Closing the Gap Between Esthetics and Digital Dentistry
John Weston, DDS, FAACD
Abstract:
While digital methods have a firm position in dentistry, a total digital workflow for multi-unit layered restorations has yet to be fully realized. Many clinicians are using a CAD/CAM workflow of some kind, but there is still a significant gap to be filled for completing the digital workflow. This article describes how practitioners can transition into the full digital workflow, showing the use of digital processes for anterior cosmetic cases. The pros and cons of “going fully digital” in an effort to increase efficiency while maintaining high-level quality with regards to fit and ceramics layering will be discussed.
Though many clinicians are familiar with digital technology, not a lot are using digital workflows for their high-end cosmetic practices.1 While digital methods have a firm position in the dental profession, it must be acknowledged that there are currently several limitations. Whether the limitations relate to the actual scanning process for larger cases or the design and fabrication of quality, highly esthetic veneers, a total digital workflow for multi-unit layered restorations has not been fully realized. Many clinicians are using a computer-assisted design/computer-assisted manufacturing (CAD/CAM) workflow of some kind for their everyday dentistry of single and sometimes multiple posterior crowns. However, for veneer cases, many are still taking polyvinyl siloxane (PVS) impressions, relying on a tried and true analog process.
There is certainly nothing wrong with using analog systems. Moreover, many clinicians prefer not to experiment with a digital workflow on high-end cases where patient expectations—and fees—are high. Yet, many clinicians may be unsure of where to start. There are a variety of reasons why so few clinicians are using digital workflows: some simply have not invested in the proper digital tools; some lack the experience needed; and, for many, it’s just a matter of not knowing what tools and technologies are available. The benefits of digital dentistry are obvious to most, so the question is how to bridge the gap and complete the digital workflow.
Getting Started
The first step to digitizing cosmetic cases is at the start of the process, with digital x-rays and digital photography. Whether 2-dimensional (2-D) or 3-dimensional (3-D), digital radiography is now the standard of care and is an ideal point for “jump-starting” a nondigital office. In addition, using a quality single-lens reflex (SLR) camera is also a crucial component to success with cosmetic cases.2
The next obvious move is to acquire a quality digital impression system. There are multiple systems on the market, so some research is needed. Issues to consider include the clinician’s intentions for using the system—whether it will be used for everyday single-crown dentistry or whether the digital work will include bridges, multi-unit restorations, removable prosthetics, implants, veneer cases, clear aligner therapy, and/or full-arch cases. If the latter, then a faster, smaller scanning wand that can more easily reach the posterior molars will most likely be needed to routinely complete accurate, full-arch scans quickly.3
For high-end cosmetic or multi-unit cases, the clinician will need the ability to acquire accurate printed or milled full-arch models. If the dental laboratory the office uses does not have the ability to operate a fully digital workflow, it has the option to work directly on accurate digital models that it receives pinned, trimmed, and mounted—ready for case-work fabrication via an analog process. Until virtual articulation becomes mainstream, most dentists will be mounting printed models for larger cases to refine occlusion and verify fit and finish. With a good digital impression system and accurate model fabrication process, the dentist will be able to achieve predictable results for larger cases and continue to use the existing lab to fabricate restorations that the dentist is familiar with. Either way, the results can be as good or better than traditional plaster model techniques.4 While this type of workflow is not completely digital, it represents a starting point and sets the stage for more continuous workflows as the lab and clinician develop knowledge in the digital process and acquire additional tools.
Case Presentation
This case study is an example of how digital processes can be used for anterior cosmetic cases. It will discuss the pros and cons of “going fully digital” (early adopter philosophy) versus using a partial digital workflow to increase efficiency and predictability while maintaining high-level quality with regards to fit and ceramics layering.
The patient was a healthy 29-year-old man serving active duty with the US Coast Guard. His chief complaint was that he did not like the appearance of his front teeth and wanted to improve his smile (Figure 1). He was unsure why his teeth did not “look right,” but requested that only the four upper front teeth be treated. Orthodontic consultation was denied on the basis of his at-sea deployment schedule. The author noted a healthy dentition with limited gingival inflammation and evidence of mild occlusal trauma. The main issue was that the patient exhibited a tooth/arch size discrepancy of teeth Nos. 7 through 10, with spacing between the four incisors and rotated lateral incisors. There was a large hypocalcification area on tooth No. 9 that the patient wanted repaired. The four front teeth were also positioned apically in the arch, creating a flat or almost reverse smile line. This resulted in slightly less than ideal incisal edge display with lips at rest.
Steps in the Digital Workflow
The challenge in this case was to create the proper display and smile line while keeping the teeth in correct proportion (ie, without looking too long or too wide). With regards to modern digital workflows, there are a number of steps where digital tools can help in the planning, discovery, and fabrication process. Starting in sequence from basic to more complicated, the simple list of digital tools might be considered as follows: (1) digital radiographs; (2) digital photography; (3) digital smile design; (4) digital impressions; and (5) computer-assisted restoration design, articulation, and fabrication.
While all five of these phases are available to dentists, it must be noted that they are all not yet fully adopted by everyday practitioners, though some practitioners use parts or pieces of each.1 By initiating at least some digital processes in their offices, clinicians can begin to grow with the technology before falling too far behind the curve.
To initiate the first step in planning this case, digital study photographs were made and imported into Keynote presentation software. Then, using ideal tooth proportions and positioning for anterior teeth, a design was able to be visualized that might correct the deficiencies. A calibrated ruler was used along with drawings directly on the images to communicate details of exact length and width to the ceramist.
It was determined that tooth length needed to be added to improve the smile line and increase tooth display. This required adding width as well to maintain the proper anterior tooth proportions. Whenever length is added, width should ideally be kept in proper proportion of 75% to 80% to length.5 The patient’s initial central incisor proportion started at 78%—11 mm tall by 8.5 mm wide—and was redesigned to 80%—12 mm tall by 9.5 mm wide—which remained within a normal accepted range and would solve the patient’s cosmetic concerns (Figure 2 through Figure 4).
At this point in the process, the smile design is communicated to the laboratory along with a diagnostic digital scan of the preoperative condition. The ceramist is able to use the information from the digital smile design, incorporate the desired dimensions directly into the digital diagnostic wax-up, and then print a model replicating the desired shapes and contours. Once a printed model of the digital wax-up is completed, a template can be printed or a silicone sleeve hand-pressed to facilitate the chairside transfer and “trial smile” appointment. In this case, a silicone index was made in the lab.
Trial Smile: Feedback Is Key
The trial smile appointment is a key component for a successful anterior case. It is important for the patient to see what is planned and give feedback or approval of the proposed changes. Additionally, taking digital photographs and transferring them into a premade presentation allows the patient to see a side-by-side comparison of preoperative and potential postoperative results. This visual comparison can also be emailed to the patient after the appointment.
The trial smile is equally as important for the clinician, because it allows for visualization and inspection of the planned changes in the mouth prior to making any irreversible changes to the existing dentition. Only after the trial smile is approved by the patient should a final treatment plan be formulated and appropriate time scheduled to perform the treatment (Figure 5).
On treatment day, the clinician should have his or her “preparation roadmap” ready, which includes: radiographs, reduction guides, provisional template, photographs, preoperative models, and a treatment checklist. The author uses a “case records list,” which has been created, modified, and refined over the years to help properly sequence and track the many important steps required to complete the case (Table 1).
Final Impressions
Once the prep guides were tried on, it was visually determined that minimal preparation would be required to allow space for restorative material. This was primarily because the case was mostly an additive case in which the required changes involved increasing length and width. The central incisor teeth were lingually inclined as well, which allowed additional space for ceramic and enough thickness to cover the white spot on tooth No. 9 (Figure 6). By following a restorative treatment plan based on sound smile design principles with trial smile testing, the results can be very natural and predictable, as seen in Figure 7 and Figure 8.
Final impressions were captured using the 3M™ True Definition Scanner (3M ESPE, www.3m.com) (Figure 9), a digital impression system that uses 3-D video capture and which studies show is highly accurate.6 The system’s scanning wand is small and lightweight, allowing for fast, easy full-arch capture, including posterior molars. Following full-arch scans, the upper and lower scans were virtually mounted using the bite registration scan, and the case was sent to the lab using the on-screen lab RX interface. Details about shade, material, and style of restoration can be entered into the prescription, and the stereolithography models typically arrive at the lab a few days later pinned, trimmed, and mounted (Figure 10). In the author’s experience, the digital impression approach has added efficiency to the restorative process while also providing a more comfortable experience for the patient.7
One of the advantages of digital workflows is the ability to work virtually without actual models in hand. Before the stereolithography apparatus (SLA) printed models arrive at the lab, the ceramist can begin the final restoration design using the digital STL files alone. When the files are received, margins are marked, dies are trimmed, models are sliced, and the bite is articulated—all virtually. Using the original smile design as a guide, a digital wax-up over the preparations can also be completed in just a few minutes. Compared to the analog process, where impressions have to be disinfected, poured, and mounted, and dies pinned, trimmed, and sawed apart, this provides a significant and efficient time savings.8 Having an open architecture impression system and easy STL file access can be valuable during this phase as printing methods and new materials come to market (Figure 11).
Esthetic Result With Durability
With advances in materials and techniques, clinicians are now able to make esthetic changes to anterior teeth using very thin yet durable ceramics. The material used for this case was layered lithium disilicate (e.max®, Ivoclar Vivadent, www.ivoclarvivadent.com). It was chosen to produce the desired esthetic result, with the durability that was needed.
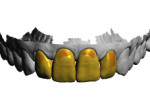
Conservative veneer restorations require a precise adaptive fit for proper bonding and long-term clinical success. In general, milled restorations have limitations with regards to fit due to the size of the milling burs and brittleness of the material. When comparing milled e.max to pressed, the difference is realized at the margins, with the pressed margins being sharper.9 As a result, the author elects not to mill final restorations but press them instead. This is a departure from a full digital workflow but justified in the author’s opinion. Because the author has seen the same internal fit issue with milled wax patterns versus printed wax patterns, the wax patterns are printed and a 0.30-mm outer reduction from full contour is included to allow for layering porcelain (Figure 12). In this case, the printed wax patterns were invested and pressed, followed by sprue removal, addition of layering porcelain, contouring, and hand polishing. The final result was esthetic restorations that fit precisely with excellent marginal adaption (Figure 13).
The veneers were seated using a total-etch technique and a 4th generation two-bottle, three-step adhesive system. The final result of this case exhibited beautiful veneers that emulate nature in every respect (Figure 7 and Figure 8). The improved proportions allowed for a more natural smile line and proper tooth display without looking unnatural. Having ideal anterior tooth length is important for effective anterior guidance and must be recognized and addressed. Because the patient had some parafunctional habits, the case was finished with a chairside anterior deprogrammer to reduce muscle activity and distribute occlusal forces on the restorations.
Conclusion
With the accuracy of intraoral scanners constantly improving, along with materials and milling and printing systems, the future outlook of complete cosmetic digital workflows is excellent. Currently, a well-defined pure digital workflow for multilayered, precise-fitting veneer restorations is not readily available to the average clinician. However, using a partial digital process such as the one described is absolutely available now and can be beneficial in many ways. The goal is to improve efficiency and predictability while maintaining quality. Taking this approach is a smart move by providers looking to sustain a strong position in the market.
Acknowledgment
The author would like to recognize his lab technician ceramist for this case, Todd Cochran, AAACD, Horizon Dental Studio, San Diego, California.
About the Author
John Weston, DDS, FAACD
Owner/Director
Scripps Center for Dental Care
La Jolla, California
References
1. Dental CAD/CAM Systems Global 2014 Market Analysis. Toronto, Ontario, Canada: Millennium Research Group; June 2014. RPGL22CC14.
2. Ludlow JB, Mol A. Digital imaging. In: White SC, Pharoah MJ. Oral Radiology: Principles and Interpretation. 6th ed. St. Louis, MO: Mosby/Elsevier; 2009:78-99.
3. Fasbinder DJ, Neiva G. Recent innovations in digital technology. Inside Dentistry. 2014;10(9):43-48.
4. Seelbach P, Brueckel C, Wöstmann B. Accuracy of digital and conventional impression techniques and workflow. Clin Oral Investig. 2013;17(7):1759-1764.
5. Bhuvaneswaran M. Principles of smile design. J Conserv Dent. 2010;13(4):225-232.
6. Boeddinghaus M, Breloer ES, Rehmann P, Wöstmann B. Accuracy of single-tooth restorations based on intraoral digital and conventional impressions in patients. Clin Oral Investig. 2015;19(8):2027-2034.
7. Yuzbasioglu E, Kurt H, Turunc R, Bilir H. Comparison of digital and conventional impression techniques: evaluation of patients’ perception, treatment comfort, effectiveness, and clinical outcomes. BMC Oral Health. 2014;14:10.
8. Burgess JO, Lawson NC, Robles A. Comparing digital and conventional impressions: assessing the accuracy, efficiency, and value of today’s systems. Inside Dentistry. 2013;9(11):68-74.
9. Anadioti E, Aquilino SA, Gratton DG, et al. 3D and 2D marginal fit of pressed and CAD/CAM lithium disilicate crowns made from digital and conventional impressions. J Prosthodont. 2014;23(8):610-617.