CBCT Planning for Successful Immediate Implant Placement
Implant planning for better predictability and accuracy
Datta Malyavantham, BDS, DDS, FICOI
Implant placement requires precision and planning for successful osseointegration and restoration. Radiographic techniques, including intraoral, panoramic, and cephalometric imaging, are the conventional methods for implant treatment planning.1 However, these techniques limit proper evaluation, as they only provide a 2-dimensional image of the mesial-distal and occlusal-apical anatomy.2 Additionally, the most important criteria for implant selection and success is the availability of adequate occlusal-apical bone height and the buccal-lingual width and angulation.2 With traditional radiographs, neither buccal-lingual width nor angulation can be determined.2
Panoramic radiographs have also been shown to overestimate implant length during treatment planning because of the inherent magnification in the imaging process.3,4 Overestimating implant depth can result in injury to adjacent anatomical structures (eg, floor of the maxillary sinus, inferior alveolar nerve) during and after implant placement.5 Additional complications from imaging distortion and superimposition can compromise the accuracy of treatment planning with conventional techniques. Recently, tomographic techniques for implant treatment planning were introduced to more accurately plan and place implants and prostheses.
Benefits of Cone-Beam Computed Tomography
Clinicians began using cone-beam computed tomography (CBCT) for treatment planning to control implant placement with a higher degree of accuracy.6-8 This technology allows clinicians to determine the most suitable area for implant placement so that bone grafting can be avoided.9 CBCT scans capture very critical information essential to determining implant size and angle, including height, width morphology, and density of the alveolar bone surrounding the implant site.10-12 It also helps to avoid complications such as inferior alveolar nerve injury because it allows for presurgical mapping of the inferior alveolar canal and its proximity to the lingual concavity in the posterior mandible regions.13 Research demonstrates that using CBCT for bone density assessment is significantly correlated with implant stability, improving predictability and efficiency of implant planning and placement.14 CBCT scanning has also proven helpful in confirming placement and osseointegration after surgery.
Historically, dental CBCT scans were used to plan implant placement, but the surgical drill guides were handmade by clinicians or laboratory technicians using cold-cure or processed acrylic.15 Although the early drill guides did not have the capacity to integrate CBCT data into the surgical plans,15 the development of computer-planning methods allowed clinicians to use fiducial markers to relate the CBCT data to the prosthetic plan.16,17 Dental implant drill guides were then created using the planned trajectories of the fiducial markers’ position in 3-dimensional (3D) space from the CBCT scan.16,17 Using the implant trajectories, the handmade radiographic guides were converted into surgical drill guides.15
Although CBCT imaging helps to increase the accuracy of immediate implant loading, handmade surgical guides are more susceptible to complications, including inaccurate implant depth, extensive surgery time, poor visibility, and inconsistencies inherent with handmade guides. Now, software-based treatment planning allows for the development of patient-specific, computer-generated CT-guided drill templates.15 Using CBCT scans along with radiographic templates and surgical simulation software offers unparalleled diagnostic accuracy.16 Rapid manufactured output from the software-planned dental implant trajectories into the bone have made it possible to create bone-borne and tooth-borne surgical drill guides.
Additionally, computer-generated surgical guides provide more predictable placement and accuracy. Designed for the drill to stop at the precise position and depth planned, this tool saves valuable time, simplifying the implantology process and creating an open field of view during surgery.
Although CBCT imaging is helpful in treatment planning, selecting the appropriate implant can be challenging. Complications from poor implant placement include inaccurate abutment seating, rotational engagement, poor bone-to-implant contact at the crestal zone, pressure on the cortical bone, time-consuming treatment, and poor stability. Using implants with internal hexagon connections provides a better fit between the implant and the abutment, minimizing micro-movements and reducing bone resorption. Micro-rings at the neck of the implant increase the bone-to-implant contact, avoiding bone resorption at the neck. With the ideal implant, surgical guide, and technology, implantology can become an efficient and accurate treatment.
Case Presentation
A 60-year-old man presented with missing teeth and the inability to properly chew his food (Figure 1 and Figure 2). He requested replacement of his missing teeth with dental implants, preferring a fixed option to avoid removables. The patient had a partially edentulous mandibular arch with non-restorable anterior teeth (Figure 3) and loss of vertical dimension of occlusion. After a thorough clinical evaluation, which included panorex radiographs, a treatment plan was developed that included extractions, immediate implant placement, and an implant-supported provisional denture in a single visit. The patient was a good candidate for immediate implant placement and restoration because of the remaining bone height and width, bone density, and a medical history with no signs of complications (Figure 4).
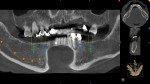
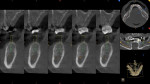
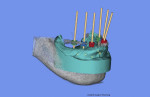
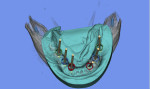
After the initial records were taken (ie, polyvinyl siloxane [PVS] impressions, facebow record, centric relation, and vertical dimension of occlusion), implant planning was completed to locate the implant sites at bilateral first molar sites, bilateral premolar sites, and bilateral canine sites to distribute the occlusal load (Figure 5 and Figure 6). CBCT (CS 9300, Carestream, www.carestream.com) was used during the implant placement planning process to locate and analyze bone density for immediate implant placement (Figure 7). CBCT planning included CAD/CAM analysis (Figure 8) and surgical guide (MGUIDE, MIS Implants Technologies Inc, www.mis-implants.com) fabrication (Figure 9 and Figure 10).
Once the implant locations were identified, diagnostic PVS impressions, models, and plans were sent to the laboratory (MCENTER, MIS Implants Technologies Inc) for fabrication of a surgical tissue-borne guide. The locations and angulations were finalized, and the guide was returned to the office prior to scheduling the surgery. Models were mounted on a semi-adjustable articulator (SAM3®, Great Lakes Orthodontics, www.greatlakesortho.com) for improved accuracy.
Placement Technique
After routine preparation, premedication was delivered and surgery was performed under local anesthesia (3% mepivacaine plain bilaterally, 2 carpules and 3% Marcaine with 100,000 epinephrine infiltration for mental foramen area bilaterally, 1 carpule). An aseptic technique was followed, and the surgical guide was verified in the mouth for perfect seating (Figure 11). Implant placement (MIS SEVEN implants, MIS Implants Technologies Inc) was performed using a flapless method with tissue punch by a precision tissue-incising drill in the posterior region. Posterior implants Nos. 19 and 30 were sequentially placed with support from the existing anterior and premolar teeth.
After placement of the posterior implants, the anterior teeth Nos. 22 through 27 were extracted, and implants were placed in the region of No. 22, Nos. 26 through 28. Final extraction of the premolars (Nos. 20 and 21) was performed, and the final implant was placed in the region of Nos. 20 and 21.
Primary stability was achieved in all implants with a torque value greater than 55 Ncm, except for the area of Nos. 22 through 27, which was 35 Ncm. Mineralized allograft cortical-cancellous bone grafts (Rocky Mountain Tissue Bank, www.rmtb.org) were used to graft the extraction and implant site areas, and final multi-unit abutments were placed. Temporary cylinders were used to immediately load the implants (Figure 12), and the screw-retained temporary hybrid denture was delivered (Figure 13). Proper implant placement was verified radiographically.
The patient required 4 months to heal, during which time the single zirconia fixed hybrid denture (Prettau® Zirconia, Zirkonzahn USA Inc, www.zirkonzahn.com) was fabricated in the laboratory. After 16 weeks, the final prosthesis was delivered, and postoperative panoramic radiographs and photographs were taken and the bite was adjusted (Figure 14 and Figure 15).
Conclusion
Using CBCT technology allows for accurate diagnosis of a patient’s preoperative condition, including bone height, width, and density. Unlike conventional radiographs, CBCT scans provide a 3D image of the anatomy, offering essential diagnostic and planning information when implants and restorations must be immediately placed. With CBCT scans and computer-generated surgical guides, clinicians can place implants more efficiently with high predictability, accuracy, and stability.
Disclosure
Datta Malyavantham, BDS, DDS, FICOI, has no relevant financial relationships to disclose.
References
1. Harris D, Buser D, Dula K, et al. E.A.O. guidelines for the use of diagnostic imaging in implant dentistry. A consensus workshop organized by the European Association for Osseointegration in Trinity College Dublin. Clin Oral Implants Res. 2002;13(5):566-570.
2. Garg AK, Vicari A. Radiographic modalities for diagnosis and treatment planning in implant dentistry. Implant Soc. 1995;5(5):7-11.
3. Batenburg RH, Stellingsma K, Raghoebar GM, Vissink A. Bone height measurements on panoramic radiographs: the effect of shape and position of edentulous mandibles. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(4):430-435.
4. Choi YG, Kim YK, Eckert SE, Shim CH. Cross-sectional study of the factors that influence radiographic magnification of implant diameter and length. Int J Oral Maxillofac Implants. 2004;19(4):594-596.
5. Zhang W, Skrypczak A, Weltman R. Anterior maxilla alveolar ridge dimension and morphology measurement by cone beam computerized tomography (CBCT) for immediate implant treatment planning. BMC Oral Health. 2015;15:65.
6. Tardieu PB, Vrielinck L, Escolano E, et al. Computer-assisted implant placement: scan template, simplant, surgiguide, and SAFE system. Int J Periodontics Restorative Dent. 2007;27(2):141-149.
7. Shotwell JL, Billy EJ, Wang HL, Oh TJ. Implant surgical guide fabrication for partially edentulous patients. J Prosthet Dent. 2005;93(3):294-297.
8. Mello LA, Garcia RR, Leles JL, et al. Impact of cone-beam computed tomography on implant planning and on prediction of implant size. Braz Oral Res. 2014;28(1):46-53.
9. Wöhrle PS. Predictably replacing maxillary incisors with implants using 3-D planning and guided implant surgery. Compend Contin Educ Dent. 2014;35(10):758-762, 764-766, 768.
10. De Oliveira RC, Leles CR, Normanha LM, et al. Assessments of trabecular bone density at implant sites on CT images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105(2):231-238.
11. Eufinger H, König S, Eufinger A, et al. Significance of height and width of the alveolar ridge in implantology in the edentulous maxilla. Analysis of 95 cadaver jaws and 24 consecutive patients. [In German] Mund Kiefer Gesichtschir. 1999;3 Suppl 1:S14-S18.
12. Roźe J, Babu S, Saffarzadeh A, et al. Correlating implant stability to bone structure. Clin Oral Implants Res. 2009;20(10):1140-1145.
13. Lin MH, Mau LP, Cochran DL, et al. Risk assessment of inferior alveolar nerve injury for immediate implant placement in the posterior mandible: a virtual implant placement study. J Dent. 2014;42 (3):263-270.
14. Salimov F, Tatli U, Kürkçü M, et al. Evaluation of relationship between preoperative bone density values derived from cone beam computed tomography and implant stability parameters: a clinical study. Clin Oral Implants Res. 2014;25(9):1016-1021.
15. Greenberg AM. Digital technologies for dental implant treatment planning and guided surgery. Oral Maxillofac Surg Clin North Am. 2015;27(2):319-340.
16. Klein M, Abrams M. Computer-guided surgery utilizing a computer-milled surgical template. Pract Proced Aesthet Dent. 2001;13(2):165-169; quiz 170.
17. Klein M, Cranin AN, Sirakian A. A computerized tomography (CT) scan appliance for optimal presurgical and preprosthetic planning of the implant patient. Pract Periodontics Aesthet Dent. 1993;5(6): 33-39; quiz 39.
About the Author
Datta Malyavantham, BDS, DDS, FICOI
Private Practice
Sterling, Virginia