Immediate Provisionalization of Immediate Implants in the Esthetic Zone: A Prospective Case Series Evaluating Implant Survival, Esthetics, and Bone Maintenance
Abstract:
This prospective study evaluates immediately placed and immediately provisionalized implants in the esthetic zone. All implants were TiO2-blasted, fluoride-modified, grade 4 titanium, with a coronal microthread design. Bone grafting and guided bone regeneration (GBR) was performed at all sites, and screw-retained temporary restorations were delivered on the day of surgery. All of the provisional crown(s) were out of occlusal function and remained in place for at least 8 weeks prior to initiation of definitive restorative therapy. Bone maintenance (BM) was considered successful if radiographs demonstrated proximal bone levels even or coronal to the implant platform. Of the 29 implants placed, 25 (86%) achieved bone maintenance at least 12 months post-loading with the final restorations. This study was considered successful, with 100% implant survival after at least 1-year loading of the final restoration, and 100% of patients were satisfied with the esthetics of their implant treatment.
Esthetic expectations related to dental implant therapy are increasingly demanding. This has been precipitated by the profession’s shift from a focus on osseointegration to one on inconspicuous “esthetic integration” of the alloplastic tooth replacement into the natural dentition. In recent years, success has been achieved with hard- and soft-tissue preservation and reconstruction as well as restorative material advancements.1-3
When a patient presents with a hopeless anterior tooth or teeth, the challenge for clinicians is to provide an immediate replacement that appears to be in harmony with the surrounding natural dentition and periodontium. As implants have evolved into a preferred method of single-tooth replacement, the mode of provisionalization has changed. In the 1990s, the majority of anterior teeth extracted were temporarily replaced with removable partial dentures or “flippers.” Although this was often cosmetically acceptable, the necessity of removal for hygiene purposes and insecurity associated with mastication and dislodgement proved to be unacceptable for many patients. This temporary measure frequently prompted many patients to elect more conventional or tooth-supported temporary and final restorations. The ability to provide fixed, implant-supported provisional restorations made implant therapy more acceptable to many of these patients. The removal of an anterior tooth followed by immediate implant placement and rapid “fixed” temporization is seen as the most acceptable treatment option in most esthetically critical situations. Some investigators have advocated this modality as not only patient pleasing but also advantageous in terms of soft-tissue conditioning.4
The mode of provisionalization can be cement-retained or screw-retained. There are advantages to cement retention, most notably ease of fabrication. However, this method also has several disadvantages. The possibility of de-cementation, requiring manipulation of the abutment and soft tissues during the early healing phase, is a potential issue. Also, the possible biologic complications such as foreign body reaction and inflammation associated with cement entrapment within the peri-implant soft tissues could prove to be catastrophic. Shapoff demonstrated in case reports the destructive nature of retained cement, which can result in bone loss.5 Using a screw-retained temporary restoration eliminates the element of cement. The disadvantage of this modality, however, is that it is more challenging to fabricate this type of restoration. The angulation of anterior implants, especially maxillary anterior implants, often results in a facial or facial-incisal screw access channel, which requires that the restorative dentist have the skillset needed to “conceal” this access on the facial surface of temporary restorations (Figure 1).
There are numerous provisional restorative materials to consider; choosing the proper material for the specific situation is crucial for success. Patras et al reviewed the various materials available for certain indications.6 Proper fabrication of a screw-retained temporary restoration can minimize early complications. Complications such as fractures require removal of these screw-retained components, often before osseointegration occurs. In early studies of immediate-loading, premature removal of restoration was considered a contributory factor to implant failure.7
Occlusion is an important factor in immediate- and early-loading protocols. Providing a temporary restoration in occlusal function cannot be considered an absolute contraindication. Investigators such as Degidi et al found that multiple splinted posterior implants restored with and without occlusal contact in mandibular posterior sites performed equally.8 Anterior implant restorations differ from their posterior counterparts in that occlusal forces are typically not directed axially, but in oblique directions. This can lead to loosening of abutment screws and fracture of acrylic or composite resin veneering materials. Keeping these restorations free of occlusal contact may minimize the frequency of these complications.
In 2011, the author (Dr. Levin) published a case series evaluating implant survival and marginal bone levels of immediately placed and immediately temporized implants in the maxillary and mandibular anterior regions of the dentition.9 Modified titanium implants (SLActive®, Straumann, www.straumann.com) were followed for an average of 9 months of loading with their final restorations. Marginal bone levels were evaluated, and bone maintenance (BM) was defined as bone present at or coronal to the implant platform proximally. Of the 30 consecutively placed implants, 25 (83%) demonstrated bone maintenance.
The present study evaluates implants in similar anatomic locations. The same surgical protocol was followed. No flapless surgeries were performed. The only variation from the prior study was the implant itself. A grade 4 titanium with a fluoride-modified blasted surface (OsseoSpeed™, DENTSPLY Implants, www.dentsplyimplants.com) was used. These implants also have a coronal microthreaded portion (0.185 mm). The Straumann bone-level implants used in the previous study did not contain this microthreaded segment of the implant body. It is postulated that the microthread is responsible for BM crestally. For more than a decade, investigators have demonstrated excellent BM with this type of implant body macrotopography. Among them was Norton, who in 2001, achieved this after 4 to 7 years of loading this implant design in single-tooth replacements.10
The purpose of this prospective study is to demonstrate implant survival and BM of OsseoSpeed implants immediately placed and non-functionally provisionalized in the esthetic zone, as well as loaded for minimally 1 year with the definitive restoration.
Methods and Materials
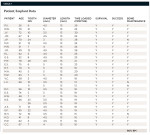
This study consisted of 27 consecutively treated patients who received 29 implants (Table 1). The age of the patients ranged from 26 to 85 years. All patients required extraction of one or more anterior teeth in the first bicuspid or mesial portion of the dentition in either the maxillary or mandibular arch. All patients were presented with alternative treatment options and signed informed consent forms explaining risks associated with implant therapy. Because no deviation from standard treatment rendered in a periodontal specialty practice existed, and the study did not involve any unapproved or special materials unique to the study, no special considerations regarding informed consent were necessary.
All patients required extractions of anterior teeth due to root fractures, untreatable caries, or advanced attachment loss. No teeth presenting with active periapical infections were included.
Once the periodontist, restorative dentist, and patient agreed to proceed with immediate placement and provisionalization, cone-beam computed tomography (CBCT) scans (Galileos, Sirona, www.sirona.com) were taken to verify the existence of 3-dimensional (3-D) bone, which is needed for favorable implant placement and primary stability. Diagnostic casts were obtained to fabricate surgical guides and facilitate provisional restorations.
After reflection of the full-thickness mucoperiosteal flaps designed to allow visualization of the facial bone while preserving proximal hard and soft tissues, the teeth were extracted with periotomes, thin elevators, and forceps. Special care was taken to avoid trauma to the facial cortex. Debridement of the extraction sockets was performed with ultrasonic and manual instruments, and a cotton pellet hydrated with tetracycline/sterile saline was placed into the cleansed socket for about 3 minutes. This step was performed empirically to chemically cleanse the fresh extraction site prior to initiation of osteotomy preparation.
The surgeon attempted to position the implants palatally, engaging palatal/lingual and apical bone in all placements. Implant diameters were selected based on the specific tooth being replaced and to avoid proximity or contact with the labial bone. The platform of the implant was inserted to a depth approximately 3-mm apical to the anticipated facial mucosal zenith of the completed restoration. Bone grafting was performed in all cases. This consisted of obturation of the residual space or horizontal defect distance (HDD) between the implant body and the inner socket wall(s). In the event of any dehiscence or fenestration, this was also grafted with a mineralized allograft (freeze-dried bone allograft [FDBA]) (LifeNet Health®, www.accesslifenethealth.org). In most situations, a thin continuous layer of graft material was also placed on the external surface of the facial cortex and a resorbable collagen membrane was adapted. The membrane consisted of either bovine type I collagen (Cytoplast® RTM Collagen, Sybron, www.sybronimplants.com) or a porcine extra-cellular matrix (DynaMatrix®, Keystone Dental, www.keystonedental.com).
Two modes of temporization—direct and indirect methods—were used in this study. The direct method consisted of fabrication of the temporary crown(s) and its insertion prior to flap closure. A temporary abutment (either TempBase or TempDesign, DENTSPLY Friadent, www.dentsply-friadent.com) was affixed to the implant, and a sterile rubber dam was placed to avoid contact between the restorative material and the underlying tissues. Then a bis-acryl material (LuxaTemp®, DMG America, www.dmg-america.com) was flowed through a vacuum-formed template to directly “pick-up” the temporary abutment (Figure 2).
Final contouring was then performed extraorally on an implant replica with the addition of flowable composite resin. The restoration could be tried in directly onto the implant and modified. Abutment screws would be hand-tightened once esthetic and occlusal goals were achieved, and the facial flap was sutured around the provisional crown.
The indirect method included identical steps to the direct method in terms of pre-surgical and surgical steps. However, prior to membrane placement and closure, an open tray impression coping was fastened to the implant and several “temporary sutures” were placed to protect the open surgical site and approximate the anticipated soft-tissue contours (Figure 3). An open tray impression was then acquired (Position™ Penta™, 3M ESPE, www.3MESPE.com). The “temporary sutures” were then removed, and bone augmentation was performed as in the direct method, with the variation of adapting the membrane and soft tissue around a loosely fastened healing abutment. The poured model containing an implant replica from the surgical impression was then given to the patient to bring promptly to the restorative practice. This allowed the restorative dentist to fabricate the provisional restoration extraorally, using a prefabricated vacuum-formed template on the model (Figure 4). The authors found this technique beneficial to both the patient and dentist, eliminating the need for another prolonged procedure after surgery.
All temporary restorations were placed the same day of immediate implant surgery. No provisional crowns were removed for at least 8 weeks after the day of treatment. Final restorative treatment consisted of fabrication of custom zirconia or titanium abutments (ATLANTIS™, DENTSPLY Implants) and cement-retained restorations.
Case 1
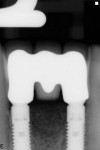
A 66-year-old female patient, who originally was treated with extraction and augmentation of the mandibular central incisors, presented for removal of the lateral incisors and immediate implant placement and fixed provisionalization. She had been wearing a removable appliance (Essix retainer) for the previous 4 months to esthetically replace the two central incisors (Figure 5). Following reflection of a full-thickness flap and careful removal of teeth Nos. 23 and 26, two 3.5-mm x 15-mm implants (OsseoSpeed) were placed into the extraction sockets of these teeth. Inserted with an insertion torque of 35 Ncm, both implants achieved primary stability (Figure 6). Bone allograft was adapted to augment the facial dehiscences of about 3 mm to 5 mm, and impression posts were secured. Several 5-0 sutures (VICRYL® ETHICON Sutures, Ethicon Products, www.ethiconproducts.co.uk) were placed to approximate the soft tissues around the impression posts (Figure 7). An open tray impression was taken using a polyvinyl material (Position Penta) and a modified stock impression tray. Implant replicas were affixed to the posts (Figure 8) and the impression was poured. Loosely tightened healing abutments were attached, and a resorbable collagen membrane (DynaMatrix) was adapted over the healing abutments via a tissue punch. The membrane overlapped the bone graft material and contacted the buccal and lingual cortices by about 3 mm. The flaps were then sutured with a monofilament, resorbable suture (MONOCRYL®, ETHICON Products) (Figure 9).
The patient was given the poured model to bring with her to the restorative dentist’s office following surgery. This model was used to fabricate a screw-retained provisional restoration (Figure 10). The restorative dentist incorporated two temporary abutments (TempDesign) into a one-piece restoration by adding a bis-acryl (LuxaTemp) and flowable composite resin extraorally. After polishing and contouring to assure proximal contacts were patent, hygiene was possible, and no occlusal contact with the maxillary anterior teeth was present, the provisional fixed partial denture (FPD) was hand-tightened to the two implants. The screw-access holes were obturated with cotton pellets and filled with flowable composite resin (Figure 11).
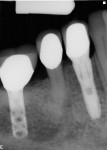
The temporary restoration remained in place for about 10 weeks prior to initiation of definitive restorative treatment. The final restoration was a cement-retained, three-unit FPD. The CAD/CAM abutments (ATLANTIS) were inserted and the abutment screws tightened to 20 Ncm. The ceramic restoration was cemented with an implant-specific cement (Premier® Implant Cement™, Premier Dental, www.premusa.com) (Figure 12). At the time of manuscript submission, this restoration had remained in situ for about 19 months without complications and proximal bone maintenance was noted (Figure 13). The patient continues to present for routine maintenance biannually at the restorative office and reports she is quite satisfied with the outcome of her implant therapy.
Case 2
A 63-year-old female patient presented with failing endodontic treatment on tooth No. 7 (Figure 14). After discussion with her restorative doctor regarding tooth replacement options, she elected to replace this tooth with a dental implant. Following surgical extraction and debridement of the extraction socket, a 3-mm x 13-mm implant was placed in a palatal position, achieving primary stability with an insertion torque of 35 Ncm (Figure 15). A transfer impression coping was placed and the soft tissue was re-approximated with two temporary sutures to facilitate impression taking (Figure 16).
Following impression taking, the sutures were removed and FDBA (LifeNet Health) was placed to obturate the space between the implant and the buccal bone wall. A resorbable collagen membrane (DynaMatrix) was adapted via a tissue punch over a loosely tightened healing abutment, and the site was closed with resorbable sutures (Figure 17). The provisional crown was fabricated extraorally on the model obtained from the surgical impression. Final contouring and occlusion were verified intraorally and the abutment screw was hand-tightened (Figure 18).
The provisional crown was removed for the first time approximately 10 weeks after surgery, demonstrating physiologic soft-tissue sculpting created by the contours of the temporary restoration (Figure 19). This enabled the restorative dentist to fabricate an all-ceramic restoration cemented onto a CAD/CAM-designed zirconia abutment (ATLANTIS), which has remained stable for 20 months, as of the time of manuscript submission (Figure 20 and Figure 21).
Results
All 29 immediately placed and temporized implants in this study achieved osseointegration and received definitive restorations, resulting in 100% survival. None displayed bone loss greater than 1 mm radiographically at a minimal loading time of 12 months. No continuous radiolucencies were noted, and none of the sites required surgical revision or loss of the restorations. All patients verbally expressed satisfaction with the esthetic outcome, and all cases were considered successful. Of the 29 fixtures, 25 showed proximal bone radiographically at or above the head of the implant, with a cumulative BM of 86%. Examples of BM are depicted in Figure 22 through Figure 26.
The data concerning implant site distribution, fixture dimensions, type of bone augmentation, and time loaded with the final restoration is found in Table 1.
Discussion
The high success of the cases presented in this study should not be surprising. Many investigators have reported excellent implant success rates in partially edentulous cases.11,12 Other parameters pertaining to esthetic success and bone maintenance prevail as long-term treatment goals for these patients receiving this type of therapy.
One attempt implant manufacturers have almost universally adopted to preserve crestal bone is the incorporation of a horizontal “off-set” of the fixture–abutment connection or “platform switch.” The theory behind this modality is that moving the “microgap,” which is known to be colonized by bacteria, and the ensuing zone of inflammation further from the bone crest may result in bone preservation. The other possibility supporting platform switching is that the normal dimension of the biologic width around an implant can be “relocated” away from the original crestal cortex. Vignoletti et al demonstrated similar dimensions of biologic width to that of a natural tooth around external hex implants in the canine model.13 This included crestal bone modeling to accommodate the vertical component of the biologic width. In a human study, Canullo et al demonstrated an inverse relationship between the amount of horizontal off-set and marginal bone loss when the patients were followed up to 21 months.14
The surface treatment and macrodesign may play a role in crestal bone maintenance. The roughened titanium surface of implants can be enhanced chemically. Investigators demonstrated accelerated bone healing with a fluoride-treated surface compared to identically roughened titanium without fluoride modification.15 In an in-vitro study, Guida et al demonstrated the fluoride-modified, titanium oxide grit-blasted surface stimulated extracellular matrix production and increased osteoprotegrin synthesis.16 Regarding macrotopography, it has been suggested that a coronal microthread can stimulate crestal bone physiologically, resulting in minimal bone loss under functional loading conditions. In a clinical study, Kim et al, showed minimal crestal bone loss radiographically with the same implant evaluated in the current study.17 Finite element analysis studies also suggest biomechanical advantages to a microthread favorably distributing occlusal forces within the crestal bone.18
The present study is very similar to a previous one by the same author (Dr. Levin).9 Implant locations are similar, the bone augmentation materials are virtually identical, and all clinical parameters regarding loading and method of screw retention are the same. The major variable is the implant itself, being of a different system. The BM obtained at an average of 9 months loading in the previous study was noted in 83% of the cases. The present study demonstrated 86% BM. The slight difference may not be significant, but certainly at almost three times longer loading time with definitive restorations, the current, microthreaded, fluoride-modified titanium implants perform at least as efficiently as the implants (SLActive) used in the earlier case series. This was not a comparative study between the two systems, but simply a second case series where clinical performance and radiographic bone levels could be seen as comparable between the two systems when used in similar practical situations.
Another reason that crestal bone may have been maintained in the present study is that all sites received bone grafts and barrier membranes simultaneously with immediate implant placement. In the dog model, Araújo et al showed that implant placement into a fresh extraction socket does not prevent significant facial bone loss.19 Botticelli et al demonstrated in a human study that slightly more than 50% of the facial bone dimensions at immediate implant placement was lost at 4-month re-entry.20 Sanz also showed significant facial and lingual bone loss at 4 months in humans.21 These immediate implants did not receive any bone augmentation at the time of placement. It is well accepted that a horizontal defect < 2 mm will spontaneously heal with osseointegration.22 If the goal is simply to achieve osseointegration for these implants in the esthetic zone, perhaps bone augmentation would not be necessary. Others have found that the thickness of the labial bone plate plays a critical role in the long-term maintenance of the soft tissues.23 With progressive bone resorption, soft-tissue recession is likely, compromising the esthetic result of these procedures. In the dog model, Barone et al found significantly less crestal bone loss for immediate implants when combining bone grafts with resorbable membranes compared to ungrafted controls.24
One technique strongly supported by some investigators is to perform immediate implant placement without the elevation of a soft-tissue flap (ie, flapless surgery). Maló et al25 found similar survival rates for implants placed with and without flaps in partially edentulous patients. He did note, however, that the percentage of crestal bone resorption for the flapless sites was slightly greater than for those implants inserted with a flap (2 mm versus 1.4 mm). The initial appeal of this procedure must be appreciated with caution. In an animal study, it was demonstrated that bone resorption, particularly on the buccal aspect, occurs to the same extent in extractions performed with or without flap reflection.26 Although flapless placement can be performed in specific situations, it can be technique-sensitive, and case selection is crucial for success. Chen et al noted that facial mucosal recession is “unpredictable” with flapless implant placement, and is more prevalent in patients with a “thin” periodontal biotype.27 These authors noted that flapless placement did not prevent marginal recession and caution surgeons that if a “good esthetic outcome is important,” this technique may be contraindicated. With respect to replacing teeth in the esthetic zone, where facial bone is often extremely “thin” or deficient,28 some investigators caution against flapless placement except in a minority of situations.29,30 A recent consensus found relatively good survival rates for flapless surgery, but did not recommend its routine use in daily practice due to the often more demanding skills it requires to produce favorable outcomes.31
Inasmuch as BM plays a crucial role in esthetic success, it is the peri-implant mucosa and how it “frames” the implant-retained restoration that provides the patient with the sense of success or failure. A scalloped, natural-appearing, soft-tissue contour is crucial for the outcome of therapy to result in an inconspicuous restoration. By delivering a provisional crown(s) at the time of extraction and implant placement rather than a round healing abutment, the healing process is initiated with the contours of the expected anatomic situation. Standard healing abutments do not provide support for proximal soft tissue or papilla and cannot be easily “under-contoured” facially, minimizing recession. A properly fabricated temporary restoration addresses these shortcomings. When two-stage implant protocols are implemented, soft-tissue conditioning begins at the time of surgical uncovery. Glauser et al demonstrated that provisionalization at this time is advantageous for achieving esthetically pleasing outcomes.32 Stein and Nevins described how the implant’s vertical depth can play a significant role in helping the provisional crown develop a pleasing soft-tissue “frame” prior to the initiation of definitive restorative treatment.33 Protocols for a two-piece implant abutment system typically recommend a vertical positioning of the fixture head approximately 3-mm apical to the planned mucosal zenith of facial restorative margins.34
Conclusions
The planning of all cases is critical to achieving success. When immediate implant placement is selected as the mode of anterior tooth (teeth) replacement, and immediate temporization is performed, several steps may aid the implant team in achieving optimal outcomes. First, the ability to place the implant in the prosthetically driven position, thus achieving primary stabilization, must be expected. Second, measures to compensate for physiologic bone modeling after extractions should be considered. These normally include bone grafting, guided bone regeneration, and even soft-tissue grafting in certain situations. Third, an anatomically contoured, highly polished provisional restoration that is out of occlusal function should be delivered and retained with an abutment screw versus temporary cement. The temporary restoration should not be removed for a minimum time period of 8 weeks to protect early hard- and soft-tissue healing dynamics and to avoid jeopardizing osseointegration.
A fluoride-modified, roughened-surface implant with a coronal microthread macrodesign can be immediately placed and immediately temporized with the expectations of implant success, survival, and bone maintenance in a predictable manner.
DISCLOSURE
The authors acknowledge no financial or material support while conducting this study.
ABOUT THE AUTHORS
Barry P. Levin, DMD
Clinical Associate Professor, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania; Private Practice limited to Periodontics and Dental Implant Surgery, Elkins Park, Pennsylvania
Brian L. Wilk, DMD
Private Practice, Restorative, Esthetic and Implant Dentistry, Chalfont, Pennsylvania
REFERENCES
1. Buser D, Halbirtter S, Hart C, et al. Early implant placement with simultaneous guided bone regeneration following single-tooth extraction in the esthetic zone: 12-month results of a prospective study with 20 consecutive patients . J Periodontol. 2009;80(1):152-162.
2. Schwarz F, Herten M, Sager M, et al. Bone regeneration in dehiscence-type defects at chemically modified (SLActive) and conventional SLA titanium implants: a pilot study in dogs . J Clin Periodontol. 2007;34(1):78-86.
3. Magne P, Paranhos MP, Burnett LH Jr, et al. Fatigue resistance and failure mode of novel-design anterior single-tooth implant restorations: influence of material selection for type III veneers bonded to zirconia abutments . Clin Oral Implants Res. 2001;22(2):195-200.
4. De Rouck T, Collys K, Cosyn J. Single-tooth replacement in the anterior maxilla by means of immediate implantation and provisionalization: a review . Int J Oral Maxillofac Implants. 2008;23(5);897-904.
5. Shapoff CA, Lahey BJ. Crestal bone loss and the consequences of retained excess cement around dental implants . Compend Contin Educ Dent. 2012;33(2):94-102.
6. Patras M, Naka O, Doukoudakis S, Pissiotis A. Management of provisional restorations’ deficiencies: a literature review . J Esthet Restor Dent. 2012;24(1):26-38.
7. Tarnow DP, Emtiaz S, Classi A. Immediate loading of threaded implants at stage 1 surgery in edentulous arches: ten consecutive case reports with 1- to 5-year data . Int J Oral Maxillofac Implants. 1997;12(3):319-324.
8. Degidi M, Nardi D, Piattelli A. A comparison between immediate loading and immediate restoration in cases of partial posterior mandibular edentulism: a 3-year randomized clinical trial. Clin Oral Implants Res.2010;21(7):682-687.
9. Levin B. Immediate temporization of immediate implants in the esthetic zone: evaluating survival and bone maintenance . Compend Contin Educ Dent. 2011;32(4):52-62.
10. Norton MR. Biologic and mechanical stability of single-tooth implants: 4- to 7-year follow-up . Clin Implant Dent Relat Res. 2001;3(4):214-220.
11. De Rouck T, Collys K, Wyn I, Cosyn J. Instant provisionalization of immediate single-tooth implants is essential to optimize esthetic treatment outcome . Clin Oral Implant Res. 2009;20(6):566-570.
12. Valentini P, Abensur D, Albertini JF, Rocchesani M. Immediate provisionalization of single extraction-site implants in the esthetic zone: a clinical evaluation . Int J Periodontics Restorative Dent. 2010;30(1):41-51.
13. Vignoletti F, de Santis M, Berglundh T, et al. Early healing of implants placed into fresh extraction sockets: an experimental study in the beagle dog. III: soft tissue findings . J Clin Periodontol. 2009;36(12):1059-1066.
14. Canullo L, Fedele GR, Iannello G, Jepsen S. Platform switching and marginal bone-level alterations: the results of a randomized-controlled trial . Clin Oral Implants Res. 2010;21(1):115-121.
15. Berglundh T, Abrahamsson I, Albouy JP, Lindhe J. Bone healing at implants with a fluoride-modified surface: an experimental study in dogs . Clin Oral Implants Res. 2007;18(2):147-152.
16. Guida L, Annunziata M, Rocci A, et al. Biological response of human bone marrow mesenchymal stem cells to fluoride-modified titanium surfaces . Clin Oral Implants Res. 2010;21(11):1234-1241.
17. Kim JJ, Lee DW, Kim CK, et al. Effect of conical configuration of fixture on the maintenance of marginal bone level: preliminary results at 1 year of function . Clin Oral Implants Res. 2010;21(4):439-444.
18. Hudieb MI, Wakabayashi N, Kasugai S. Magnitude and direction of mechanical stress at the osseointegrated interface of the microthread implant . J Periodontol. 2011;82(7):1061-1070.
19. Araújo MG, Wennström JL, Lindhe J. Modeling of the buccal and lingual bone walls of fresh extraction sites following implant installation . Clin Oral Implants Res. 2006;17(6):606-614.
20. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites . J Clin Periodontol. 2004;31(10):820-828.
21. Sanz M, Cecchinato D, Ferrus J, et al. A prospective, randomized-controlled clinical trial to evaluate bone preservation using implants with different geometry placed into extraction sockets in the maxilla . Clin Oral Implants Res. 2010;21(1):13-21.
22. Wilson TG Jr, Schenk R, Buser D, Cochran D. Implants placed in immediate extraction sites: a report of histologic and histometric
analyses of human biopsies . Int J Oral Maxillofac Implants. 1998;13(3):333-341.
23. Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering . Ann Periodontol. 2000;5(1):119-128.
24. Barone A, Ricci M, Calvo-Guirado JL, Covani U. Bone remodeling after regenerative procedures around implants placed in fresh extraction sockets: an experimental study in Beagle dogs . Clin Oral Implants Res. 2011;22(10):1131-1137.
25. Maló P, Nobre Md. Flap vs. flapless surgical techniques at immediate implant function in predominantly soft bone for rehabilitation of partial edentulism: a prospective cohort study with follow-up of 1 year . Eur J Oral Implantol. 2008;1(4):293-304.
26. Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog . Clin Oral Implants Res. 2009;20(6):545-549.
27. Chen ST, Darby IB, Reynolds EC, Clement JG. Immediate implant placement postextraction without flap elevation . J Periodontol. 2009;80(1):163-172.
28. Huynh-Ba G, Pjetursson BE, Sanz M, et al. Analysis of the socket bone wall dimensions in the upper maxilla in relation to immediate implant placement . Clin Oral Implants Res. 2010;21(1):37-42.
29. Braut V, Bornstein MM, Belser U, Buser D. Thickness of the anterior maxillary facial bone wall—a retrospective radiographic study using cone beam computed tomography . Int J Periodontics Restorative Dent. 2011;31(2):125-131.
30. Januário AL, Duarte WR, Barriviera M, et al. Dimension of the facial bone wall in the anterior maxilla: a cone-beam computed tomography study . Clin Oral Implants Res. 2011;22(10):1168-1171.
31. Brodala N. Flapless surgery and its effect on dental implant outcomes . Int J Oral Maxillofac Implants. 2009;24 suppl:118-125.
32. Glauser R, Sailer I, Wohlwend A, et al. Experimental zirconia abutments for implant-supported single-tooth restorations in esthetically demanding regions: 4-year results of a prospective clinical study . Int J Prosthodont. 2004;17(3):285-290.
33. Stein JM, Nevins M. The relationship of the guided gingival frame to the provisional crown for a single-implant restoration . Compend Contin Educ Dent. 1996;17(12):1175-1182.
34. Martin W, Morton D, Ruskin J. Planning for esthetics—part 1: single tooth bone level implant restorations . Tex Dent J. 2011;128(12):1298-1299.