Characterization of the Double Bond Conversion of Acrylic Resins for 3D Printing of Dental Prostheses
Frank Alifui-Segbaya, BSc (Hons), MPhil, PhD; Jasper Bowman, BSc; Alan R. White, BSc; Roy George, BDS, MDS, PhD; and Ismail Fidan, BSc, MSc, PhD
Abstract
Characterization of the double bond conversion of acrylic resins is considered critical in the evaluation of dental materials due to the propensity of end-use devices to accumulate residual monomer and degradation products that can cause local and systemic side effects in high doses. In this study, the authors examine two different acrylic-based photopolymers indicated for 3D printing of dental prostheses using Fourier transform infrared spectroscopy: a denture base material comprising ≥75% ethoxylated bisphenol A dimethacrylate, and a crown-and-bridge material composed of >60% proprietary methacrylic oligomer and 15%–25% 2-hydroxyethyl methacrylate. Infrared spectroscopy data showed a conversion rate (240 s) of 52.37 ± 1.05% for the former material and 45.36 ± 1.41% for the latter. Compared to traditional acrylic resins, both materials exhibited a considerably lower degree of conversion. With limited scientific data available on the clinical performance of 3D printing materials in general, additional evidence is needed to ascertain their in vivo performance in the long-term.
Photopolymerization, or light-induced polymerization, of solvent-free resins offers economy and a myriad of practicalities in dentistry, where various devices for prosthodontic treatments are constructed with acrylic resins. For enhanced clinical outcomes, the resins should display high curing rate, good storage stability, low viscosity, low toxicity, and acceptable physico-mechanical properties after polymerization.1,2 Since polymerization does not guarantee a 100% monomer conversion rate,3 there is a tendency for dental devices to accumulate residual monomer and degradation products that can cause local and systemic side effects in high doses.4-6 To put this in context, structurally deficient acrylic-based devices can cause cytotoxic effects on pulp and oral mucosa and inhibit protein synthesis of oral epithelial cells.7
In this study, double bond conversion (DBC), considered an essential clinical property that may influence the physical and mechanical properties of dental resins and composites during polymerization, is measured. DBC describes the percentage of carbon-carbon double bonds (-C=C-) that is converted to single bonds (-C-C-) or the extent to which all of the monomer is converted to polymer.8-10 In essence, a higher conversion of double bonds may produce superior mechanical strength; the unreacted double bonds (monomer), on the other hand, may be present either in free monomer or as pendant groups on the polymer network, which may leach and irritate the soft tissue.11 Because very little data is published on 3D printing of dental resins, the current study will examine Class IIa materials for denture bases and crowns and bridges.
Materials and Methods
Liquid photopolymer resins for this study were manufactured by Vertex Dental (vertex-dental.com) and supplied by NextDent-3D Systems (nextdent.com) (Table 1). During experimentation, test specimens were prepared by compressing uncured resins between sodium chloride crystals (Supelco®, Merck KGaA, emdgroup.com) and irradiated (440-nm to 480-nm wavelength range and 1200 mW/cm2 light intensity) at 5-mm fixed distance using a LED curing light (Radii-cal, SDI Limited, sdi.com.au).
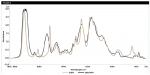
The degree of conversion was calculated from the decrease in infrared absorbance (A) after a given exposure using the formula: 1- At /A0 x 100,12 where "A0" is the peak absorbance at 1637 cm-1 at null time (initial intensity when time, "t," is zero); and "At" is the absorbance when "t" was 10 s, 20 s, 40 s, 60 s, 80 s, 120 s, 180 s, and 240 s during irradiation.11 Variable absorbance of aliphatic double bond (peak at 1637 cm-1) was used in relation to constant absorbance (internal standard)7: 1608 cm-1 for the first material, Denture 3D+ (D3D+), and 778 cm-1 for the second material, C&B Micro Filled Hybrid (C&B MFH). Experiments were performed on resin samples (n = 3) in triplicates using a FT-IR spectrometer (Spectrum Two™ FT-IR, PerkinElmer, Inc., perkinelmer.com) at 4 cm-1 spectral resolution, four scans, and 4000-450 cm-1 range.
Results
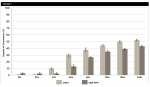
Infrared spectroscopy data for the two photopolymers are presented in graphical form in Figure 1. Figure 2 and Figure 3 show absorbance spectra obtained at null time and 240 s after irradiation, respectively. Absorbance spectra at null time also indicate the compositional variations of the two materials.
Discussion
With 3D printing gaining in popularity,13 the variety of dental materials being developed is increasing,14 and these materials are likely to differ in polymerization rate, vinyl group conversion, network structure,15 and biocompatibility.16-22 By adopting the thin film transmission method,23 the authors measured the decrease in intensity of the methacrylate C=C stretching mode absorption at 1637 cm-1, as monomer is converted to polymer. For both materials tested, degree of conversion (%) increased with time. Although D3D+ recorded a higher conversion rate, it was relatively low compared with traditional acrylic resins.24 Being a dimethacrylate, D3D+ exhibited high unsaturated monomers, which possiblywas due to limited movement of the monomers during onset vitrification of the polymer and the inability of unreacted methacrylate groups to diffuse through the matrix when attached to the polymer.7
In photopolymerization-based 3D printing, several manufacturing parameters are able to influence the clinical outcome of dental devices.16,20 Consequently, the quality of the devices may vary significantly regardless of whether they were manufactured using different 3D printers or with the same 3D printer and a standardized workflow of parameters, process steps, and materials.25 Currently, it remains a matter of discussion whether the amount of eluted substances from polymerized resins correlates with conversion rate.26 For 3D printing materials, experimental data to date imply that limited correlation exists between a material's conversion rate and biological performance.21 As such, caution must be particularly exercised when new and proprietary formulations are used that are likely to exhibit varying chemical structure, functionality, and concentration of the various constituents in the additive processes. It should be noted that factors such as resin composition, specimen geometry, photoinitiator concentration, irradiation intensity and duration, curing temperature, exposure to oxygen, and curing methods all interact to control the extent of polymerization.10 In 3D printing, resins with relatively low viscosity are likely to produce rapid polymerization yielding cross-linked polymers with properties suited to the demands imposed by the target application.2 To ensure this, some printers have a built-in heating mechanism for approved materials.27 It is important that this aspect of the manufacturing process is not overlooked.
With limited scientific data available on the clinical performance of 3D printing materials, additional evidence is needed to ascertain their in vivo performance in the long-term.
About the Authors
Frank Alifui-Segbaya, BSc (Hons), MPhil, PhD
Lecturer, School of Dentistry and Oral Health, Griffith Health, Gold Coast Campus, Griffith University, Queensland, Australia
Jasper Bowman, BSc
Technical Officer, School of Environment and Science, Griffith Sciences, Nathan Campus, Griffith University, Queensland, Australia
Alan R. White, BSc
Senior Scientific Officer, School of Environment and Science, Griffith Sciences, Nathan Campus, Griffith University, Queensland, Australia
Roy George, BDS, MDS, PhD
Associate Professor, School of Dentistry and Oral Health, Griffith Health, Griffith University, Queensland, Australia
Ismail Fidan, BSc, MSc, PhD
Professor, Tennessee Tech University, Cookeville, Tennessee
References
1. Li J, Cui Y, Qin K, et al. Synthesis and properties of a low-viscosity UV-curable oligomer for three-dimensional printing. Polymer Bulletin. 2016;73(2):571-585.
2. Vitale A, Cabral JT. Frontal conversion and uniformity in 3D printing by photopolymerisation. Materials (Basel). 2016;9(9):760.
3. Duray SJ, Gilbert JL, Lautenschlager EP. Comparison of chemical analysis of residual monomer in a chemical-cured dental acrylic material to an FTIR method. Dent Materials. 1997;13(4):240-245.
4. Mir GN, Lawrence WH, Autian J. Toxicological and pharmacological actions of methacrylate monomers. 3. Effects on respiratory and cardiovascular functions of anesthetized dogs. J Pharm Sci. 1974;63(3):376-381.
5. Mir GN, Lawrence WH, Autian J. Toxicological and pharmacological actions of methacrylate monomers. I. Effects on isolated, perfused rabbit heart. J Pharm Sci. 1973;62(5):778-782.
6. Mir GN, Lawrence WH, Autian J. Toxicological and pharmacological actions of methacrylate monomers. II. Effects on isolated guinea pig ileum. J Pharm Sci. 1973;62(8):1258-1261.
7. Kim S-H, Watts DC. Degree of conversion of bis-acrylic based provisional crown and fixed partial denture materials. The Journal of Korean Academy of Prosthodontics. 2008;46(6):639-643.
8. Anusavice K, Shen FC, Rawls HR. Phillips' Science of Dental Materials. 12th ed. St. Louis, MO: Elsevier Saunders; 2013.
9. Powers JM, Wataha JC. Dental Materials: Foundations and Applications. Philadelphia, PA: Elsevier Health Sciences; 2017.
10. Stansbury JW, Dickens SH. Determination of double bond conversion in dental resins by near infrared spectroscopy. Dent Mater. 2001;17(1):71-79.
11. Sideridou I, Tserki V, Papanastasiou G. Effect of chemical structure on degree of conversion in light-cured dimethacrylate-based dental resins. Biomaterials. 2002;23(8):1819-1829.
12. Decker C. Kinetic study and new applications of UV radiation curing. Macromolecular Rapid Communications. 2002;23(18):1067-1093.
13. Fidan I, Imeri A, Gupta A, et al. The trends and challenges of fiber reinforced additive manufacturing. International Journal of Advanced Manufacturing Technology. 2019;102(5-8):1801-1818.
14. The Market Reports. Global Dental 3D Printing Market Research Report 2021: QY Research. https://www.themarketreports.com/report/global-dental-3d-printing-market-research-report-2021. Updated August 2016. Accessed October 28, 2019.
15. Yu Q, Nauman S, Santerre JP, et al. Photopolymerization behavior of di(meth)acrylate oligomers. 2001;36(15):3599-3605.
16. Alifui-Segbaya F, Varma S, Lieschke GJ, George R. Biocompatibility of photopolymers in 3D printing. 3d Print Addit Manuf. 2017;4(4):185-191.
17. Oskui SM, Diamante G, Liao C, et al. Assessing and Rreducing the toxicity of 3D-printed parts. Environmental Science & Technology Letters. 2016;3(1):1-6.
18. MacDonald NP, Zhu F, Hall CJ, et al. Assessment of biocompatibility of 3D printed photopolymers using zebrafish embryo toxicity assays. Lab Chip. 2016;16(2):291-297.
19. Carve M, Wlodkowic D. 3D-printed chips: compatibility of additive manufacturing photopolymeric substrata with biological applications. Micromachines (Basel). 2018;9(2):91.
20. Alifui-Segbaya F, George R. Biocompatibility of 3D-printed methacrylate for hearing devices. Inventions. 2018;3(3):52.
21. Alifui-Segbaya F, Bowman J, White AR, et al. Toxicological assessment of additively manufactured methacrylates for medical devices in dentistry. Acta Biomaterialia. 2018;78(15):64-77.
22. Alifui-Segbaya F. Toxicological assessment of photopolymers in additive manufacturing using the innovative zebrafish embryo model. [PhD Doctorate]. Brisbane: Griffith University; 2018.
23. Ruyter IE, Gyorosi PP. An infrared spectroscopic study of sealants. Scandinavian Journal of Dental Research. 1976;84(6):396-400.
24. Urban VM, Machado AL, Vergani CE, et al. Degree of conversion and molecular weight of one denture base and three reline resins submitted to post-polymerization treatments. Mat Res. 2007;10(2):191-197.
25. Food and Drug Administration. Technical considerations for additive manufactured devices: draft guidance for industry and food and drug administration staff. 2016:1-28.
26. Schmalz G, Galler KM. Biocompatibility of biomaterials-lessons learned and considerations for the design of novel materials. Dent Mater. 2017;33(4):382-393.
27. Formlabs. Expanding 3D Printing Technologies to High-Volume Applications and Beyond. Mary Ann Liebert, Inc. publishers. https://www.nxtbook.com/nxtbooks/mal/formlabsebook201709/index.php.