You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Posture, temporomandibular disorders (TMD), muscles in the neck, back, pelvis, legs, and the whole craniomandibular complex are all intimately related to the bite or how teeth interdigitate. An improper bite can predispose and/or directly cause malfunction of the temporomandibular joint (TMJ) (internal derangement), which can result in one or more of the following symptoms: headaches, pain behind the eyes, facial or throat pain, dizziness, earaches, clenching or grinding of the teeth, neck pain, clicking, popping or grating sounds in the jaw joints, and tired jaws. These problems can be caused by the joints, the muscles of the face and jaw, or a combination thereof. Structures that make it possible to open and close the mouth include bones, joints, and muscles. The teeth are inserted into the jaw bone. The TMJs connect the jaw to the skull. Muscles attach to the bones and joints of the stomatognathic system. Improper muscle function creates muscle spasm, which has a direct correlation with displaced discs within the jaw joints. The muscles that manipulate the jaw with respect to the skull facilitate talking, chewing, breathing, and swallowing. A bite where the teeth do not come together properly directly impacts all of these physiologic functions negatively. If a nonphysiologic bite continues on a chronic basis and is further disrupted by trauma, clenching and grinding, a poor airway, and/or numerous dental restorations, an adverse effect on the overall physiology of the patient is likely. Treatment of a patient to optimal dental physiology takes into consideration these situations and diagnoses the major contributions of the problem, ultimately correcting the improper bite, which facilitates healing and relief of the patient’s adverse symptoms. Optimal dental physiology is a treatment philosophy that diagnoses existing teeth, periodontal, maxillary/mandibular orthopedic, airway, and overall stomatognathic functioning conditions realizing that they are related intimately. The treatment philosophy recognizes that pathology in any or a combination of the above mentioned areas contributes to a negative impact on several physiologic considerations of the patient’s well-being and health.
A THREE-STAGE COMBINATION CASE STUDY
A 57-year-old woman presented with the chief complaints of jaw joint clicking and popping, jaw joint pain, and headaches. She felt that she had a bad bite and that her mouth did not close properly. Further, she disliked the appearance of her teeth. An initial screening examination revealed that she had been involved in an accident and suffered a traumatic blow to the mandible. She had a hard time closing her mouth together for several weeks following the accident. The patient stated that her jaw joints were sore on awakening. She was aware of daytime and nighttime clenching, and her jaw popped on opening and closing. She had several old fillings and crowns, and her teeth were becoming sensitive. She did not like the way her teeth looked and wanted to be happy with her smile (Figure 1 and Figure 2). The patient was given a consult to take diagnostic records.
Record Gathering and Examination
Upper and lower models were made and mounted on an articulator at her existing habitual bite. A series of full-mouth bitewing, periapical, and panoramic radiographs were made. In addition, right and left corrected-angle tomograms were taken at her maximum intercuspation, rest, and full-opening posture. Also, a cephalogram, right/left anterior/posterior coronal tomograms, frontal skull, Towne’s view, and lateral skull radiographs were taken. The biometric records taken included joint vibration analysis (JVA), resting and functional electromyograms (EMGs), range of motion jaw tracking, and opening and closing mandibular velocity trace. Intraoral, extraoral, and postural photographs were taken. The patient was given a comprehensive questionnaire to complete. The mounted models revealed an uneven occlusal pattern with a high uphill roll pattern to the left. The bitewing and periapical radiographs showed extensively failing restorations with recurrent decay and various isolated periapical lesions. There was generalized stage III bone loss as a result of chronic occlusal trauma, determined because the patient’s home care was excellent and there was no bleeding or evidence of periodontal disease.
The panoramic radiograph revealed teeth Nos. 1, 13, 16, 17, and 32 were missing. There was bilateral antegonial notching, resulting from chronic excessive masseter muscle hyperfunction. The nasal septum was relatively straight with no turbinate obstruction noted. The right and left tomograms revealed excessive posterior and superior displacement. Excessive orthopedic bending was noted bilaterally and the right tomogram showed osseous degeneration. Both joints exhibited hypertranslation,1 which represents excessive stretching in the bilaminar zone of the posterior ligament. The cephalogram showed lack of normal lordotic curvature, with inadequate spacing between the C1 and C2 vertebrae. The antigonial notching was again noted, and the double border of the mandible was consistent with the previously noted uphill cant to the left of the occlusal table. This cervical orthopedic relationship was also consistent with the forward head posture observed on the postural photographs. The anterior and posterior coronal tomograms showed normal osseous contour on the left, and osseous degeneration of the right lateral pole. The frontal skull radiograph was traced for a triplanar analysis. The three planes traced ran through the frontosphenoid sutures of the orbits, the mastoid processes, and the gonial angles of the mandibles. By tracing these three planes, cranial orthopedic problems can be diagnosed.2 The frontosphenoid plane and the mastoid process plane were parallel. The gonial angle plane converged to the left side. Gonial angle plane discrepancies can be corrected with a mandibular orthopedic repositioning appliance (MORA), which will make the gonial angle level with the other planes. Cases with orthopedic and TMJ issues, as presented here, initially can be treated with a bite registration and construction of a MORA appliance. The patient wears the MORA during all waking hours and removes it only to brush his or her teeth.3-8
The Towne’s view radiograph showed no fracture of the condylar neck. This is always a concern when dealing with TMD and orofacial pain patients. Final full-opening posture was straight and symmetrical. The lateral skull radiograph is excellent for diagnosing cervical degeneration in C5 through C7.9,10 This is important because TMD patients often require multidisciplinary treatment. This patient had a normal C5 through C7 lateral skull radiograph. BioJVA™ (BioResearch Associates Inc, Milwaukee, WI) is a diagnostic aid that objectively detects pathology in the jaw joints during function. It can be used to aid the detection of TMD at an accuracy rate greater than 90%.11-14 According to the American Dental Association, every dentist is required to diagnose jaw joint pathology.
This patient presented with a Wilkes stage II internal derangement (disc displacement with reduction, Figure 3). Resting and functional EMGs recorded with the Bio-EMG II™ (BioResearch Associates Inc) were used to diagnose how the muscles of the stomatognathic system were functioning with the existing occlusion and also how well they relaxed at rest.14-24 Muscles that function abnormally often do not rest normally either. This can cause pain and tension in the TMD patient. This patient presented with extremely high resting EMGs for the temporalis, masseter, and sternocleidomastoid muscles. This illustrated that the chronic malfunctioning of this patient’s occlusion, along with a chronic history of clenching and forward head posture, was creating a pathological situation that did not allow the muscles to rest adequately. The muscles, joints, and whole body posture were being affected negatively, creating a dwindling spiral that ultimately broke down the whole stomatognathic system and affected this patient’s entire body. The functional EMG recordings indicated the temporalis and masseter muscles had poor left–right symmetry during clenching. This muscle pathology is consistent with poor orthopedic and occlusal schemes where the patient is forced to go through “muscular gymnastics” to facilitate chewing, swallowing, and breathing. The jaw-tracking range of motion and velocity tests (recorded with the JT-3D™, BioResearch Associates Inc) revealed a maximum opening of 41.4 mm. Left lateral excursion was 7 mm, and right lateral excursion was 8 mm. Protrusion was 7 mm. This is considered to be at the low end of a normal range of motion. However, the velocity trace showed an opening speed of only 250 mm/sec and a closing speed of 200 mm/sec, indicating bradykinesia (slow movement). Normal opening and closing speeds should be in excess of 350 mm/second.25-28 A normal opening and closing velocity is consistent with normal muscle and jaw joint function. When there is pathologic opening and closing velocity, there is a potential for muscle and/or TMJ dysfunction.
Bradykinesia is slow movement and commonly is associated with dyskinesia (erratic movement). It can be an indication of a disc that is reducing and displacing. In this patient, there was a significant slowdown present right before the teeth contacted at centric occlusion. This pathology was consistent with intracapsular trauma and the body’s sensory proprioception protecting against additional trauma associated with tooth contact. Ultimately, this pathology puts pressure on the condyle intracapsularly. When there is damage intracapsularly, which is associated with inflammation, the body braces to protect itself.28,29 Intraoral and extraoral photographs revealed a patient with a large number of old failing restorations, including fillings, root canals, crowns, and bridges. The occlusal pattern was irregular overall. There was generalized type III bone loss. Also noted on the models and in the examination was upper/lower loss of transverse arch form. The maxillary arch form was anteriorly “V” shaped with central incisor overlap. The mandibular arch form was also narrow anteriorly and had general anterior crowding with tooth No. 22 blocked out (Figure 4 and Figure 5). This orthopedic condition significantly affects the TMJ because the occlusion will displace the condyles posteriorly and superiorly. 30,31 This has a negative impact on joints, muscles, and airways. The blocked out tooth No. 22 and upper/lower crowding directly impact the treatment process because of the limitations of crown-and-bridge alone. This patient required orthopedic and orthodontic treatment. The extraoral photographs illustrated noticeable forward head posture.
This structural posture is a person’s adaptation to facilitate swallowing, and/or is seen in someone who has become a mouth breather. These functioning adaptations significantly affect diagnoses and treatment plans. The subjective questionnaire revealed that the patient’s chief complaints were headaches, jaw clicking, shoulder pain, neck pain, pain when chewing, and appearance. The patient was healthy overall. She had had her tonsils and wisdom teeth removed. She had right-sided frontal, temporal, and back-of-the-head headaches. She was aware of daytime and nighttime clenching. She had a previous accident where she was struck violently on her mandible. Her history indicated that her pain patterns started thereafter and she had been in chronic pain for many years. She had experienced occasional numbness in her fingers. She experienced chronic vertigo. She wakened with a dry mouth in the morning.
Diagnosis
The patient was diagnosed with bilateral Wilkes stage II anterior disc displacement with reduction, bilateral capsilitis, bilateral myalgia, right-sided headache/facial pain, and chronic clenching.
Treatment Plan
The treatment plan consisted of three phases.
Phase 1:
- Clean up existing dentistry, removing all dental and periodontal pathology
- Realign mandible (condyles) orthopedically
- Reduce adverse joint loading
- Improve function
- Improve myalgia
- Reduce pain
Phase 2:
- Transversely develop upper and lower arches orthopedically
- Rotate, level, and align dentition on upper and lower arches (braces)
Phase 3:
- Full-mouth prosthetic reconstruction to the correct orthopedic and functional relationship
- Improve cosmetics
Consultation
It was explained to the patient that her problems were associated predominantly with soft-tissue issues of the jaw joint with early degeneration. Her other problems were overworked muscles, which were not getting adequate rest. Finally, it was explained to her that the maxillary and mandibular dental and orthopedic arches needed to be developed transversely. The patient was informed that the total treatment time would be approximately 2.5 years, start to finish. The patient agreed to treatment and signed informed consent forms.
Phase 1
The patient was sent to a periodontist for bone grafting and general periodontal treatment. After the completion of periodontal treatment, the author removed all of her existing dental work, with the exception of old conservative fillings. These fillings were not a liability of later needing root canals, and they would be removed in Phase 3 when the teeth were prepped for the full-mouth rehabilitation. Through the course of cleaning up the existing dentistry, teeth Nos. 19, 29, and 30, which had old failing crowns and advanced decay, were treated by extraction. The remainder of the teeth were restored with healthy restorations, buildups, and temporary crowns. The teeth and periodontia were then healthy and could support the complete treatment. Orthopedic realignment of the condyles started with a bite registration. Because the patient had bilateral retrodiscitis (TM inflammation) and disc displacements, and needed anterior/posterior correction, the phonetic bite registration technique was used.32-34 The phonetic bite technique provides the limit of anterior/posterior movement of the mandible (Figure 6 and Figure 7). Additionally, the phonetic bite achieves significant improvement in the airway. From the phonetic bite registration and upper and lower impressions, a neuromuscular demand appliance (NDA) was made for the patient to wear during all of her waking hours. This orthotic, in essence, resets the jaw orthopedically to enable the condyle the opportunity to recapture the disc. In addition, the orthotic, by moving the condyle in a down and forward position, decompresses the joints allowing for healthy blood flow, and the elimination of pressure on retrodiscal nerves and blood vessels35-37 (Figure 8 and Figure 9).
Ultimately, the NDA aids in eliminating inflammation of the joint capsule, which previously was caused by occlusal and parafunctional trauma. At night a separate orthotic was used, which was a nighttime deprogrammer with a palatal ramp. This appliance, an anterior discluder, keeps the condyles, mandible, and muscles in a posture that is consistent with the occlusal trajectory established with the day appliance. In addition, the posterior teeth do not touch, significantly eliminating night clenching.38-40 Finally, by holding the jaw in position at night and combining this with patient functioning in the NDA orthotic in the daytime, the musculature will reprogram to this position and the TMJ capsules will adapt to the condyles’ new posture. These two orthotics, worn over a period of 3 to 4 months, set the foundation for the subsequent Phase 2 and Phase 3 treatments.
In addition to wearing the appliances, the patient had subsequent trigger point, ligament insertion, and prolotherapy injections. She also had the chiropractor do some cervical adjustments. After 8 weeks of therapy, the patient reached maximum medical improvement (MMI). All of her pain issues were gone. The final Phase 1 records were taken, including new tomograms, cephalograms, bitewing and perioapical radiographs, JVA, EMGs, and jaw-tracking records. The records showed objectively that she had reached MMI.
Phase 2
The orthopedic position established in Phase 1 was maintained in Phase 2 by constructing anterior composite incisal ramps/blocks for the lower anterior incisor occlusion. In the posterior, occlusal blocks were built on the occlusal surface of the second molars. This tripod (Figure 10) maintained the jaw and bite trajectory, which was established in Phase 1 through the NDA and the nighttime deprogrammer with palatal ramp. With this functional tripod established, the Phase 2 goals of orthopedic expansion could be accomplished as well as the orthodontic goals of rotating, leveling, and alignment. The upper-arch orthopedic development was accomplished through a fixed Hyrax expansion appliance (Figure 11 and Figure 12). The lower arch development was accomplished along with the upper arch and through use of straight wire techniques (Figure 13 and Figure 14). Final coupling of the dentition was accomplished through verticalization with eruption of the teeth through elastics. Phase 2 took 13 months. The patient then was placed in retention for an additional 6 months (Figure 15).
Phase 3
With the completion of Phase 2, the patient was ready to start Phase 3, full-mouth reconstruction to optimal dental physiology. This process started by constructing the upper and lower arch bite-registration stent out of Sil-tech (Ivoclar Vivadent Inc, Amherst, NY). This bite registration stent was constructed from the upper and lower models mounted on the articulator. The mounting was from the current complete orthopedic/orthodontic relationship established in Phase 2. The bite-registration stent allowed the author to prepare the teeth and then put a wash in the stent for the upper and lower prepped teeth, which maintained the relationship established in Phase 1 and Phase 2. After construction of the bite-registration stent, the upper and lower models were prepped and both dental arches were waxed up in an ideal relationship (Figure 16).
From this waxup, a triple-tray temporary stent was constructed. The design of the temporary stent enabled the preparation of both arches in a single visit. The temporization of the occlusion maintained the relationship established in Phase 1 and Phase 2. The patient had both arches prepped and temporized. After 3.5 weeks, the permanent restorations were placed. The following day, the final restorations were fine-tuned with computerized occlusal analysis. The laboratory constructed a new nighttime deprogrammer with a palatal ramp for the patient to wear every night. This appliance would protect against nighttime parafunction and maintain a healthy airway.
The patient returned 1 month later for computerized occlusal analysis. The analysis objectively confirmed that the occlusion was balanced and right and left cuspid disclusion as well as protrusion were immediate and measurable to less than 0.2 seconds. The patient was reevaluated at 6 months, 1 year, and 3 years posttreatment. Her symptoms have not returned. Follow-up examinations using biometric instrumentation objectively show normal healthy muscle function, normal jaw function, normal swallowing, and a normal airway. The patient is ecstatic with her final result (Figure 17 through Figure 19).
CONCLUSION
This case study illustrates the intimate relationship between how teeth interdigitate and the impact interdigitation has on the whole body. The patient presented with chief complaints of jaw clicking and popping, jaw joint pain, headaches, bad bite, and dislike of the appearance of her teeth. The patient went through three phases of treatment over a period of approximately 2.5 years. The phases dealt with her physiologic chief complaints, enhanced her orthopedic arch form, straightened her teeth and, finally, prosthetically restored her entire mouth.
The entire treatment plan was established by using extensive record gathering through radiographic and computerized electrodiagnostic modalities. In this patient, many different sources of record gathering were used to diagnose the cause of the patient’s chief complaints before treatment and ultimately to direct the course of treatment. The occlusion was examined by mounting models on an orthopedic articulator. This mounting showed the relationship of the occlusal plane of the teeth to the maxilla, mandible, and jaw joints. The function of the joints was assessed objectively by JVA. The function of the muscles was assessed objectively by EMG. These assessments illustrated pathologic muscle resting and functional activity.
The functional activities assessed were clenching, chewing, and swallowing. The degenerative and pathologic bony orthopedics were diagnosed from various craniomandibular radiographs. These radiographs illustrated improper neck curvature in the cervical vertebra, bony apposition associated with clenching, and displaced TMJ posture bilaterally. All of the observed diagnostic modalities directly influenced the course of treatment selected for this patient. The completed treatment was subjectively and objectively very successful, with the patient doing well 3 years after treatment.
REFERENCES
1. Conti PC, Miranda JE, Araujo CR. Relationship between systemic joint laxity, TMJ hypertranslation and intra-articular disorders. Cranio. 2000;18(3):192-197.
2. Carlson J. Occlusal diagnosis. Midwest Access. Seattle, Washington.
3. Kaufman A, Kaufman RS. Use of the MORA to reduce headaches on members of the U.S. Olympic Luge Team. Basal Facts. 1983;5(4):129-133.
4. Pertes RA. Updating the mandibular orthopedic repositioning appliance (MORA). Cranio. 1987;5(4):351-356.
5. Pertes RA, Attanosio R, Cinotti WR, et al. Occlusal splint therapy in MPD and internal derangements of the TMJ. Clin Prev Dent. 1989;11(4):26-32.
6. Brown DT, Gaudet EL Jr, Phillips C. Changes in vertical tooth position and face height related to long term anterior repositioning splint therapy. Cranio. 1994;12(1):19-22.
7. Niemann W. The bicuspid block MORA convertible appliance. Funct Orthod. 2004;21(1):12-26.
8. Tecco S, Caputi S, Teté S, et al. Intra-articular and muscle symptoms and subjective relief during TMJ internal derangement treatment with maxillary anterior repositioning splint or SVED and MORA splints: a comparison with untreated control subjects. Cranio. 2006;24(2):119-129.
9. Hendriksen IJ, Holewijn M. Degenerative changes of the spine of fighter pilots of the Royal Netherlands Air Force (RNLAF). Aviat Space Environ Med. 1999;70(11):1057-1063.
10.Tanaka H, Nakamura K, Kurokawa T, et al. Roentgenological measurement of the cervical vertebral bodies in ossification of the posterior longitudinal ligament (OPLL) and cervical spondylosis (CS) (author’s transl) [in Japanese]. Nippon Seikeigeka Gakkai Zasshi. 1981;55(7):635-645.
11.Bessette RW. A clinical study of temporomandibular joint vibrations in TMJ dysfunction studies. Paper presented at: American Academy of Head, Neck Facial Pain, and TMJ Orthopedics; August 15, 1992; Kansas City, MO.
12.Ishigaki I, Bessette RW, Maruyama T. Vibration of the temporomandibular joints with normal radiographic imagings: comparison between asymptomatic volunteers and symptomatic patients. Cranio. 1993;11(2):88-94.
13.Ishigaki S, Bessette RW, Maruyama T. Vibration analysis of the temporomandibular joints with meniscal displacement with and without reduction. Cranio. 1993;11(3):192-201.
14.Widmalm SE, Lee YS, McKay DC. Clinical use of qualitative electromyography in the evaluation of jaw muscle function: a practitioner’s guide. Cranio. 2007;25(1):63-73.
15.Kerstein RB, Radke J. The effect of disclusion time reduction on maximal clench muscle activity levels. Cranio. 2006; 24(3):156-165.
16.Scopel V, Alves da Costa GS, Urias D. An electromyographic study of masseter and anterior temporalis muscles in extraarticular myogenous TMJ pain patients compared to an asymptomatic and normal population. Cranio. 2005;23(3):194-203.
17.Mahony D. Refining occlusion with muscle balance to enhance long-term orthodontic stability. J Clin Pediatr Dent. 2005;29(2):93-98.
18.Acosta-Ortiz R, Schulte JK, Sparks B, et al. Prediction of different mandibular activities by EMG signal levels. J Oral Rehabil. 2004;31(5):399-405.
19.Ferrario VF, Sforza C, Tartaglia GM, et al. Immediate effect of a stabilization splint on masticatory muscle activity in temporomandibular disorder patients. J Oral Rehabil. 2002;29(9):810-815.
20.Buzinelli RV, Berzin F. Electromyographic analysis of fatigue in temporalis and masseter muscles during continuous chewing. J Oral Rehabil. 2001;28(12):1165-1167.
21.Kamyszek G, Ketcham R, Garcia R Jr, et al. Electromyographic evidence of reduced muscle activity when ULF-TENS is applied to the Vth and VIIth cranial nerves. Cranio. 2001;19(3):162-168.
22.Levine E. and Levine J. The choice of surface EMG for muscle functional capacity evaluation. AJPM. 1999;9(3):104-108.
23.Sgobbi de Faria CR, Bérzin F. Electromyographic study of the temporal, masseter and suprahyoid muscles in the mandibular rest position. J Oral Rehabil. 1998;25(10):776-780.
24.Ferrario VF, Sforza C, D’Addona A, et al. Reproducibility of electromyographic measures: a statistical analysis. J Oral Rehabil. 1991;18(6):513-521.
25.Cooper BC. The role of bioelectronic instrumentation in the documentation and management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;83(1):91-100.
26.Cooper BC. Parameters of an optimal physiological state of the masticatory system: the results of a survey of practitioners using computerized measurement devices. Cranio. 2004;22(3):220-233.
27.Monaco A, Cozzolino V, Cattaneo R, et al. Osteopathic manipulative treatment (OMT) effects on mandibular kinetics: kinesiographic study. Eur J Paediatr Dent. 2008;9(1):37-42.
28.Branch TP, Hunter R, Donath M. Dynamic EMG analysis of anterior cruciate deficient legs with and without bracing during cutting. Am J Sports Med. 1989;17(1):35-41.
29.Kumar S, Ferrari R, Narayan Y. Cervical muscle response to head rotation in whiplash-type right lateral impacts. J Manipulative Physiol Ther. 2005;28(6):393-401.
30.Shino T, Kawabata K, Nojima K, et al. Morphological study on quadruplets by cephalometric and model analyses. Bull Tokyo Dent Coll. 2007;48(1):19-26.
31.Baccetti T, Franchi L, McNamara JA Jr, et al. Early dentofacial features of class II malocclusion: a longitudinal study from the deciduous through the mixed dentition. Am J Orthod Dentofacial Orthop. 1997;111(5):502-509.
32.Pound E. Let /S/ be your guide. J Prosthet Dent. 1977;38(5): 482-489.
33.Mehnert T. Investigations on the relation of dysgnathias and S-sound pronunciation. J Oral Rehabil. 1987;14(1):95-103.
34.Jeliciç D, Panteliç Z, Dimitrijeviç M. Phonetic method for the determination of the physiologic rest of the mandible by graphic registration [in Croatian]. Stomatol Vjesn. 1968;2(1-6):435-440.
35.Wish-Baratz S, Ring GD, Hiss J, et al. The microscopic structure and function of the vascular retrodiscal pad of the human temporomandibular joint. Arch Oral Biol. 1993;38(3):265-268.
36.Pereira FJ, Lundh H, Eriksson L, et al. Microscopic changes in the retrodiscal tissues of painful temporomandibular joints. J Oral Maxillofac Surg. 1996;54(4):461-469.
37.Cooper B, Oberdorfer M, Rumpf D, et al. Trauma modifies strength and composition of retrodiscal tissues of the goat temporomandibular joint. Oral Dis. 1999;5(4):329-336.
38.Yap AU. Effects of stabilization appliances on nocturnal parafunctional activities in patients with and without signs of temporomandibular disorders. J Oral Rehabil. 1998;25(1):64-68.
39.Kawazoe Y, Kotani H, Hamada T, et al. Effect of occlusal splints on the electromyographic activities of masseter muscles during maximum clenching in patients with myofascial pain-dysfunction syndrome. J Prosthet Dent. 1980;43(5):578-580.
40.Goldstein L, Gilbert LM. Use of the BEST-BITE anterior discluder for the treatment of migraine headache: a case study. Funct Orthod. 2004;21(2):34-37.
About the Author
Jim K. Beck, DDS
Private Practice, Pueblo, ColoradoFeatured Speaker at the 2009 BioRESEARCH Annual Conference
 Figure 1 The patient was unhappy with the esthetics of her smile. Note the uphill cant to the left. |  Figure 2 Several occlusal flags included crowded anteriors and abfractions. |  Figure 3 Joint vibration analysis showing stage II anterior disc displacement with reduction. |
 Figure 4 Pretreatment upper study model. Crowded maxillary anteriors and “V”-shaped arch form. |  Figure 5 Pretreatment lower study model. Crowded mandibular anteriors, “V“-shaped arch form, and blocked out tooth No. 22. |  Figure 6 The patient’s habitual bite. Note the anterior overjet and the relationship of molars and cuspids. |
 Figure 7 Note the anterior/posterior and vertical change from phonetic bite registration. | 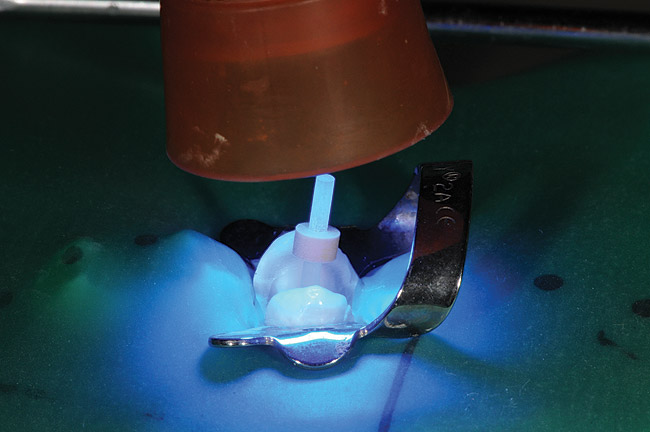 Figure 8 Left-side habitual bite condylar posture. |  Figure 9 Left-side phonetic bite registration posture from which the MORA appliance was constructed. |
 Figure 10 Tripod transfer established from Phase I orthotic after MMI was established. |  Figure 11 Hyrax transverse expansion appliance with rectangular wire to establish proper torque. |  Figure 12 Upper-arch clean up, orthopedic expansion, and orthodontics completed. |
 Figure 13 Note the rectangular wire used to create ideal torque. |  Figure 14 Lower-arch clean up, orthopedic expansion, and orthodontics completed. |  Figure 15 Removable retention that was used for 6 months. |
 Figure 16 Final upper and lower waxup, maintaining the established position. The temporary stent was made from the waxup. |  Figure 17 Completed case, right-side view. |  Figure 18 Completed case, left-side view. |
 Figure 19 Completed case. The patient was pleased with her final smile |