Interdisciplinary Treatment Planning in Transitioning a Periodontally Hopeless Dentition: A Clinical Case Review
Bozidar “Bole” Kuljic, DDS
Abstract:
Treating patients with advanced periodontal disease may require staged treatment that utilizes various modalities. In this case report, a patient with a high-risk periodontal condition lacked the financial means to receive optimal treatment immediately. The interdisciplinary team was able to provide a solution that addressed immediate needs and provide stability in the short term by retaining teeth that could be maintained for a limited amount of time until a long-term solution using implant-retained prostheses could be provided.
Decreasing risk in a dentition with advanced periodontal disease presents a great challenge for both dentist and patient. For the patient, confronting the reality of transitioning from a natural, hopeless dentition to a removable prosthesis is likely the greatest oral change he or she will ever experience.1 Psychological distress and functional concerns due to the loss of teeth and the need to adapt to a new and diminished chewing system are compounded by additional challenges, such as a decreased sense of taste and temperature. It is critical that the treating clinician have a thorough and frank discussion with the patient explaining the differences between, the nuances of, and the expectations involved with chewing with natural teeth versus dentures.2 Additionally, a full understanding of the differences between tissue-borne and implant-retained dentures will help patients make an educated choice for their future.
The following case demonstrates a way of staging treatment by using different modalities to treat a patient with advanced periodontal disease. While reducing overall risk and improving the prognosis should always drive treatment decisions, orthodontics and restorative dentistry can provide a means to delay and stage the ultimate loss of periodontally involved teeth and provide acceptable interim outcomes.3
Clinical Case Review
Patient History and Chief Complaint
A 54-year-old woman presented with a chief complaint that she was unable to eat properly. She added that she was self-conscious of her upper teeth because they were shifting and moving, and was also concerned about a missing front tooth in her lower jaw (Figure 1 through Figure 3). As an employee at a local grocery store, she had a limited discretionary income. Throughout her life, she had irregular dental visits that were usually prompted by pain and often resulted in extraction.
The patient had been to the practice 1 year earlier to treat pain in tooth No. 21. The tooth was treated with root canal therapy, a core build-up, and a full-coverage crown. At the time, the patient was informed she had advanced periodontal disease and was advised to schedule a comprehensive treatment plan appointment to address the hopeless prognosis of numerous teeth (Figure 4 through Figure 6). She appeared to understand and stated that she was not surprised by the diagnosis; however, she did not return to the practice until 1 year later.
The patient was otherwise healthy without any medical conditions or contraindication to dental care, so her medical risk was deemed low and the prognosis good.
Diagnosis, Risk Assessment, and Prognosis
Periodontal: The examination revealed severe bleeding upon probing throughout the patient’s dentition. Probing depths were in the range of 5 mm to 8 mm around teeth Nos. 7 through 10 and 30. Radiographic bone loss greater than 4 mm existed throughout the mouth, with intrabony defects found on teeth Nos. 7 through 10, 28, and 30. Teeth Nos. 7 through 10 had Class 3 mobility, while teeth Nos. 6, 24, 28, and 30 exhibited Class 1 mobility. Gingival recession of more than 2 mm was noted on teeth Nos. 6 through 8, 11, 20, 22, 24, 28, and 30.
Risk: High
Prognosis: Poor, with teeth Nos. 7 through 10 and 30 hopeless
Biomechanical: Upon clinical examination, two acceptable amalgam restorations were found. The filling on tooth No. 28 had a small overhang, while tooth No. 30 had an extensive amalgam restoration that compromised the structural integrity of the tooth. There was no indication of active caries.
Risk: Moderate
Prognosis: Fair
Functional: The patient had minimal attrition. Secondary occlusal traumatism was noted on teeth Nos. 22, 24, and 28. Clinical examination revealed the presence of a unilateral click on the right side upon opening. Due to the absence of the posterior teeth, the patient had developed a collapsed bite with a loss of vertical dimension (Figure 7). The initial diagnosis was occlusal dysfunction.
Risk: Moderate
Prognosis: Fair
Dentofacial: In repose, teeth Nos. 7 and 8 were labially positioned in comparison to the adjacent teeth (Figure 8). The upper lip was found to have medium dynamics, whereas the lower lip exhibited high dynamics.
Risk: Medium to High
Prognosis: Poor
Treatment Goals
Following a discussion with the patient about the high-risk periodontal condition of her teeth, while being mindful and sensitive to her financial, esthetic, and functional concerns, the clinician and patient developed treatment goals together. The treatment goal for the mandibular arch was to stabilize the periodontal disease and create a favorable condition for the positioning of future restorative work. In the maxillary arch, the goal was to treat the periodontally hopeless situation by removing all remaining teeth and allowing the bone and tissue to heal, thereby establishing a stable, healthy environment for the placement of implants. The prosthetic plan was for the fabrication of an implant-retained, full maxillary denture with a stable, second-premolar occlusion with the lower arch.
Treatment Plan
With the patient’s input, the following treatment plan was developed, to be carried out in phases.
• Remove all remaining upper teeth and fabricate an immediate full denture.
• Extract tooth No. 30 and perform limited orthodontic treatment in the lower arch.
• Place four tissue-level implants in the upper arch and one bone-level implant in the lower arch.
• Fabricate an upper implant-retained full denture.
• Place an implant-retained abutment and crown at No. 29.
• Create a direct composite pontic to temporarily fill the space of missing tooth No. 23.
Treatment Phases
Phase 1: Extractions, Immediate Denture, and Orthodontics
In the first phase of treatment, all maxillary teeth were removed and an immediate complete denture was delivered, thereby lowering the patient’s periodontal risk in the maxillary arch. This treatment followed all the necessary record taking and pre-delivery appointments required to ensure a successful result. Additionally, tooth No. 30 was removed, which lowered the patient’s biomechanical risk from moderate to low.
The limited orthodontic treatment on the mandibular arch began at the same time as the extractions and maxillary denture delivery. The purpose of the limited orthodontic treatment was to close the gaps between the lower teeth (Figure 9) and provisionally stabilize the periodontal condition by improving the vertical load on the compromised, periodontally involved teeth.4 The orthodontic treatment also created a more optimal alignment of the teeth in the lower arch. This was deliberately planned in preparation for and gradual transition into implants, due to the periodontal risk and poor prognosis. The transition, when necessary, could be into an implant-retained fixed crown-and-bridge prosthesis or an implant-retained complete lower denture. The decision would depend on the patient’s desires and financial concerns.
Phase 2: Planning and Execution of Implant Placement
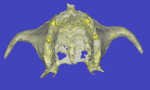
Following a 4-month waiting period from the delivery of the maxillary immediate denture, a CAT scan of the maxillary arch was taken and used with computer planning to determine the optimal location for four maxillary implants. The plan was to place the implants in the positions of the canines and second premolars (Figure 10). Anatomical landmarks, particularly in the maxillary arch, usually do not allow for parallelism of implants. However, the attachments used in this case (Locator™, ZEST Anchors, www.zestanchors.com) provide some allowance for the expected divergence, though achieving as much parallelism as possible between the implants when placed is still ideal (Figure 11). The more parallelism there is between the implants, the easier the seating of the denture becomes, and there is less resultant wear of the plastic retentive gaskets that fit over the Locator attachments. Clearly, decreased wear of the gaskets will result in improved longevity and less need for replacement during the life of the prosthesis.
Once the planning was completed, four tissue-level implants were placed in the upper arch, and one bone-level implant was placed in the position of tooth No. 29.
Phase 3: Post-Orthodontics and Replacement of Tooth No. 23
After the completion of orthodontic treatment, a bonded lingual wire was placed on the lower anterior teeth. This wire accomplished three goals: (1) it served as a bonded retainer following the orthodontic treatment; (2) it acted as a periodontal splint for the periodontally compromised teeth5; and (3) it provided anchorage for the composite pontic replacing tooth No. 23.
Once the wire was in place, a direct composite pontic was bonded onto teeth Nos. 22 and 24 and the lingual wire as a temporary esthetic solution until the patient was ready to proceed with further treatment (Figure 12 and Figure 13).
Phase 4: Delivery of Final Prosthesis
In the last phase of the present treatment plan, the maxillary implant-retained denture was delivered (Figure 14), as were the implant abutment and porcelain-fused-to-metal crown on tooth No. 29. The occlusal vertical dimension was greatly improved following the limited orthodontics (Figure 15), and the patient was able to enjoy the benefits of a much more efficient and healthy masticatory system6 until she could have the mandibular arch restored with a fixed, implant-retained option (Figure 16 through Figure 20).
Discussion
The patient understood that the existing anterior repair on the mandibular arch was a short-term solution, and that two long-term options were available to her: (1) receive an implant-retained fixed bridge extending from teeth Nos. 23 through 26, with implants in the Nos. 24 and 26 locations; or (2) opt for an implant-retained removable appliance. Both options were significantly better than a conventional removable partial or full denture. Had she chosen to have the implant-retained, fixed, four-unit bridge, she could have the mandibular arch restored with fixed, implant-retained options and avoid a removable prosthesis. This future treatment plan could be staged and phased, which is crucial for a patient on a limited budget.
An additional consideration was the high lower lip dynamics, where she showed all of the lower anterior teeth and gingival tissues during maximum smile. This presented a high esthetic risk with a fair-to-poor prognosis for the mandibular restorations.
It is challenging to preserve bone and gingival architecture for esthetic emergence profiles of pontics if the abutments are too far apart. Until the patient can continue with the optimal treatment of a four-unit fixed implant in the mandibular incisor area, the maintenance of teeth Nos. 24 and 26 is important to help preserve the crestal bone and allow for a more favorable emergence profile of her future pontics. While her dento-facial risk assessment would not change, her dento-facial prognosis and result would improve.
Conclusion
Transitioning from a natural dentition to a removable prosthesis is quite traumatic for most patients. This can be mitigated through frank discussion and careful consideration of options and expectations. Whenever possible, it is best to encourage patients to restore their broken dentitions with prostheses that are implant retained because they do not interfere with daily functions like eating, talking, and smiling as much as a tissue-borne prosthesis. Avoiding the removal of all remaining teeth at one time while staging the treatment may make the transition for patients easier. It is rare that a dentition is in such dire condition that it necessitates the removal of all remaining teeth at once. Selecting those teeth that can be maintained for a few extra years, with great cooperation and vigorous periodontal maintenance,7 can allow for staging and delivering an optimal treatment plan for the future.
For patients who are experiencing difficult financial times and are on a limited budget and cannot afford an ideal treatment plan all at once, this solution addresses immediate needs and provides stability until long-term options are attainable.
About the Author
Bozidar “Bole” Kuljic, DDS
Private Practice
Beverly, Massachusetts
References
1. Kapur KK, Soman SD. Masticatory performance and efficiency in denture wearers. J Prosthetic Dent. 2006;95(6):407-411.
2. Carlsson GE. Clinical morbidity and sequelae of treatment with complete dentures. J Prosthet Dent. 1998;79(1):17-23.
3. Gkantidis N, Christou P, Topouzelis N. The orthodontic-periodontic interrelationship in integrated treatment challenges: a systemic review. J Oral Rehabil. 2010;37(5):377-390.
4. Closs LQ, Gomes SC, Oppermann RV, Bertoglio V. Combined periodontal and orthodontic treatment in a patient with aggressive periodontitis: a 9-year follow-up report. World J Orthod. 2010;11(3):291-297.
5. Mosedale RF. Current indications and methods of periodontal splinting. Dent Update. 2007;34(3):168-170,173-174,176-178.
6. Kois JC, Phillips KM. Occlusal vertical dimension: alteration concerns. Compend Contin Educ Dent. 1997;18(12):1169-1177.
7. Zafiropoulos GG, Rebbe J. Comprehensive treatment in a case with advanced chronic periodontitis: a 15-year follow-up. Gen Dent. 2010;58(4):e149-e155.