiety. The findings of Ching and coworkers21 during their use of the DV with adolescents confirmed that its effect was seen to be increased in relation to the pain rating from the injection without the DV, indicating that the more discomfort a patient experiences during an injection or possibly the more anxiety he or she has concerning dental treatment the greater effect a pain reduction technique such as the DV can have. Ching and colleagues accordingly found a higher reduction of perceived pain with the DV in subjects with a higher pain response during their control injection. Their finding agrees with the findings of Palm and colleagues,33 who investigated the effect of pain during mandibular block injections using the Wand® (Wand Dental Inc., thewand.com) and who found a significantly greater reduction in perceived pain with the Wand in patients with a higher pain perception during traditional injection.
Because dental anxiety influences an individual's reaction to dental treatment, knowledge of the patient's level of dental anxiety should alert the provider to tailor the treatment to meet the patient's needs. The present study results indicate that use of the DV3 significantly reduces the pain of dental anesthesia in injections that are difficult for patients to tolerate. But, contrary to the study results, the authors did not find that the level of a patient's pretreatment anxiety (as determined by the FAS) was associated with increased pain during the dental injection, nor did it influence DV3 effectiveness. Only six of the subjects in the present study had moderate or severe anxiety, making an association of anesthesia discomfort levels to pre-anesthesia anxiety difficult. One would expect that the more phobic a patient is the greater potential for effect a pain reduction device such as a DV3 would have, whether or not it is a definitive effect or a placebo effect such as the use of topical anesthetic during an IAN block.
A limitation of this study is that the majority of subjects were medical and dental students familiar with performing and enduring injections and who could be perceived as having decreased anxiety concerning dental anesthesia as compared with a typical dental patient. In fact, the third-year students who participated in the study had just received anesthesia training, which involved administering dental anesthesia on each other. One could expect that, overall, given their recent anesthesia training these dental students would be less anxious concerning the procedures used in this study. The fact that the first- and second-year dental students had more pretreatment anxiety than the third- and fourth-year students supports this assumption. Interestingly, though, three of the subjects with high pre-injection anxiety were third-year dental students. This underscores the point that a patient's previous dental experience may continue to influence his or her anticipation of dental anesthesia, despite recent positive experiences or desensitizing procedures. Overall, the subjects in the present study had relatively low levels of anxiety.
The subjects in this study were not blinded to the use of the DV3 during their injections, so the possibility of a placebo effect in influencing the subjects' perceptions of their injections could be considered a limitation to this study. Only the study evaluators were blinded to whether or not the subjects were anesthetized with the use of the DV3. But, as previously discussed, the patients' pre-anesthesia levels of anxiety influence their perception of anesthesia discomfort. Whether a reduction of anesthesia discomfort is related to a placebo effect, an actual physiological blocking of the C fiber or A delta nerve pain stimulus, or both, could be considered irrelevant to the purpose and outcome of this study: that is, does the DV3 lessen discomfort from dental anesthesia? Difficulty in blinding a subject to the use of DV3 should be recognized. One could use another DV3 type of device that vibrates at a different frequency as a control device, but then one is assessing the frequency and/or intensity of the DV3 pulsations rather than the use of the device itself. The investigation of DV3 pulsation parameters should be done in a subsequent study with the DV3 to understand how changes in pulsation frequency, intensity, and duration affect nerve transmission. Once the effects of changes in pulsation characteristics on nerve transmission are understood, testing the DV3 on subjects with trigeminal neuropathy should be considered.
Conclusion
This study showed that for subjects in this study, the DV3 significantly reduced pain from dental anesthesia when used with injections that are routinely difficult for patients to tolerate, such as the LB and IAN. The use of the DV3 did not influence the time it took to achieve complete mandibular anesthesia in this cohort of subjects. The pulsed vibration provided by the DV3 seems effective for controlling patient discomfort and improving pain control during the administration of dental anesthesia. The DV3 device could also be considered for use in medical practices when local anesthesia is used without sedation, as the use of vibration to prevent discomfort from cutaneous injection has been reported in two clinical trials, one that involved taking blood in a pediatric population and the other involving eyelid surgery.38-40 Pain control during procedures that cause discomfort, such as joint manipulation, wound cleaning, or bandage removal, that are routinely done without the use of local anesthesia could also benefit from the counter-stimulation effect of pulsed vibration. The role that the DV3's unique pulsation frequency plays in controlling pain transmission warrants further investigation.
DISCLOSURE: This study was financially supported by DentalVibe Inc. (dentalvibe.com).
About the Authors
Jeffry R. Shaefer, DDS, MS, MPH
Assistant Professor, Department of Oral and Maxillofacial Surgery, Harvard School of Dental Medicine, Boston, Massachusetts
Stephanie J. Lee, BS
Dental student, Harvard School of Dental Medicine, Boston, Massachusetts
Nina K. Anderson, PhD
Instructor, Developmental Biology, Harvard School of Dental Medicine, Boston, Massachusetts
References
1. Weisenberg M. Psychological intervention for the control of pain. Behav Res Ther. 1987;25(4):301-312.
2. Dworkin SF. Integrating behavioral and pharmacological therapeutic modalities. Anesth Prog. 1986;33(1):29-33.
3. Pollack S. Pain control by suggestion. J Oral Med. 1966;21(2):89-95.
4. Aminabadi NA, Farahani RM, Balayi Gajan EJ. The efficacy of distraction and counterstimulation in the reduction of pain reaction to intraoral injection by pediatric patients. J Contemp Dent Pract. 2008;9(6):33-40.
5. Touyz LZ, Lamontagne P, Smith BE. Pain and anxiety reduction using a manual stimulation distraction device when administering local analgesia oro-dental injections: a multi-center clinical investigation. J Clin Dent. 2004;15(3):88-92.
6. Fitton AR, Ragbir M, Milling MA. The use of pH adjusted lingnocaine in controlling operative pain in the day surgery unit: a positive randomized trial. Br J Plast Surg. 1996;49(6):404-408.
7. Kakigi R, Shibasaki H. Mechanisms of pain relief by vibration and movement. J Neurol Neurosurg Psychiatry. 1992;55(4):282-286.
8. Yarnitsky D, Kunin M, Brik R, Specher E. Vibration reduces thermal pain adjacent dermatomes. Pain. 1997;69(1-2):75-77.
9. Weerakkody NS, Percival P, Hickey MW, et al. Effects of local pressure and vibration on muscle pain from eccentric exercise and hypertonic saline. Pain. 2003;105(3):425-435.
10. Dahlin L, Lund I, Lundberg T, Molander C. Vibratory stimulation increase the electro-cutaneous sensory detection and pain thresholds in women but not in men. BMC Complement Altern Med. 2006;6:20.
11. Zoppi M, Voegelin MR, Signorini M, Zamponi A. Pain threshold changes by skin vibratory stimulation in healthy subjects. Acta Physiol Scand. 1991;143(4):439-443.
12. Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150(3699):971-979.
13. Sufka KJ, Price DD. Gate Control Theory reconsidered. Brain Mind. 2002;3(2):277-290.
14. Melzack R. Recent concepts of pain. J Med. 1982;13(3):147-160.
15. Hashem A, Bonjar S. Syringe micro vibrator (SMV) a new device being introduced in dentistry to alleviate pain and anxiety of intraoral injections, and a comparative study with a similar device. Ann Surg Innov Res. 2011;5(1):1.
16. Saijo M, Ito E, Ichinohe T, Kaneko Y. Lack of pain reduction by a vibrating local anesthetic attachment: a pilot study. Anesth Prog. 2005;52(2):62-64.
17. Meechan JG, Winter RA. A comparison of topical anaesthesia and electronic nerve stimulation for reducing the pain of intra-oral injections. Br Dent J. 1996;181(9):333-335.
18. Hutchins HS Jr, Young FA, Lackland DT, Fishbourne CP. The effectiveness of topical anesthesia and vibration in alleviating the pain of oral injections. Anesth Prog. 1997;44(3):87-89.
19. Nanitsos E, Vartuli R, Forte A, et al. The effect of vibration on pain during local anaesthesia injections. Aust Dent J. 2009;549(2):94-100.
20. DentalVibe 3-in-1 Injection Comfort System. https://www.dentalvibe.com. Accessed May 10, 2017.
21. Ching D, Finkleman M, Loo CY. Effect of the DentalVibe injection system on pain during local anesthesia injections in adolescent patients. Pediatr Dent. 2014;36(1):51-55
22. Ungor C, Tosun E, Dayisoylu EH, et al. The effects of vibration on pain and anxiety during local anesthesia administration. JSM Dent. 2014;2(1):1022.
23. Elbay ÜS, Elbay M, Yildirim S, et al. Evaluation of the injection pain with the use of DentalVibe injection system during supraperiosteal anaesthesia in children: a randomized clinical trial. Int J Paediatr Dent. 2015;26(5):336-345.
24. van Wijk AJ, Hoogstraten J. Anxiety and pain during dental injections. J Dent. 2009;37(9):700-704.
25. Difelice MG, Vandewalle KS, Maller SC, Hancock RH. Effects of a vibratory device on pain from anesthetic injections. Compend Contin Educ Dent. 2014;35(4):246-251.
26. Hockenberry MJ, Wilson D. Wong's Essentials of Pediatric Nursing. 8th ed. St. Louis, Mo: Mosby; 2009.
27. Miller MD, Ferris DG. Measurement of subjective phenomena in primary clinical care research: the Visual Analogue Scale. Fam Pract Res J. 1993;13(l):15-24.
28. Shaefer JR, Jackson DL, Schiffman EL, Anderson QN. Pressure-pain thresholds and MRI effusions in TMJ arthralgia. J Dent Res. 2001;80(10):1935-1938.
29. Malamed SF. The Gow-Gates mandibular block: evaluation after 4275 cases. Oral Surg Oral Med Oral Pathol. 1981;51(5):463-467.
30. Johnson TM, Badovinac R, Shaefer J. Teaching alternatives to the standard inferior alveolar nerve block in dental education: outcomes in clinical practice. J Dent Educ. 2007;71(9):1145-1152.
31. Al-Melh M, Andersson L, Behbehani E. Reduction of pain from needle stick in the oral mucosa by topical anesthetics: a comparative study between lidocaine/prilocaine and benzocaine.
32. Meechan JG. Effective topical anesthetic agents and techniques. Dent Clin North Am. 2002;46(4):759-766.
33. Palm AM, Kirkegaard U, Poulsen S. The wand versus traditional injection for mandibular nerve block in children and adolescents: perceived pain and time of onset. Pediatr Dent.
34. Rosivack RG, Koenigsberg SR, Maxwell KC. An analysis of the effectiveness of two topical anesthetics. Anesth Prog. 1990;37(6):290-292.
35. Martin MD, Ramsay DS, Whitney C, et al. Topical anesthesia: differentiating the pharmacological and psychological contributions to efficacy. Anesth Prog. 1994;41(2):40-47.
36. Kincheloe JE, Mealiea WL Jr, Mattison GD, Seib K. Psychophysical measurement on pain perception after administration of a topical anesthetic. Quintessence Int. 1991;22(4):311-315.
37. Nakanishi O, Haas D, Ishikawa T, et al. Efficacy of mandibular topical anesthesia varies with the site of administration. Anesth Prog. 1996;43(1):14-19.
38. Fayers T, Morris DS, Dolman PJ. Vibration-assisted anesthesia in eyelid surgery. Ophthalmology. 2010;117(7):1453-1457.
39. Inal S, Kellecci M. Relief of pain during blood specimen collection in pediatric patients. MCN Am J Matern Child Nurs. 2012;37(5):339-345.
40. Eichhorn MG, Karadsheh MJ, Krebiehl JR, et al. Vibration for pain reduction in a plastic surgery clinic. Plast Surg Nurs. 2016;36(2):63-68.