Computer-Guided Implant Surgery
Improving predictability of placement for practitioners new to implant dentistry
Joseph V. Califano, DDS, PhD | Michael C. Taylor, DMD
Successful dental implants result from careful, prosthetically driven treatment planning,1,2atraumatic surgical placement, proper restoration, and regular maintenance. Success has been defined to include the absence of discomfort or pain, implant immobility, the absence of peri-implant radiolucency, negligible progressive bone loss, and an implant position that allows the placement of an esthetic and functional prosthesis.3 Implant failure can occur shortly after placement, but prior to restoration. This is referred to as an early failure. In these cases, the implant does not achieve proper osseointegration after placement. Late failure can occur when there is a period of uneventful healing and osseointegration, but the implant later fails after it is restored and placed into function. Early failure is often related to the surgical procedure. It can occur as a result of surgical trauma, infection, occlusal overload during healing, an absence of keratinized gingiva, or a poor placement position that compromises or prevents restoration. Late failure can also be caused by many factors, such as an improper occlusal scheme that results in heavy and/or non-axial forces on the implant. In addition, the loosening of a screw that is retaining an implant restoration or an implant abutment can result in unfavorable forces on the implant and ultimately lead to failure. Dental implants can also exhibit plaque-induced, peri-implant inflammation and bone loss analogous to periodontitis.4,5 This may be the result of local factors contributing to plaque accumulation, such as excess retained cement or unfavorable restoration contours. Genetically controlled host factors similar to those associated with periodontitis may also be important because implant patients who have a history of periodontitis are at greater risk of developing peri-implantitis.6
Many of the challenges that result in implant failure can be avoided with proper planning and surgical execution that places the implant atraumatically in an ideal position. Implants placed in ideal positions facilitate esthetic restorations with optimal contours that are not plaque retentive. Proper implant position also allows for an occlusal scheme that promotes light contact in centric occlusion with minimal or no contact in excursions to eliminate or minimize non-axial forces.7
Prosthetically Driven Placement
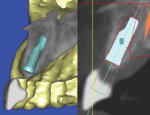
Planning for surgical implant placement is prosthetically driven. Therefore, at a minimum, it begins with mounted diagnostic study models and two-dimensional imaging. From this, a conventional surgical guide can be fabricated that brings the prosthetic information to the surgery. With surgical placement utilizing a conventional surgical guide, decisions regarding the ideal implant position are made intraoperatively after flap reflection. The three-dimensional relationship of the available alveolar bone and the desired prosthesis as indicated by the surgical guide helps determine the position (Figure 1 through Figure 6). Alternatively, planning can be accomplished by importing a cone-beam computed tomography (CBCT) scan into interactive implant planning software.1 Implants can be placed virtually on the computer where the software merges anatomical and prosthetic information in three dimensions. This allows decisions regarding the ideal implant position to be made preoperatively (Figure 7). Information from the virtual plan can then be used to fabricate a computer-generated surgical guide that precisely controls the osteotomy preparation and surgical placement of the implant (Figure 8 through Figure 14). In some cases, the software can facilitate fabrication of a provisional restoration in advance of the surgery (Figure 15 through Figure 19). Ideal implant placement also supports a functional and esthetic final restoration (Figure 20 through Figure 21).
After several years of specialty training in dental implant surgery in an academic environment, a dentist can predictably place implants with either the conventional or digital approach. However, for the private, general practitioner who is new to implant dentistry, it can be difficult to acquire the knowledge and skill necessary to predictably accomplish ideal implant placement. Un-fortunately, opportunities for patient-based, hands-on training in implant surgery are limited outside of postgraduate residency programs in academic institutions. Therefore, for dentists interested in placing implants, virtual planning and computer-generated surgical guides can be helpful in achieving ideal implant placement.
Benefits of Digital Education
The residents in the Department of Perio-dontology at the Oregon Health and Science University (OHSU) School of Dentistry utilize both conventional and computer-generated surgical guides. When residents surgically place implants for the patients of the predoctoral dental students, the implant placement is exclusively virtually planned and the implant is placed using a computer-generated guide. The faculty in the Department of Perio-dontology recently decided to restrict the predoctoral implant program to the use of this technology to enhance the predoctoral students' understanding of implant dentistry and increase their participation in the treatment planning process. The school's experience during the last several years has indicated that in addition to improving the learning opportunities for predoctoral students, emphasizing the digital approach has greatly improved the surgical outcomes for patients in terms of ideal implant placement. In the past, when the school was only using conventional surgical guides, the faculty found that in some cases, implants were placed in unfavorable positions (Figure 22 through Figure 24). This occurred even though the residents placing the implants received close supervision from experienced attending faculty during the implant surgeries. Although not a frequent occurrence, there was always a small percentage of cases for which the final restoration was compromised due to the position of the implant. For any clinician who was developing his or her skills in conventional implant surgery, it became clear that it was difficult to avoid occasionally placing an implant in a less-than-optimal position. Virtual planning and fabrication of computer-generated surgical guides for implant placement eliminated this problem for implants placed by the school's residents (Figure 25 through Figure 29).
In addition, virtual implant planning affords a complete understanding of the nature of the available bone and its relationship to the desired prosthesis in advance of surgical placement. This has several advantages. When anatomic limitations do not allow implants to be placed in a location that will support an ideal restoration, the periodontal faculty, restor-ative faculty, residents, and students discuss appropriate treatment plan options. It may be possible to redesign the prosthesis so that the available bone is sufficient. Alternatively, a decision to develop the site via bone grafting may allow the originally planned restoration to be placed in an ideal position. Any plans, decisions, or compromises are the result of a collaboration between all of the dentists and laboratory technicians involved in the patient's care. The patient can also be included in the decision-making process. This type of decision-making is often superior to what might occur unilaterally and intraoperatively by the dentist placing the implant. If the implant site is developed via bone grafting, new imaging studies and virtual planning allow for an optimal prosthetic result.
Treatment Planning and Surgical Protocol
The application of computer-guided implant dentistry in clinical practice and factors important to its successful implementation have been reported previously.8 In the planning software, anatomic information from a CBCT scan is merged with prosthetic information that is derived from either a diagnostic wax-up on mounted study models (for the partially edentulous patient) or from an existing interim or final complete denture (for the completely edentulous patient). For a partially edentulous patient, a diagnostic wax-up of the desired prosthesis is created, duplicated in dental stone, and scanned with a digital scanner to yield a so-called "stereolithography" or "STL" file. For a completely edentulous patient, special stick-on, radiopaque radiographic markers are temporarily added to the denture. A CBCT scan is then captured with a radiolucent bite registration in place to ensure freeway space between all of the patient's natural or prosthetic teeth. For completely edentulous patients, dentures are also scanned by CBCT outside of the patient's mouth with the radiographic markers still in place. For the partially edentulous patient, prosthetic information from the STL file and the CBCT scan are imported into the planning software. For the completely edentulous patient, the CBCT scans of the patient with the denture and the denture alone are imported into the planning software.
Once the anatomic and prosthetic data are merged in the planning software, implants can then be virtually placed in the alveolar bone in a position to support the prosthesis. The implants can be viewed in cross-sectional, panoramic, axial, and 3D views, and their positions can be adjusted in all views until they are ideal (Figure 7). Next, a stereolithographic, computer-generated guide is fabricated to assist in the osteotomy preparation and implant placement (Figure 8 through Figure 14). This process has been studied and found to be extremely reliable and precise.9
Utilizing a CBCT scanner with interactive planning software in this fashion can sig-nificantly enhance the treatment planning process as well as the precision of surgical implant placement. Like all dental procedures, this process requires considerable attention to detail. At each step, any errors that occur will be incorporated into the surgical guide and then precisely transferred to the patient during surgery.8 For example, the mounted study models and the wax-up of the prosthesis must accurately represent the patient and the desired final prosthesis because the virtual planning of the implant position is directly related to their accuracy. For complete denture patients, the prothesis must be fully seated during the CBCT scan without any gaps between the edentulous ridges and the denture. This is facilitated by the radiolucent bite registration. During surgery, the computer-generated surgical guide must be fully seated on the remaining natural teeth, bone, or edentulous ridge. In some cases, the stability of the guide can be enhanced with fixation screws during the osteotomy preparation. A full discussion of possible sources of error in this process has been reported.8
It is important for clinicians who surgically place implants with computer-generated guides to avoid the tendency to completely rely on the guide without verifying its accuracy. Once it is determined that the guide is fully seated, the drill should be inserted into the guide, and its relationship to the crowns and root eminences of the existing natural teeth should be examined and verified. The relationship should present as expected based on printed images from the virtual plan made in advance of the surgery. It is useful to have a vacuform matrix from the wax-up with holes in the planned implant sites available to help verify the accuracy of the osteotomy preparation as the surgery proceeds with the first twist drill (Figure 30). In very rare cases, a practitioner might find that something is not as expected, and the surgery will either need to be aborted or completed using a conventional guide derived from the wax-up. The vacuform matrix can serve as a conventional surgical guide in this situation.
In some cases, the computer-generated guide can be used in a flapless surgical approach (Figure 8 through Figure 14). Flapless surgery, however, should be considered with extreme caution. If the osteotomy preparation is in close proximity to natural teeth or other anatomical structures, flapless surgery may not be indicated.8 Although the flapless surgical technique has been marketed as a way for a clinician with limited surgical experience to place implants, flapless surgery actually requires a greater amount of experience with implant placement because it affords much less opportunity to verify the accuracy of the guide during the procedure.8
Conclusion
The process of ideal implant planning and surgical placement is prosthetically driven, technically challenging, and requires con-siderable training and experience to execute well. Computer software that facilitates virtual implant planning and placement can enhance the dental implant treatment plan. Furthermore, utilizing computer-generated surgical guides derived from such a plan can improve the predictability of achieving an optimal surgical placement. This results in functional and esthetic implant restorations that are optimal treatment outcomes for patients.
About the Authors
Joseph V. Califano,
DDS, PhD
Professor of Periodontics
Oregon Health and Science University
School of Dentistry
Portland, Oregon
Michael C. Taylor, DMD
Assistant Professor
Oregon Health and Science University
School of Dentistry
Portland, Oregon
References
1. D'Haese J, Ackhurst J, Wismeijer D, et al. Current state of the art of computer-guided implant surgery. Periodontol 2000. 2017;73(1):121-133.
2. Elian N, Ehrlich B, Kim GU. Complications associated with implant planning: etiology, prevention, and treatment. In: Froum SJ, ed. Dental implant complications: etiology, prevention, and treatment. 1st ed. West Sussex, UK: Wiley-Blackwell;2010:46-67.
3. Smith DE, Zarb GA. Criteria for success of osseo-integrated end-osseous implants. J Prosthet Dent. 1989;62(5):567-572.
4. Mombelli A, Muller N, Cionca N. The epidemiology of peri-implantitis. Clin Oral Implants Res. 2012;23(Suppl 6):67-76.
5. Lindhe J, Meyle J, Group D of European Workshop on Periodontology. Peri-implant diseases: consensus report of the sixth european workshop on periodontology. J Clin Periodontol. 2008;35(8 Suppl):282-285.
6. Heitz-Mayfield LJ. Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol. 2008;35(8 Suppl):292-304.
7. Siddiqui AA, O'Neal R, Nummikoski P, et al. Immediate loading of single-tooth restorations: one year prospective results. J Oral Implantol. 2008;34(4):208-218.
8. Califano JV, Rosenfeld AL, Mandelaris GA. A logical and progressive approach to computed tomography-guided implantology. Clinical Advances in Periodontics. 2012;2(4):263-273.
9. Testori T, Robiony M, Parenti A, et al. Evaluation of accuracy and precision of a new guided surgery system: a multicenter clinical study. Int J Periodontics Restorative Dent. 2014;34 Suppl 3:s59-69.