Ridge Augmentation Simultaneous With Immediate Implant Placement: The Subperiosteal Tunneling Technique
Barry P. Levin, DMD
Abstract
The efficacy of immediate implant placement has made it an appealing treatment modality in dentistry. Over the past several decades various surgical techniques to minimize the ridge collapse and other adverse changes that occur after tooth extraction have been advocated. This case series proposes a method of soft-tissue augmentation when multiple implants are being immediately placed. The authors describe a subperiosteal tunneling technique that achieves the dual purpose of graft containment/guided bone regeneration and soft-tissue augmentation around maxillary anterior implants.
Immediate implant placement is becoming increasingly common in current implant practice. The expediency and efficiency this treatment modality offers makes it attractive to both patients and clinicians. The early belief or philosophy that placement of an implant into a fresh extraction socket would preserve dentoalveolar contours1,2 has been disproven,3-5 as implants do not alter the wound healing process in the extraction socket after tooth removal. More currently, many authors have advocated various surgical techniques to minimize the ridge collapse and negative changes that occur after extraction. These techniques include implant placement without reflection of mucoperiosteal flaps6,7 and with the use of bone augmentation,8,9soft-tissue grafting,10 guided bone regeneration (GBR), or various combinations of these procedures.11,12
When anterior single-tooth implants are placed, it is not uncommon for surgeons to use autogenous connective tissue grafts for soft-tissue augmentation. The size of these grafts is relatively small and the morbidity associated with their procurement is mild to moderate in most cases, though Chung et al reported on the possibility of graft failure.13 When multiple immediate implants are placed, the relative size of these grafts can be significant, and the surgical time and morbidity are typically increased. Alternatives to this approach often include the use of allogeneic dermal grafts. A drawback to these materials, however, is their inert, avascular composition.14 Though these grafts are capable of being incorporated into native tissues,15 time is required for adequate revascularization; the exact amount of time needed for incorporation to occur is speculative, though clinically this usually takes place over several weeks. Therefore, these grafts must be covered with the overlying soft tissues to prevent premature exposure and consequent sloughing of the graft.
In flapless immediate implant placement, soft tissues cannot be coronally advanced significantly, and, therefore, a resultant void usually exists between the implant and hard/soft-tissue socket walls.16 This void can be obturated with particulate bone graft materials, collagen membranes, and/or soft-tissue grafts. It may also be "sealed" with provisional restorations17,18 or anatomically shaped healing abutments.19 The size of the gap is also important.20 It has been demonstrated that sites with larger gaps, ie, greater than 1 mm, result in significantly greater osseous regeneration.21 Recently, a technique to augment peri-implant soft tissues at the time of immediate implant placement and temporization was introduced for single-tooth replacement.22 When multiple implants are being placed, another method of soft-tissue augmentation is proposed, as discussed herein.
This case series describes a subperiosteal tunneling technique for the dual purpose of graft containment/GBR and soft-tissue augmentation around multiple maxillary anterior implants.
Clinical Technique
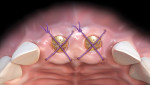
This procedure, illustrated in Figure 1 through Figure 5, is indicated for flapless immediate implant placement in maxillary anterior sites where implants are placed to the palatal aspect of the extraction sockets. Implant diameter is deliberately selected to preserve a "gap" between the inner aspect of the buccal wall of the socket and implant surface. The gap is obturated with a composite bone graft material consisting of mineralized freeze-dried bone allograft (FDBA) and deproteinized bovine bone mineral (DBBM) in a ratio of 4:1. Implants are sealed with appropriately sized stock healing abutments.
Subsequent to bone grafting, a subperiosteal dissection of the facial, palatal, and proximal soft tissues is performed. This is accomplished with periodontal knives and small periosteal elevators. Great care is necessary to avoid soft-tissue dehiscence and perforation. The procedure requires serial and circumferential elevation moving the elevator mesial-distally as well as coronal-apically beneath the papillae. Singular focus in one area can lead to unwanted soft-tissue tearing; patience is needed to widen the zone of subperiosteal elevation, slowly and gradually moving the reflection.
Once a zone of at least 4 mm to 5 mm of facial and palatal elevation is confirmed, the dermal allograft is trimmed to match the subperiosteal zone created by elevation. A soft-tissue punch is used to perforate the dermal graft according to the position of the healing abutments. It is critical to orient the dermal allograft in a manner in which the connective tissue surface is facing "up" to be in direct contact with the periosteum of the overlying soft tissues. This is done to facilitate and ensure integration of the graft within the soft tissues.
A monofilament, resorbable suture is passed through the distofacial aspect of the mucosa relative to one of the terminal implants. It is "tucked" under the detached papilla or papillae to engage the dermal allograft in both facial and palatal positions and passed back through the initial path. A C-3 needle is then passed through the distal-palatal mucosa. With careful manipulation, the graft is advanced via the suture under the papillae and adapted between the facial and palatal bone and periosteum, and the initial suture is tied on the palatal aspect of the ridge. Additional sutures are used to secure the allograft to the soft tissues facially and palatally. "Figure 8" design sutures are used to compress the detached soft tissue to minimize clots between the periosteum and dermal allograft and dermal allograft and coronal/proximal bone.
Case Reports
Case 1
Clinical case No. 1 involves an 89-year-old female patient with a history of implant therapy. She presented with mobile crowns on teeth Nos. 9 and 10, which were placed only 1 year prior (Figure 6). Both teeth had a history of endodontic and restorative therapy and demonstrated significant recurrent caries.
After extractions were done without flap elevation, the sockets were debrided with ultrasonic (Piezotome, Acteon, acteongroup.com) and manual instrumentation. Implants were intentionally placed toward the palatal aspect of the extraction sockets with primary stability, confirmed with an insertion torque exceeding 25 Ncm (Figure 7).23 The gaps between the implants and inner walls of the extraction sockets were obturated with a composite particulate bone graft composed of FDBA/DBBM in a 4:1 ratio. The dermal allograft (PerioDerm™, Dentsply Sirona, dentsplysirona.com), with a thickness of 0.4 mm to 0.8 mm, was trimmed as described earlier and pierced with tissue punches to correspond with the positions of the healing abutments. It was then placed beneath the periosteal aspect of the elevated soft tissues. Extreme care was taken to avoid detachment of the interproximal papillae. Monofilament sutures (Monocryl® 5-0, Ethicon, ethicon.com) were used to secure the allograft and gently compress the overlying soft tissues (Figure 8).
After 8 weeks of healing, the site appeared healthy with preservation of the alveolar ridge in three dimensions (Figure 9). The patient was referred to the restorative dentist to begin esthetic treatment at approximately 10 weeks after surgery. Both implants were restored with custom CAD/CAM abutments and cement-retained single crowns (Figure 10).
Case 2
The second case demonstrates a 76-year-old female patient with a failing three-unit fixed dental prosthesis (FDP) from teeth Nos. 7 through 9 (Figure 11). After flapless extraction, immediate implant placement toward the palatal aspect of the sockets was performed. Healing abutments were placed, and the void between the implant surface and socket walls was filled with the same particulate bone graft as in the previous clinical situation (Figure 12). The overlying soft tissues, including the pontic space of tooth No. 8, was reflected and the same dermal allograft was carried via suture through the field and secured as previously described. This was meant to augment the coronal and buccal aspect of the future ovate pontic site, as well as the peri-implant mucosa (Figure 13).
After 5 weeks, the site appeared healthy, and facial contours were improved compared to the presurgical situation. The concavity in the edentulous site of No. 8 was convex and peri-implant bone levels were unchanged. After another 4 weeks, radiographic bone levels remained unchanged (Figure 14 and Figure 15). The healing abutment on the implant in the No. 9 position was changed to a taller (4 mm height versus 3.5 mm height) but narrower (4 mm diameter versus 5 mm diameter) abutment to facilitate easier restorative therapy and encourage coronal migration of soft tissue prior to provisional restoration (Figure 16). The final cement-retained FPD from Nos. 7 through 9 is shown in Figure 17.
Case 3
The third and final case involves treatment of a 60-year-old male patient, whose restorative dentist had deemed teeth Nos. 7 and 8 unrestorable (Figure 18). Both teeth were extracted without flap reflection and implants were placed palatally with primary stability confirmed by resonance frequency analysis (Osstell Mentor, Osstell, osstell.com). Bone grafting was performed as previously described.
Prior to subperiosteal tunneling, an open-tray impression was taken, which facilitated indirect fabrication of splinted screw-retained temporary restorations that would be delivered the same day as surgery. Healing abutments were placed and tunneling as described earlier was performed. Again, caution was used to avoid separation or detachment of the interproximal papillae. A thin (0.4 mm to 0.8 mm) dermal allograft was advanced through the subperiosteal space and secured with 5-0 monofilament sutures. The patient presented immediately to the restorative dentist for delivery of the splinted screw-retained restorations (Figure 19). Care was taken to prevent any occlusal contact with these restorations, and the patient was advised to avoid mastication on the surgical site for about 6 weeks.
After approximately 12 weeks of healing, definitive restorative therapy was performed, comprising custom abutment fabrication and two individual cement-retained crowns (Figure 20).
Discussion
When treating hopeless teeth in the maxillary anterior sextant, clinicians face unique challenges. Both hard and soft tissues are relatively thin.24 These tissues are susceptible to atrophy after tooth extraction. When immediate implants are placed in the esthetic zone, the naturally occurring diminutive changes of the alveolar ridge can compromise esthetic outcomes.25 Investigators have proposed augmenting soft tissues at the time of implant placement.26,27
The subperiosteal tunneling technique is designed to accomplish several goals. First, it eliminates the need to procure relatively large, autogenous connective tissue grafts. This reduces treatment time and surgical morbidity. Second, it allows peri-implant soft tissues to be augmented while they also function as a collagen barrier (ie, GBR). Because the allograft is passed under the interproximal papillae, it has the potential to increase soft-tissue volume between adjacent implants and/or implants and pontics in the esthetic zone.
In the maxillary anterior sextant, where hard and soft tissues are naturally thin, it is difficult or impossible to reflect partial-thickness mucosal tissues. It has been speculated that the retention of minimal connective tissue coverage may be of little benefit compared to subperiosteal reflection, which is easier to perform, in terms of limiting bone resorption.28 Because the soft-tissue elevation is subperiosteal in nature, some of the benefits of a flapless procedure are compromised, however. Therefore, the zone of elevation is minimized to approximately 4 mm to 5 mm beyond the crestal osseous margins of the extraction sockets.
A similar approach for mucogingival corrective surgery has been documented.29 In that technique, a subperiosteal elevation is combined with insertion of a dermal allograft between the alveolar bone and periosteum, and the soft tissues are coronally advanced to achieve root coverage secondary to gingival recession. Also, because the proximal tissues are not incised, blood supply from the facial and palatal aspects of the mucosa is not severed. Pressure to minimize the size of the postoperative blood clots and use of compression sutures encourage rapid healing and prevent soft-tissue necrosis and hematoma formation.
Increasing the thickness of peri-implant mucosa is a topic of great interest. Linkevicius et al demonstrated the benefit of augmenting naturally occurring thin mucosa, in terms of crestal bone preservation.30,31 These authors have exhaustively researched the role of tissue thickness as it relates to crestal bone levels in edentulous sites. Any extrapolation of their findings as they relate to immediate implant placement must be done with caution.
The present author (BPL) has published a case series utilizing the same dermal allograft in an open or flapped immediate implant placement scenario.32 The dermis is used as both a GBR membrane and tissue-thickening agent. Because the procedure is demonstrated in a case series and not a controlled clinical trial, more research is required to confirm its efficacy.
Conclusion
The present case series described a subperiosteal tunneling technique for the dual purpose of graft containment/GBR and soft-tissue augmentation around multiple maxillary anterior implants. The procedure, featuring flapless immediate implant placement where implants are placed to the palatal aspect of the extraction sockets, was shown to achieve alveolar ridge preservation and improved facial contours while enabling esthetic restoration in a timely fashion. The tunneling procedure is also intended to augment soft tissue volume in proximal and pontic regions; however, controlled studies are necessary to confirm this clinical finding.
About the Author
Barry P. Levin, DMD
Clinical Associate Professor, University of Pennsylvania, Philadelphia,
Pennsylvania; Diplomate, American Board of Periodontology; Private Practice, Jenkintown, Pennsylvania
References
1. Werbitt MJ, Goldberg PV. The immediate implant: bone preservation and bone regeneration. Int J Periodontics Restorative Dent. 1992;12(3):
206-217.
2. Denissen HW, Kalk W, Veldhuis HA, van Waas MA. Anatomic consideration for preventive implantation. Int J Oral Maxillofac Implants. 1993;8
(2):191-196.
3. Araújo MG, Lindhe J. Ridge alterations following tooth extraction with and without flap elevation: an experimental study in the dog. Clin Oral Implants Res. 2009;20(6):545-549.
4. Araújo MG, Wennström JL, Lindhe J. Modeling of the buccal and lingual bone walls of fresh extraction sites following implant installation. Clin Oral Implants Res. 2006;17(6):606-614.
5. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004;31(10):820-828.
6. Chen ST, Darby IB, Reynolds EC, Clement JG. Immediate implant placement postextraction without flap elevation. J Periodontol. 2009;
80(1):163-172.
7. Lazic Z, Golubovic M, Markovic A, et al. Immunohistochemical analysis of blood vessels in peri-implant mucosa: a comparison between mini-incision flapless and flap surgeries in domestic pigs. Clin Oral Implants Res. 2015;26(7):775-779.
8. Sanz M, Lindhe J, Alcaraz J, et al. The effect of placing a bone replacement graft in the gap at immediately placed implants: a randomized clinical trial. Clin Oral Implants Res. 2017;28(8):902-910.
9. Tarnow DP, Chu SJ, Salama MA, et al. Flapless postextraction socket implant placement in the esthetic zone: Part 1. The effect of bone grafting and/or provisional restoration of facial-palatal ridge dimensional change-a retrospective cohort study. Int J Periodontics Restorative Dent. 2014;34(3):323-331.
10. Grunder U. Crestal ridge width changes when placing implants at the time of tooth extraction with and without soft tissue augmentation after a healing period of 6 months: report of 24 consecutive cases. Int J Periodontics Restorative Dent. 2011;31(1):9-17.
11. Cardaropoli D, Gaveglio L, Gherlone E, Cardaropoli G. Soft tissue contour changes at immediate implants: a randomized controlled clinical study. Int J Periodontics Restorative Dent. 2014;34(5):631-637.
12. Caneva M, Botticelli D, Morelli F, et al. Alveolar process preservation at implants installed immediately into extraction sockets using deproteinized bovine bone mineral-an experimental study in dogs. Clin Oral Implants Res. 2102;23(7):789-796.
13. Chung S, Rungcharassaeng K, Kan JY, et al. Immediate single tooth replacement with subepithelial connective tissue graft using platform switching implants: a case series. J Oral Implantol. 2011;37(5):559-569.
14. Potter MJ, Linge C, Cussons P, et al. An investigation to optimize angiogenesis within potential dermal replacements. Plast Reconstr Surg. 2006;117(6):1876-1885.
15. Cohen M, Joester D, Geiger B, Addadi L. Spatial and temporal sequence of events in cell adhesion: from molecular recognition to focal adhesion assembly. Chembiochem. 2004;5(10):1393-1399.
16. Botticelli D, Persson LG, Lindhe J, Berglundh T. Bone tissue formation adjacent to implants placed in fresh extraction sockets. an experimental study in dogs. Clin Oral Implants Res. 2006;17(4):351-358.
17. Degidi M, Daprile G, Nardi D, Piattelli A. Immediate provisionalization of implants placed in fresh extraction sockets using a definitive abutment: the chamber concept. Int J Periodontics Restorative Dent. 2013;33(5):559-565.
18. Chu SJ, Salama MA, Garber DA, et al. Flapless postextraction socket implant placement, Part 2: the effects of bone grafting and provisional restoration on peri-implant soft tissue height and thickness-a retrospective study. Int J Periodontics Restorative Dent. 2015;35(6):803-809.
19. Becker W, Doerr J, Becker BE. A novel method for creating an optimal emergence profile adjacent to dental implants. J Esthet Restor Dent. 2012;24(6):395-400.
20. Ferrus J, Cecchinato D, Pjetursson EB, et al. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Implants Res. 2010;21(1):22-29.
21. Le BT, Borzabadi-Farahani A. Labial bone thickness in area of anterior maxillary implants associated with crestal labial soft tissue thickness. Implant Dent. 2012:21(5):406-410.
22. Levin BP. The dermal apron technique for immediate implant socket management: a novel technique. J Esthet Restor Dent. 2016;28(1):18-28.
23. Norton MR. The influence of insertion torque on the survival of immediately placed and restored single-tooth implants. Int J Oral Maxillofac Implants. 2011;26(6):1333-1343.
24. Younes F, Eghbali A, Raes M, et al. Relationship between buccal bone and gingival thickness revisited using non-invasive registration methods. Clin Oral Implants Res. 2016;27(5):523-528.
25. Kan JY, Rungcharassaeng K, Lozada JL, Zimmerman G. Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants: a 2- to 8-year follow-up. Int J Oral Maxillofac Implants. 2011;26(1):179-187.
26. Yoshino S, Kan JY, Rungcharassaeng K, et al. Effects of connective tissue grafting on the facial gingival level following single immediate implant placement and provisionalization in the esthetic zone: a 1-year randomized controlled prospective study. Int J Oral Maxillofac Implants. 2014;29(2):432-440.
27. Migliorati M, Amorini L, Signori A, et al. Clinical and aesthetic outcome with post-extractive implants with or without soft tissue augmentation: a 2-year randomized clinical trial. Clin Implant Dent Relat Res. 2015;17(5):983-995.
28. Wood DL, Hoag PM, Donnenfeld OW, Rosenfeld LD. Alveolar crest reduction following full and partial thickness flaps. J Periodontol. 1972;
43(3):141-144.
29. Allen EP. Subpapillary continuous sling suturing method for soft tissue grafting with the tunneling technique. Int J Periodontics Restorative Dent. 2010;30(5):479-485.
30. Linkevicius T, Puisys A, Linkeviciene L, et al. Crestal bone stability around implants with horizontally matching connection after soft tissue thickening: a prospective clinical trial. Clin Implant Dent Relat Res. 2015;17(3):497-508.
31. Linkevicius T, Puisys A, Steigmann M, et al. Influence of vertical soft tissue thickness on crestal bone changes around implants with platform switching: a comparative clinical study. Clin Implant Dent Relat Res. 2015;17(6):1228-1236.
32. Levin BP. The dual function of a dermal allograft in immediate implant therapy. Int J Periodontics Restorative Dent. 2015;35(4):507-513.