Immediate Loading of Straumann® TLX Implant in Grafted Maxillary First Molar Site
Dean Morton, DDS, MS; Ahmet Orgev, BDS, MS; and Waldemar D. Polido, DDS, MS, PhD
ABSTRACT
The patient treatment described in this case report demonstrates management of a failing maxillary first molar utilizing an immediate loading approach. Following extraction, the site was successfully managed with socket grafting (ridge preservation) and allowed to heal prior to implant placement. A Straumann® TLX implant was placed using a guided approach and restored using CAD/CAM.
A 32-year-old female patient presented with a failing maxillary first molar. The tooth had been subjected to endodontic treatment and re-treatment, and several attempts had been made to restore the tooth with metal-ceramic crowns. A draining buccal fistula was noted (Figure 1 and Figure 2).
The patient was offered several treatment alternatives prior to the extraction of the tooth, inclusive of various implant placement and restoration protocols. She consented to having the tooth extracted and replaced with an implant-supported single-crown restoration. The extraction was planned for a minimum of trauma to the supporting bone and surrounding tissues. If the post-extraction situation proved to be favorable, immediate placement of a dental implant would be undertaken. Should the situation be considered compromised, the site would be grafted and allowed to heal prior to implant placement and loading.
Sectioning of the roots was required during the extraction, and the site was considered less than optimal for immediate implant placement. A socket grafting procedure, therefore, was completed utilizing demineralized bovine bone mineral with 10% collagen (DBBM+C) (Figure 3) sealed with a collagen matrix.
The graft was afforded 6 months of undisturbed healing. Clinically, at that point the ridge was broad, and the surrounding soft tissues appeared healthy and attached (Figure 4). There was no evidence of the fistula.
Treatment Planning
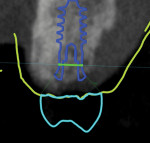
A digital volume or cone-beam computed tomography was acquired (digital imaging and communications in medicine [DICOM]) along with intraoral scans of the patient's remaining dentition (STL files) and virtual interocclusal records (Virtuo Vivo™, Straumann, straumann.com). The DICOM and STL files were imported into planning software (coDiagnostiX®, Straumann), and the datasets were registered and merged. A virtual diagnostic design was developed using CARES® Visual software (Straumann). Using Synergy™ interface, the treatment team was able to determine the appropriate 3-dimensional (3D) restoration-driven implant position (Figure 5 and Figure 6).
The planned implant position was confirmed and accepted by the treatment team. A surgical template was designed using coDiagnostiX software (Figure 7). This template was to be used as a static guide (s-CAITS) to facilitate restoration-driven 3D positioning of the chosen implant (Straumann® TLX RT Ø 4.5 mm x 8 mm, Straumann). The surgical template design incorporated a channel to facilitate irrigation during implant placement. Once the template design was approved, it was exported for manufacture using a digital workflow.
The surgical template was positioned clinically and the fit was verified using direct visualization and observation windows incorporated into the template design (Figure 8). The procedure was performed under local anesthesia. To facilitate surgical positioning of the implant (Figure 9) a mid-crestal full-thickness incision was made along with sulcular releasing incisions. No vertical releasing incisions were made. The crestal tissues on either side of the incision were reflected and the osteotomy prepared. The final twist drill size (3.7 mm) was limited to enhance primary stability of the implant. A profile drill was also used to ensure 1 mm subcrestal positioning of the polished collar of the implant. Adequate primary stability for immediate loading of the implant was achieved with an insertion torque of 50 Ncm and an implant stability quotient (ISQ) measurement of 78.
The Straumann TLX implant was chosen to maximize primary stability of the implant in the grafted bone in order to facilitate immediate loading. After placement of the implant the soft tissues were repositioned and sutured into place (Figure 10).
Before the implant was placed a provisional crown was designed and prefabricated using a digital workflow (CARES Visual). The provisional crown was milled in polymethyl methacrylate (PMMA) (Vita CAD-Temp® monoColor, VITA, vitanorthamerica.com) using a milling unit (Straumann® M Series, Straumann).
Following implant placement and confirmation of primary stability, a provisional abutment for a crown was positioned into the implant and torqued to 15 Ncm. The prefabricated provisional restoration was oriented over the provisional abutment using the proximal and occlusal contacts (Figure 11). Autopolymerizing resin was used to lute the prefabricated shell to the abutment. The provisional restoration was then finished and polished, torqued to 20 Ncm, and sealed (Figure 12). The provisional restoration was adjusted to ensure no occlusal contacts were evident in maximum intercuspation (Figure 13) or during any excursive movements. The position of the implant was confirmed with a post-placement periapical radiograph (Figure 14).
Healing was evaluated 2 weeks after implant placement and was considered to be excellent. The patient reported no postoperative concerns, and all tissues were healthy. The provisional restoration was well-tolerated, and no implant or restoration loosening was noted (Figure 15).
Definitive Zirconia Crown
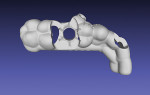
The patient was re-evaluated after an additional 3 weeks of healing (5 weeks total). The peri-implant soft tissues were in excellent health and the patient reported no concerns. The provisional restoration was removed and the soft tissue evaluated (Figure 16). A scanbody (CARES® Mono Scanbody, Straumann) was positioned and a final digital impression was captured with an intraoral scanner (Virtuo Vivo). The intraoral scans and virtual articulation records were imported in a CAD/CAM software program (CARES Visual), which was used to design the definitive zirconia crown. The definitive crown was designed for luting to a titanium abutment (Variobase® for Crown, Straumann) prior to delivery (Figure 17), enabling screw retention of the definitive prosthesis at the level of the implant.
The patient presented for definitive crown delivery 7 weeks post implant placement. She reported no concerns with the provisional restoration or the surrounding tissues, and she had favorably received the immediate loading of the implant with the provisional. The provisional restoration was removed and the peri-implant tissues were evaluated and considered healthy (Figure 18). After the patient confirmed esthetic acceptance of the definitive prosthesis, and occlusal adjustment and finishing was done, the definitive crown was secured to the implant to 35 Ncm. Polytetrafluoroethylene tape and light-polymerizing composite resin were used to seal the screw access (Figure 19). The definitive crown was confirmed as having light occlusal contact with the opposing dentition in maximum intercuspation (Figure 20) and was free of contact in excursive movements. A periapical radiograph was obtained to establish baseline bone levels and confirm adaptation of all components (Figure 21).
Outcome and Conclusion
An immediate loading approach was used for this clinical treatment. The implant was positioned according to a conventional protocol as a result of the need for grafting. A digital workflow was utilized throughout all phases of treatment; this included digital data recording, digital planning, computer-guided surgery, and CAD/CAM design and fabrication of the provisional and definitive restorations. The Straumann TLX implant system allows clinicians to combine the benefits of improved thread design, such as primary stability and biocompatibility, with proven tissue-level implant characteristics (eg, emergence profile, proven restorative platform, and peri-implant tissue health and predictability).
Disclosure
This article was commercially supported by Straumann.
About the Authors
Dean Morton,DDS, MS, FACP
Indiana Dental Association Endowed Professor, Department of Prosthodontics, Indiana University School of Dentistry (IUSD), Indianapolis, Indiana; Director of the Center for Implant, Esthetic and Innovative Dentistry at IUSD; Private Practice limited to Prosthodontics and Implant Dentistry at IUSD
Ahmet Orgev, BDS, MS
Resident in Prosthodontics, Indiana University School of Dentistry, Indianapolis, Indiana
Waldemar D. Polido, DDS, MS, PhD
Oral and Maxillofacial Surgeon; Professor and Acting Chairman of Oral and Maxillofacial Surgery, Indiana University School of Dentistry (IUSD), Indianapolis, Indiana; Co-Director of the Center for Implant, Esthetic and Innovative Dentistry at IUSD