The Advantages of Photogrammetry in Implant Dentistry
A discussion with Blake Roney
Blake Roney, digital solutions manager for S.I.N. Dental USA, is a CAD/CAM dental technician with a degree in engineering graphics. Considered to be a leading expert in photogrammetry, he is a CAD software trainer and was the recipient of the "Masters of the Craft" award at LMT'S LAB DAY Chicago 2020. Inside Dentistry recently spoke to Roney about photogrammetry and its uses in dentistry.
Inside Dentistry (ID): What is photogrammetry?
Blake Roney (BR): Photogrammetry is the science of obtaining 3D measurements and information about physical objects using 2D photographs. It involves analyzing and interpreting 2D images acquired from multiple angles to create 3D models or maps of the photographed objects that incorporate accurate measurements.
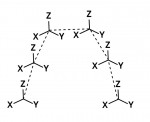
In photogrammetry, photographs are acquired from various angles with specialized cameras, and then the images are processed using software to create a 3D model or map of the photographed objects. The process involves determining the positions and orientations of the cameras, calculating the spatial relationships between the images, and extracting 3D information from the images to create a detailed and accurate representation of the subject.
ID: How is photogrammetry used in dentistry?
BR: In dentistry, photogrammetry is used to capture data about implant placement for full-arch prostheses. Special scan bodies are placed on top of the implant abutments (Figure 1), and an extraoral scanner is used to record very precise data about the location and angulation of the abutments. Because the traditional methods of capturing implant data for full-arch restorations were either inaccurate or labor and time intensive, the use of dental photogrammetry systems (eg, ICam4D, Imetric; MicronMapper, ClaroNav; PIC system, PIC dental) can be seen as the missing piece in providing predictable and efficient fully digital full-arch restorations.
ID: Why can't clinicians just use their intraoral scanners?
BR: With photogrammetry, clinicians still use their intraoral scanners. Photogrammetry scanners are actually useless by themselves. Currently, photogrammetry scanners only capture data about where implants are located and their relationships to each other, so an intraoral scanner is still needed to capture the surface of the tissue and the bite relationship between the two jaws.
ID: Ok, but why can't clinicians just use their intraoral scanners to capture the implant data as well?
BR: Intraoral scanners and traditional scan bodies work great for cases involving single unit implant restorations and small bridges, but due to the nature of these scanners being intraoral, they are only capturing small sections of data at a time and then "stitching" each of these small scans together. In contrast, photogrammetry scanners are extraoral, so they can capture all of the scan bodies at one time. This allows them to not only measure where one implant is located in 3D space but also more accurately record the relationships between multiple implants (Figure 2).
ID: How is this better than traditional analog methods?
BR: Going fully digital with photogrammetry allows you to reduce the "time to teeth" for patients. No longer will you need to schedule an entire appointment just to make a verification jig for a stone model. So, although paying $35,000 to $45,000 for these scanners up front sounds like a lot, the downstream savings on materials and time add up fast.
ID: Exactly how accurate are dental photogrammetry systems?
BR: People always ask for the accuracy of the scanners to be described using a single value, such as "accurate down to 15 microns," but like most things in life, the truth is much more complicated. The Co-CEO of ClaroNav, Doron Dekel, does a great job of addressing this in his most recent white paper on the MicronMapper, in which he explains that there is currently no standard and verifiable process to obtain such a value. In my opinion, clinicians should be wary of vendors selling 3D scanning equipment who provide an accuracy measurement as a single value without explaining their methods. Many factors, including the number of implants involved, the circumstances of the test, and the methodology used to calculate the results down to a single value, should be considered. However, the first question that we should be asking is what clinically significant amount of error is still acceptable for a passive fit? A review of the currently available literature suggests that a root mean square error of 50 µm to 100 µm with less that 1° of deviation will be passive in most clinical cases, and current studies have shown that, in most cases, all of the available photogrammetry systems fall within this acceptable range.
ID: Can designers use the data in their current software applications?
BR: Absolutely. Most designers can incorporate this data into the software that they're already using. All of the available photogrammetry systems have a library or workflow for using their data in common dental CAD software applications, such as exocad and 3Shape.
ID: Is it only for multi-unit abutments?
BR: This depends on which system you use. The scan bodies for both ICam4D and MicronMapper are currently only for multi-unit abutments. The PIC system does offer scan bodies for direct-to-implant restorations; however, I personally don't want to design a full-arch restoration that is not on multi-unit abutments. Without multi-unit abutments for angle correction, it's much harder to design an all-on-X prosthesis that has a passive fit. Going direct to implant would also require you to use some type of metal interface between the prosthesis and the implants, such as a titanium base. Photogrammetry on multi-unit abutments allows us to design directly to the multi-unit abutments with no titanium interface.
ID: What are the benefits of going direct to multi-unit abutments?
BR: Going direct to multi-unit abutments means that there is no titanium interface between the all-on-X restoration and the multi-unit abutments (Figure 3 and Figure 4). Titanium bases debonding from bridges is a common failure mode in our field, and this workflow completely eliminates that issue. It also allows for a much smaller hole to be milled in the bridge when compared with the large interface required for a titanium base. Although there is currently no long-term data on this method because it's so new, the initial results appear promising. So, ask me in 5 to 10 years how these all-zirconia bridges are holding up, but to me, it seems like bridges with more zirconia would have to be stronger, right?