The Impact of Early-in-Life Periodontal Infection on the Smiles of Children: A Worldwide View
Hessam Nowzari DDS, PhD; Javier Enrique Botero, DDS, PhD; and Sandra K. Rich, PhD
Abstract
Little attention has been directed toward evidence that an early-in-life oral infection with the potential to reach epidemic proportions is threatening the health of youths throughout world. Health professionals and the public seem unaware that the silent disease process of early-in-life periodontal infection is targeting thousands of children and young adults, their smiles, and, consequently, their emotional and psychologic lives. Yet, the literature is replete with reports that many periodontopathic microorganisms are multiplying at an alarming rate with a serious impact on youths in many cities, towns, and villages throughout the globe. However, clinical measurement of reported periodontal disease has been fraught with problems that have confused and clouded messages to policymakers in government and health professionals in treatment settings. The aim of this article is to help raise the level of awareness so that those who have the power and knowledge can appropriately address the suffering of the youngest members of societies.
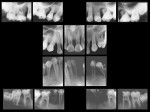
Periodontal disease is one of the most common forms of oral disease and can manifest early in life. This silent disease targets children and young adults with the consequent affection of the supporting periodontal tissues. Teeth start to shift position and, in severe cases, are lost, resulting in an impairment of the smile. The loss of an attractive smile is emotionally and socially relevant for a child’s interaction with the society.1 Several microorganisms, such as Aggregatibacter actinomycetemcomitans, Porphyromonasgingivalis, Tannerella forsythia, Campylobacter rectus, Eikenella corrodens, Prevotella intermedia, Prevotella nigrescens, and Treponema denticola, have been implicated as important initiators of periodontal disease throughout the world.2-4 The early-in-life periodontal infection is distinguished from the chronic form of periodontal disease affecting adults in that it is established in children and adolescents and has a rapid rate of tissue destruction. The extrusion or protrusion of maxillary incisors following periodontal attachment loss, extensive destruction of anterior papilla, or loss of maxillary central incisors seriously damages facial expression (Figure 1, Figure 2 and Figure 3).
While studies addressing the prevalence of chronic periodontitis are abundant, reports of periodontal disease among children and adolescents are scarce. A position paper by the American Academy of Periodontology in 2003 states that the most prevalent form of periodontal disease in young individuals is gingivitis and attachment loss (≥ 5 mm) can occur in approximately 0.2% to 0.5% of this population. Although this number seems low, the young population has an increased risk of developing periodontitis, and routine dental examinations should be performed annually.5
There is a need to examine the evidence critically and to raise the international level of awareness of the importance of maintaining good oral health from birth to adulthood.
Evidence of a Global Crisis
The focus on dental caries in the 20th century overshadowed important information regarding the impact of periodontal disease on the global population. In the US,6 the pre-valence of early-onset periodontitis has been reported to be as low as < 1% in 14 to 17 year olds, but other indications are that it may be as high as 3.6% in adults 18 to 34 years old. In Nigeria, the most frequently lost teeth are incisors, a finding which is indicative of aggressive periodontitis.7 Nonetheless, extensive and severe periodontitis in Nigeria is much more prevalent in minorities and certain regions of the country. Epidemiological findings indicate that profound periodontal health disparities exist within the US as well as in other populations around the world. In Israel, Stabholz et al8 noted that 33 (38.4%) of 86 individuals from 15 families living in close proximity were diagnosed with localized juvenile periodontitis. Also in Israel, Levin et al9 found aggressive periodontitis in 4.3% (localized) and 1.6% (generalized) of 642 army recruits aged 18 to 30 years. Studies from Brazil, Argentina, Chile, Mexico, and Colombia10-17 (Table 1) revealed that signs of gingival inflammation in individuals younger than 19 years are common and the frequency of gingivitis can reach 100%. Conversely, signs of periodontitis, such as clinical attachment loss (> 5 mm) and pocketing (> 5 mm), were 0.1% to 0.32%. One Brazilian study by Gjermo et al10 found a prevalence of 28% of periodontitis, indicated by the presence of one or more sites with radiographic bone loss. Results from studies conducted in Asia are similar (Table 2).18-30 Gingivitis once again was the most prevalent form of periodontal disease, ranging from 15% to 99%. In addition, the frequency of pockets 4 mm to 5 mm was as high as 44% while probing depths ≥ 6 mm were not as frequent (2%). The highest prevalence of periodontal disease has been reported in African countries (Table 3).31-37 The detection of pockets measuring ≥ 6 mm was in the order of 7%, and a study reported a frequency of localized juvenile periodontitis of 41.5% in Senegal.35 In addition, the prevalence of generalized juvenile periodontitis was 4% in Morocco37 and 28.8% in Senegal.35 While few studies provide information on the prevalence of periodontal disease in young individuals in Latin American, Asian, and African countries, these data should be considered carefully. In a review of juvenile periodontitis, Saxén38 noted prevalence rates varied widely from 0.1% to 17.6%. The author stated that although there could be racial variations, estimations of the prevalence varied within racial groups, as well. Saxén suggested this inconsistency indicated there “must be great variations” in the methods of evaluation used. Likewise, studies mentioned in Table 1, Table 2, and Table 3 also reflect disparities in diagnostic methods, thresholds for clinical measures, different clinical indexes, and social and economic variations. For this matter, the lowest socioeconomic level was found in Africa, where the prevalence of periodontitis was higher. Other individual variants such as ethnicity and genetic predisposition also should be considered.
Epidemiologic studies (Table 1, Table 2 and Table 3) found gingivitis and pockets 4 mm to 5 mm were the most frequent periodontal findings. However, these findings should be analyzed carefully because there are significant differences between studies, such as recording of clinical parameters and the use of periodontal indexes. Furthermore, gingival inflammation and increased probing depths (in the absence of clinical attachment loss, a pseudo-pocket) create a subgingival environment for the overgrowth of P gingivalis, A actinomycetemcomitans, T forsythia, superinfecting bacteria such as enteric rods, and viruses, thus creating a niche for periodontal and systemic infection. In addition, untreated gingivitis still represents a long-term immune process that can progress to periodontitis.
Pathogenesis of Early Microbial Infection
The specific mechanism that explains the degree of periodontal destruction in children as compared to adults requires further evaluations. Is severe periodontal destruction in children related to a highly pathogenic microorganism? Is destruction because of an overexpression of cytokines and an elevated immune system? Or is it a combination of all?
Periodontopathic bacteria, such as P gingivalis, T forsythia, and A actinomycetemcomitans, produce potent virulence factors.39-41 Based on overwhelming microbiologic and immunologic data, A actinomycetemcomitans is the consistent and prominent microorganism in most countries where early-onset periodontitis has been evaluated. In these countries, eradication and reassessment of recolonization of A actinomycetemcomitans seems to be an efficacious preventive approach.42 However, the microbial profile of the early-onset aggressive-periodontitis population can be more complex. Ethnic origin and geographic factors appear to influence the distribution of pathogenic species. P gingivalis may be more prevalent in Chile.43 On the other hand, T forsythia, C rectus, P gingivalis, and T denticola seem to be the predominant periodontopathic bacteria in Japan.44 In Korea, the major periodontal pathogens strongly associated with aggressive periodontitis are Fusobacterium species, P gingivalis, Treponema species, T forsythia, Micromonas micros, P intermedia, and, less frequently, A actinomycetemcomitans.45 In Turkey, serotypes not-yet-identified of A actinomycetemcomitans suggest that local conditions may influence the colonization of the species.46 In Morocco, JP2 clone of A actinomycetemcomitans is associated significantly with an increased risk of periodontal attachment loss.47
When the microbial biofilm has established in subgingival environment, inflammation occurs and the sulcular and junctional epithelial cells initiate an inflammatory response48 by production of defensins and cytokines, including interleukin (IL)-8 and IL-1b.49-51 From 1 week to 2 weeks after the bacterial challenge, CD4 T cells infiltrate the connective tissue, resulting in a combination of Th1 and Th2 T cell response.52 In most cases, the response is capable of controlling the infection. However, when the bacterial invasion is not controlled and an early oral microbial infection is established, connective-tissue degradation and bone destruction advance rapidly.53 In advanced states, B cells and plasmocytes dominate the inflammatory infiltrate.54 Although an adaptative immune response is established, macrophages continue producing IL-1b and tumor necrosis factor (TNF)-a, resulting in more inflammation and osteoclast differentiation.55,56 In addition, activated CD4 T cells express receptor activator of nuclear factor k-b ligand (RANKL) and more osteoclast activation.56 The concomitant recruitment of Th1 T cells establishes the production of IL-2 and INF-g, which are important factors for the production of matrix metalloproteinases (MMPs) and collagenases from monocytes and fibroblasts.57 In answer to the question of a specific mechanism to explain severe periodontal destruction in children, all the aforementioned events work in combination to eventually lead to the degradation of collagen connective tissues, bone loss, and pocket formation.
The Emotional Impact
Patel et al58 found that periodontal health/disease in adults affected psychosocial outcomes in smiling patterns for what they termed “smile-related quality of life.” Most likely, their findings would apply with stronger significance in child and adolescent populations. Specifically, they determined the more teeth with probing depths between 4 mm and 6 mm the subjects had, the less widely they opened their mouths when they smiled (P = .03); the more hypermobile teeth the subjects had, the less open their smiles were (P = .04), and the more likely they were to cover their mouths when they smiled (P = .01); and the more sites of gingival recession in the esthetic zone the subjects had, the fewer teeth they showed when they smiled (P = .02). They concluded that self-concept and social interactions may be affected by smiling patterns.
Periodontal disease in children, as well as in adults, can be responsible for an unattractive smile and abnormal smile behavior along with causing the discomfort, pain, and necessity of extensive dental treatment. Further, the condition can lead to emotional pain from social rejection and alienation.59 To date, little attention has been given to the psychologic and emotional impact of early-in-life periodontal infection. Yet, increasing numbers of children are being affected (Figure 2 and Figure 3). How are these children giving a meaning to what is happening to them? How do affected adolescents face personal challenges and social difficulties associated with their facial appearance? How do young adults relate to each other? How are relationships influenced by the facial appearance of the smile or speech problems that can result from loss of teeth?
Modern society places significant emphasis on facial expression, and, consequently, facial expression plays an important role in human interactions. The smile has significant effect on first impressions that can dictate the way others respond to children or adolescents.60 Unfortunately, reactions eagerly anticipated by the smiling child with missing teeth and inflamed gingiva may not be forthcoming from others. Expectations and opportunities can be limited because of miscommunication and misinterpretation due to facial differences.
The permanent loss of maxillary incisors can result in learning problems at school and social inhibition caused by self-consciousness about appearance.61 Children may show dependent behavior or regress to behaviors appropriate to a much younger child. Therefore, school-age children affected by destructive early-in-life periodontal diseases may be at risk for delayed educational development because of poor social interactions and responses from the public, peers, parents, and teachers.
In addition, the familial tendency of many forms of early-onset periodontal diseases may result in significantly more complicated psychologic issues by having an impact on the well being of the entire family.
Conclusion
Resources are limited with regard to trained public health practitioners and facilities available to support periodontal health programs. However, evidence reviewed in this article strongly suggests that the well-being of children worldwide is challenged by early-in-life oral infections. The au-thors believe these findings clearly and firmly indicate a need for the dental community’s best efforts to reduce the incidence of infections and improve periodontal health through prevention, early diagnosis, and treatment. Protecting and restoring the smiles of affected children and adolescents can enhance health and confidence, diminish anxiety and negative feelings, and, thus, encourage them to explore new ways of moving forward.
References
1. Strauss RP, Fenson C. Experiencing the “Good Life”: literary views of craniofacial conditions and quality of life. Cleft Palate-Craniofac J. 2003;42(1):14-18.
2. Herrera D, Contreras A, Gamonal J, et al. Subgingival microbial profiles in chronic periodontitis patients from Chile, Colombia and Spain. J Clin Periodontol. 2008;35(2):106-113.
3. Tanner AC, Kent R Jr, Kanasi E, et al. Clinical characteristics and microbiota of progressing slight chronic periodontitis in adults. J Clin Periodontol. 2007;34(11):917-930.
4. Ximénez-Fyvie LA, Haffajee AD, Socransky SS. Comparison of the microbiota of supra- and subgingival plaque in health and periodontitis. J Clin Periodontol. 2000;27(9):648-657.
5. Califano JV; Research, Science and Therapy Committee of the American Academy of Periodontology. Position paper: periodontal disease in children and adolescents. J Periodontol. 2003;74:1696-1704.
6. Oliver RC, Brown LJ, Löe H. Periodontal diseases in the United States population. J Periodontol. 1998;69(2):269-278.
7. Dosumu OO, Dosumu EB, Arowojolu MO. Pattern of tooth loss in Nigerian juvenile and plaque-induced chronic periodontitis patients. Afr J Med Med Sci. 2003;32(4): 361-365.
8. Stabholz A, Mann J, Agmon S, et al. The description of a unique population with a very high prevalence of localized juvenile periodontitis. J Clin Periodontol. 1998;25(11):872-878.
9. Levin L, Baev V, Lev R, et al. Aggressive periodontitis among young Israeli army personnel. J Periodontol. 2006;77(8):1392-1396.
10. Gjermo P, Bellini HT, Pereira Santos V, et al. Prevalence of bone loss in a group of Brazilian teenagers assessed on bite-wing radiographs. J Clin Periodontol. 1984;11(2): 104-113.
11. de Muñiz BR. Epidemiologic oral health survey of Argentine children. Community Dent Oral Epidemiol. 1985;13(6):328-333.
12. López NJ, Rios V, Pareja MA, et al. Prevalence of juvenile periodontitis in Chile. J Clin Periodontol. 1991;18: 529-533.
13. González M, Cabrera R, Grossi SG, et al. Prevalence of dental caries and gingivitis in a population of Mexican schoolchildren. Community Dent Oral Epidemiol. 1993:21(1):11-14.
14. Tinoco EM, Beldi MI, Loureiro CA, et al. Localized juvenile periodontitis and Actinobacillus actinomycetemcomitans in a Brazilian population. Eur J Oral Sci. 1997;105(1):9-14.
15. Cunha ACP, Chambrone LA. Prevalencia de gengivite em criancas. Revista Periodontia 1998;7:1-5.
16. Cunha ACP, Chambrone LA. Prevalencia de gengivite em criancas de um nivel social baixo. Revista Periodontia. 1998;7: 6-10.
17. Ministerio de Salud. III Estudio nacional de salud bucal—ENSAB III, II estudio nacional de factores de riesgo de enfermedades cronicas—ENFREC II. Lito Servicios Aler. 1999: 105-110.
18. Wei SH, Shi Y, Barmes DE. Needs and implementation of preventive dentistry in China. Community Dent Oral Epidemiol. 1986;14(1):19-23.
19. Nordblad A, Kallio P, Ainamo J, et al. Periodontal treatment needs in populations under 20 years of age in Espoo, Finland and Chiangmai, Thailand. Community Dent Oral Epidemiol. 1986;14(3):129-131.
20. Lind OP, Holmgren CJ, Evans RW, et al. Hong Kong survey of adult oral health. Part 1: clinical findings. Community Dent Health. 1987;4(4): 351-366.
21. Songpaisan Y, Davies GN. Periodontal status and treatment needs in the Chiangmai/Lamphun provinces of Thailand. Community Dent Oral Epidemiol. 1989;17(4):196-199.
22. Abdul-Kadir R, Yassin AT. Periodontal status (CPITN) of six- to fifteen-year-old West Malaysian Aborigines (Proto-Malays). J Nihon Univ Sch Dent. 1989;31(4):612-618.
23. Miyazaki H, Hanada N, Andoh MI, et al. Periodontal disease prevalence in different age groups in Japan as assessed according to the CPITN. Community Dent Oral Epidemiol. 1989;17(2): 71-74.
24. Arvidson-Bufano UB, Holm AK. Dental health in urban and rural areas of central and western Bangladesh. Odontostomatol Trop. 1990;13(3): 81-86.
25. Anil S, Hari S, Vijayakumar T. Periodontal conditions of a selected population in Trivandrum District, Kerala, India. Community Dent Oral Epidemiol. 1990;18(6): 325.
26. Abdul-Kadir R. Periodontal status of 16-year-old west Malaysian urban students. Community Dent Oral Epidemiol. 1990;18(6):324.
27. Peng TK, Yao JH, Shih KS, et al. Assessment of periodontal disease in an adult population survey in Taipei city using CPITN and GPM/T indices. Zhongha Ya Yi Zue Hui Za Zhi. 1990;9(2):67-74.
28. Peng B, Petersen PE, Fan MW, et al. Oral health status and oral health behaviour of 12-year-old urban schoolchildren in the People’s Republic of China. Community Dent Health. 1997;14(4):238-244.
29. Pilot T. The periodontal disease problem. A comparison between industrialized and developing countries. Int Dent J. 1998;48:221-232.
30. Lo EC, Jin LJ, Zee KY, et al. Oral health status and treatment need of 11-13-year-old urban children in Tibet, China. Community Dent Health. 2000;17(3): 161-164.
31. Harley AF, Floyd PD. Prevalence of juvenile periodontitis in schoolchildren in Lagos, Nigeria. Community Dent Oral Epidemiol. 1988;16: 299-301.
32. Haikel Y, Turlot JC, Cahen PM, et al. Periodontal treatment needs in populations of high- and low-fluoride areas of Morocco. J Clin Periodontol. 1989;16(9): 596-600.
33. Baelum V, Fejerskov O, Manji F, et al. Influence of CPITN partial recordings on estimates of prevalence and severity of various periodontal conditions in adults. Community Dent Oral Epidemiol. 1993;21(6):354-359.
34. Clerehugh V, Laryea U, Worthington HV. Periodontal condition and comparison of toothcleaning using chewing sponge, chewing sticks and toothbrushes in 14-year-old schoolchildren in Ghana. Community Dent Oral Epidemiol. 1995;23(5):319-320.
35. Ndoye-Ngom M, Sembene M, Diallo PD, et al. Les parodontites juveniles a l’institut d’odonto-stomatologie de dakar. A propos de 118 cas. Odonto Stomatologie Tropicale. 1995: 15-20.
36. Tapsoba H, Bakayoki-Ly R. Oral health status of 12-year-old schoolchildren in the province of Kadiogo, Burkina Faso. Community Dent Health. 2000;17(1): 38-40.
37. Belhaissi FE, Cherkaoui A, Laporte C, et al. The localized aggressive periodontitis prevalence in Morocco. Odonto Stomatologie Tropicale. 2004;105:27-28.
38. Saxén L. Juvenile periodontitis. J Clin Periodontol. 1980;7(1): 1-19.
39. Kadowaki T, Takii R, Yamatake K, et al. A role for gingipains in cellular responses and bacterial survival in Porphyromonas gingivalis-infected cells. Front Biosci. 2007;12:4800-4809.
40. Inagaki S, Kuramitsu HK, Sharma A. Contact-dependent regulation of a Tannerella forsythia virulence factor, BspA, in biofilms. FEMS Microbiol Lett. 2005;249(2): 291-296.
41. Ebersole JL, Kraig E, Bauman G, et al. Molecular approaches to leucotoxin as a virulence component in Actinobacillus actinomycetemcomitans. Arch Oral Biol. 1990;35(suppl): 69S-78S.
42. Kamma JJ, Nakou M, Gmür R, et al. Microbiological profile of early onset/aggressive periodontitis patients. Oral Microbiol Immunol. 2004;19(5): 314-321.
43. López NJ, Mellado JC, Leighton GX. Occurrence of Actinobacillus actinomycetemcomitans, Porphyromonas gingivalis and Prevotella intermedia in juvenile periodontitis. J Clin Periodontol. 1996;23(2):101-105.
44. Takeuchi Y, Umeda M, Ishizuka M, et al. Prevalence of periodontopathic bacteria in aggressive periodontitis patients in a Japanese population. J Periodontol. 2003;74(10):1460-1469.
45. Lee JW, Choi BK, Yoo YJ, et al. Distribution of periodontal pathogens in Korean aggressive periodontitis. J Periodontol. 2003;74(9): 1329-1335.
46. Do×gan B, Antinheimo J, Cetiner D, et al. Subgingival microflora in Turkish patients with periodontitis. J Periodontol. 2003;74(6): 803-814.
47. Haubek D, Ennibi OK, Poulsen K, et al. Risk of aggressive periodontitis in adolescent carriers of the JP2 clone of Aggregatibacter (Actinobacillus) actinomycetemcomitans in Morocco: a prospective longitudinal cohort study. Lancet. 2008;371(9608): 237-242.
48. Kinane D, Lappin DF. Immune processes in periodontal disease: a review. Ann Periodontol. 2002;7(1):62-71.
49. Delima AJ, van Dyke TE. Origin and function of the cellular components in gingival crevice fluid. Peridontol 2000. 2003;31:55-76.
50. Ebersole JL. Humoral immune responses in gingival crevice fluid: local and systemic implications. Peridontol 2000. 2003;31:135-166.
51. Van Dyke TE, Kornman KS. Inflammation and factors that may regulate inflammatory response. J Periodontol. 2008;79(8 suppl):1503-1507.
52. Yamazaki K, Nakajima T, Gemmel E, et al. IL-4- and IL-6-producing cells in human periodontal disease tissue. J Oral Pathol Med. 1994;23(8): 347-353.
53. Van Dyke T, Serhan CN. Resolution of inflammation: a new paradigm for the pathogenesis of periodontal diseases. J Dent Res. 2003;82(2): 82-90.
54. Page RC, Offenbacher S, Schroeder HE, et al. Advances in the pathogenesis of periodontitis: summary of developments, clinical implications and future directions. Peridontol 2000. 1997;14:216-248.
55. Fujihashi K, Beagley KW, Kono Y, et al. Gingival mononuclear cells from chronic inflammatory periodontal tissues produce interleukin (IL) 5 and IL-6 but not IL4 and IL-2. Am J Pathol. 1993;142(4): 1239-1250.
56. Cochran DL. Inflammation and bone loss in periodontal disease. J Periodontol. 2008;79(8 suppl):1569-1576.
57. Seymour GJ, Gemmell E, Reinhardt RA, et al. Immunopathogenesis of chronic inflammatory periodontal disease: cellular and molecular mechanisms. J Periodontal Res. 1993;28(6 Pt 2):478-486.
58. Patel RR, Richard PS, Inglehart MR. Periodontal health, quality of life, and smiling patterns—an exploration. J Periodontal. 2008;7(2): 224-231.
59. Lovegrove E, Rumsey N. Ignoring it doesn’t make it stop: adolescents, appearance, and bullying. Cleft Palate Craniofac J. 2005;42(1): 33-44.
60. Bull R, Rumsey N. The Social Psychology of Facial Appearance. 1st ed. New York, NY: Springer-Verlag; 1988.
61. Broder H, Strauss RP. Self-concept of early primary school age children with visible and invisible defects. Cleft Palate J. 1989;26(2): 114-117.
About the Authors
Hessam Nowzari DDS, PhD
Professor and Director
Advanced Periodontics
University of Southern California School of Dentistry
Los Angeles, California
Javier Enrique Botero, DDS, PhD
School of Dentistry
Universidad de Antioquia
Medellin, Colombia
Sandra K. Rich, PhD
Associate Professor
Advanced Periodontics
University of Southern California School of Dentistry
Los Angeles, California