Use of Narrow-Diameter Implants in Treatment of Severely Atrophic Maxillary Anterior Region With Implant-Supported Fixed Restorations
Stuart J. Froum, DDS; Sang-Choon Cho, DDS; Salvatore Florio, DDS; and Craig M. Misch, DDS, MDS
Abstract: The edentulous anterior atrophic maxilla represents a challenge for the surgeon and restorative dentist. Soft- and hard-tissue augmentation procedures are often required prior to, or simultaneously with, implant placement. A well-planned treatment protocol, patient compliance, and collaboration between the treating clinicians and the laboratory are requirements in achieving predictable long-term outcomes that satisfy patient expectations. Avoiding transmucosal loading and movement of the graft during the healing phase are crucial factors in achieving lasting success. In this case report, a fixed provisional restoration supported by four immediately loaded narrow-diameter implants (NDIs) was used to enable function during healing and protect the grafted site. Two of the NDIs, along with three conventional-diameter implants, were subsequently used to support the final restoration. NDIs with diameters of less than 3 mm can achieve excellent long-term osseointegration and may be used together with conventional implants for definitive prosthodontic treatment as demonstrated by the 11-year follow-up reported in this case.
Placing implants in prosthetically ideal positions in the atrophic maxilla is challenging and often requires soft- and hard-tissue augmentation procedures prior to, or simultaneously with, implant placement.1,2 Considering the complexity and treatment time, correct sequential planning is crucial to achieving predictable long-term results while satisfying the patient’s expectations for function and esthetics. The use of narrow-diameter implants (NDIs) presents an invaluable modality for restoring an edentulous atrophic maxillary area in the provisionalization, augmentation, and final restorative phases of therapy.
All NDIs in this case report were category 1, according to the Klein classification, and are defined as implants with a less-than-3-mm diameter.3 These implants have been used to support removable and fixed dental prostheses since they were introduced in 1994.4 Among the articles that have been published on NDIs reporting survival rates comparable with conventional implants, Klein et al,3 in a systematic review of the literature, reported NDI survival rates between 90.9% and 100%.
The original function of NDIs was to support fixed interim prostheses during the osseointegration phase of conventional implants to avoid transmucosal loading that could compromise the final outcome. Following this initial healing period, the NDIs would be removed. It was later reported that the removal of these implants could be difficult because of the various degrees of integration they achieved.5 Froum et al6 confirmed this finding in a histologic study with machined-surface transitional implants. They analyzed the percentage of bone-to-implant contact (BIC) for NDIs after an average functioning period of 10.8 months. The values obtained were similar to the percentage of BIC of conventional turned, machined-surface implants. The results indicated that NDIs were able to achieve the same degrees of integration as implants with conventional diameters.6
In 2004 the US Food and Drug Administration approved the use of NDIs in the human jawbone for long-term use.7 Several authors have showed successful results when NDIs were used to support definitive prostheses.8-12 Furthermore, in a 2013 systematic review, Bidra and Almas13 reported a 94.7% survival rate of NDIs (diameter <3 mm) when used exclusively for definitive prosthodontics treatment. NDIs have been successfully used to support both transitional and fixed prostheses, thus providing clinicians with a simplified treatment option in areas of limited alveolar bone dimensions. In addition, they typically cost less than conventional implants and, in many cases, are able to be placed with a flapless procedure, which decreases patient postsurgical discomfort and morbidity.
This case report presents an 11-year follow-up of a patient in whom NDIs were used to support both the provisional and final restorations. The planning and sequencing of the procedures, including provisionalization, ridge augmentation, and final NDIs-conventional implants–supported restorations, will be discussed to illustrate the use of NDIs in the various phases of treatment.
Case Report
In 2004, a 30-year-old male was referred to the Ashman Department of Periodontology and Implant Dentistry of New York University College of Dentistry. The patient was a nonsmoker with an unremarkable medical history. His chief complaint was discomfort with his existing six-unit removable partial denture (Nos. 7 through 12), which he said he “could not tolerate” (Figure 1). He desired a fixed prosthesis. Two years earlier, severe trauma to the anterior maxilla had caused the loss of teeth Nos. 7 through 12 and the subsequent loss of supporting bone and soft tissues (Figure 2 and Figure 3). A computerized tomography scan revealed a deficient volume of buccolingual crestal bone and the need for a bone regeneration procedure prior to implant placement.
The treatment plan was to first provide the patient with a fixed provisional restoration that would afford function and protect the planned grafted site. Four NDIs were planned to support an acrylic provisional prosthesis prior to the augmentation procedure and during the healing period. This was to be followed by replacement of two of the NDIs with three conventional-diameter implants to support the definitive prosthesis.
Surgical Procedures
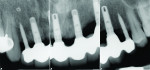
Placement of four NDIs (1.8 mm x 14 mm) (ANEW®, Dentatus, www.dentatus.com) guided by a CAD/CAM surgical template (iGuide, Midwest Dental Arts, www.midwestdentalarts.com) was performed without flap elevation (Figure 4 and Figure 5). A single 1.4-mm pilot drill (CePo®, Dentatus) was used to prepare the osteotomy under copious irrigation at 1000 RPMs. The four NDIs were subsequently inserted at low speed (30 RPM) in position Nos. 7 through 9 and 12 (Figure 6 and Figure 7). Primary stability was tested with a torque driver and found to be sufficient for immediately loading the implants. Following placement of the NDIs, the patient’s provisional restoration was connected chairside.
The design of the ANEW implants allowed fabrication of a screw-retained fixed restoration that was retrievable. Four openings were drilled in the patient’s acrylic prosthesis to ensure proper fit. A coping was attached to each of the four NDIs and secured in place with a screw cap. This coping assembly was then processed into the partial restoration using a self-curing acrylic resin (Bosworth TrueRepair®, Keystone Industries, www.keystoneindustries.com). The access holes for the screws were blocked with cotton pellets and sealed with off-color resin for easy re-access (Figure 8).
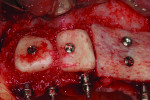
The bone augmentation procedure was performed 2 months following implant placement. The patient was given a prescription of amoxicillin 2000 mg 1 hour prior to surgery. Because of the large dimension of the horizontal defect, both allogeneic bone block grafts and autogenous bone blocks, harvested from the right ascending mandibular ramus, were used. Crestal and intrasulcular incisions were made in the regions of teeth Nos. 6 through 15 around all teeth and NDIs. The autogenous bone block was sectioned in two pieces and shaped to eliminate sharp corners. After decortication, the two segments were fixated using two screws (OsteoMed, www.osteomed.com) in the region of missing teeth Nos. 7 through 10. The allogeneic bone block, which was also shaped, was fixated after decortication with two screws on the buccal aspect of missing teeth Nos. 10 through 12. The spaces were filled with particulate allogeneic graft (Puros Cancellous Particulate Allograft®, Zimmer Dental, www.zimmerdental.com) to obtain a homogenous surface (Figure 9). The grafted area was covered with two resorbable collagen membranes (Bio-Gide®, Geistlich Pharma, www.geistlich-pharma.com) that were stabilized with five tacks (truFIX, ACE Surgical, www.acesurgical.com) (Figure 10). A periosteal releasing incision was made to achieve tension-free closure using resorbable sutures (Coated Vicryl® 4.0, Ethicon, www.ethicon.com). To prevent transmucosal pressure on the tissues, which may have interfered with the healing process and the integration of the bone grafts, the buccal flange of the provisional was trimmed (Figure 11). Following surgery, amoxicillin 500 mg TID for 10 days and chlorhexidine 0.12% mouthrinse (Peridex™, 3M ESPE, www.3MESPE.com) BID for 2 weeks were prescribed. The healing process was uneventful.
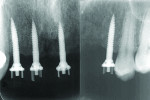
Five months later, the block grafts appeared well integrated, and no signs of inflammation or bone resorption were noted. Two of the four NDIs (Nos. 7 and 12) were retained as planned and supported the provisional, while the other two (Nos. 8 and 9) were removed and replaced with three standard-diameter implants (3.5 mm x 13 mm) (Zimmer Dental) in sites Nos. 8, 9, and 11. Healing abutments were connected to these three implants (Figure 12). Due to a partial resorption of the allogeneic block graft, implant No. 11 was placed slightly more apical than Nos. 8 and 9, and a guided bone regeneration procedure was performed simultaneously using particulate allogeneic graft (Puros Cancellous Particulate Allograft) and a resorbable collagen membrane (Bio-Gide). The flap was sutured with absorbable 4-0 chromic gut sutures (Ethicon). The augmented area was submerged while implants Nos. 8 and 9 and their healing abutments were left exposed (Figure 13). The provisional was relined with TrueRepair to close the access holes through which NDIs Nos. 8 and 9 had been connected to the restoration and to cover the two non-submerged healing abutments. At this stage, the provisional remained connected and supported only by two NDIs (Nos. 7 and 12).
Four months later, a new provisional, supported by all five implants, was delivered (Figure 14). Once the healing of the soft tissues was completed, the final impression was taken and the final restoration was delivered (Figure 15).
Follow-up
Eleven years later, the patient, who lived in London, returned to the New York University periodontology and implant dentistry department for follow-up. Radiographic evaluation demonstrated complete implant integration with no bone resorption around either the standard-diameter implants or the NDIs (Figure 16). One of the titanium tacks that secured the membrane had remained above the No. 7 NDI. Because the tack was well tolerated with no hard- or soft-tissue pathology, it was allowed to remain in place. Clinically, no signs of soft-tissue inflammation were noted (Figure 17 and Figure 18), and the patient reported complete satisfaction with the function and esthetics of his fixed restoration.
Discussion
Implant treatment in an extremely atrophic maxilla is challenging for clinicians and requires careful evaluation, planning, and execution to achieve long-term success and fully satisfy the patient’s expectations. The surgeon, restorative dentist, and laboratory technician must work in collaboration to achieve the desired outcome.
In the present case, the patient’s desire was to replace his removable partial denture with a fixed restoration. Oftentimes, patients do not tolerate removable prostheses well, especially when the tooth loss was sudden and caused by trauma or hopeless teeth need to be removed. Furthermore, when augmentation procedures are necessary, regardless of the final restorative options, protecting the grafted area and maintaining graft immobilization are essential to achieve success.14 Using a fixed provisional restoration is usually preferable, but many times this entails preparing healthy teeth to function as abutments. Another option is to immediately load the implants; however, this risks complications and failure when implants are placed in augmented sites.
A more predictable option is the use of NDIs, which can be placed in residual bone and support a fixed provisional restoration during the first phase of restoring function and during the time necessary for graft healing. The NDIs in the Nos. 7 and 12 positions were retained in the final prosthesis for the following reasons: First, they supported the provisional while the conventional-diameter implants—Nos. 8, 9, and 11—were allowed to integrate, which avoided transmucosal loading and provided a fixed provisional. Second, the width gained following block grafting in the No. 12 area was insufficient to place a conventional-diameter implant and still maintain at least 1 mm of buccal bone. Third, these implants continued to be stable with no bone loss and were, therefore, included as abutments in the final splint.
Narrow-diameter implants are designed to be placed with a nonsubmerged protocol and then immediately loaded to support fixed interim prostheses.15 Findings from histologic studies have confirmed their bone integration at the light microscopic level, and their removal has been noted to be difficult.5,13 In a systematic review of the literature, Klein et al3 reported a survival rate between 90.9% and 100% for implants with diameters of less than 3 mm (the mean functional follow-up ranged between 12 and 96 months). Shatkin and Petrotto11 in a retrospective analysis of 5640 mini implants supporting fixed and removable prostheses found an overall implant survival rate of 92.1%. Although NDIs were originally introduced to support provisional restorations, the Food and Drug Administration, considering high-survival–rate data, approved their use for long-term prosthodontic treatment in 2004.7
Although some in vitro studies16,17 reported a higher risk for overload and fracture for NDIs, these findings have not been confirmed clinically. When NDIs are used properly, long-term success without complications can be achieved, as this report demonstrates.
Using an increased number of implants was suggested to overcome the risk for overload complications.16 A more predictable alternative is to splint NDIs to conventional-diameter implants. This strongly reduces stress levels in the surrounding bone tissue18,19 and may provide a more even distribution of strains during off-axis loading that could occur clinically.20
While the 11-year follow-up in the present case report demonstrates that long-term success could be achieved using this protocol, patient compliance played a key role in the outcome. In addition, the London dentist reported that the patient had professional dental maintenance every 3 months while in London. The patient’s oral hygiene was optimal for the duration of the treatment and then for years following the delivery of the final restoration. The patient also followed post-surgery instructions to not chew on the provisional or overload the implants for 3 to 4 months. The patient’s expectations were fully satisfied, and he was grateful for the treatment received.
Conclusion
Maxillary atrophic anterior ridges represent a challenge for the surgeon and restorative dentist. A well-planned treatment protocol, based on the close collaboration between the treating clinicians and laboratory, is a prerequisite for success. Through the careful evaluation and planning of the case, the clinicians must assess the advantages and disadvantages of the various therapy alternatives, selecting the most appropriate option to achieve long-term success and satisfy patient expectations.
When bone-regeneration procedures are needed in order to place and restore an implant-supported restoration, various techniques have shown a high percentage of success. A requirement for effective bone regeneration is the avoidance of loading and movement during the healing process. A fixed interim restoration supported by NDIs protects the augmented site and represents a more comfortable and acceptable solution for most patients when compared to a removable denture. The use of NDIs presents a valuable modality in supporting fixed provisionals and does not require adjacent teeth to be prepared. Furthermore, these implants achieve excellent osseointegration and may be used long term to support the definitive prosthesis when splinted to standard-diameter implants.
Disclosure
The authors had no disclosures to report.
About the Authors
Stuart J. Froum, DDS
Clinical Professor and Director of Clinical Research
Ashman Department of Periodontology and Implant Dentistry
New York University College of Dentistry
New York, New York
Private Practice
New York, New York
Sang-Choon Cho, DDS
Clinical Assistant Professor
Director of Advanced Program for International Dentists in Implant Dentistry, and Co-Director of Clinical Research
Ashman Department of Periodontology and Implant Dentistry
New York University College of Dentistry
New York, New York
Salvatore Florio, DDS
Resident
Ashman Department of Periodontology and Implant Dentistry
New York University College of Dentistry
New York, New York
Craig M. Misch, DDS, MDS
Private Practice limited to Oral and Maxillofacial Surgery
Sarasota, Florida
References
1. Belser UC, Schmid B, Higginbottom F, Buser D. Outcome analysis of implant restorations located in the anterior maxilla: a review of the recent literature. Int J Oral Maxillofac Implants. 2004;19 suppl:30-42.
2. Funato A, Salama MA, Ishikawa T, et al. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007;27(4):313-323.
3. Klein MO, Schiegnitz E, Al-Nawas B. Systematic review on success of narrow-diameter dental implants. Int J Oral Maxillofac Implants. 2014;29 suppl:43-54.
4. Barber HD, Seckinger RJ. The role of the small-diameter dental implant: a preliminary report on the Miniimplant system. Compendium. 1994;15(11):1390,1392.
5. Simon H, Caputo AA. Removal torque of immediately loaded transitional endosseous implants in human subjects. Int J Oral Maxillofac Implants. 2002;17(6):839-845.
6. Froum SJ, Simon H, Cho SC, et al. Histologic evaluation of bone-implant contact of immediately loaded transitional implants after 6 to 27 months. Int J Oral Maxillofac Implants. 2005;20(1):54-60.
7. Food and Drug Administration website. Access Data. Rockville, MD: US Dept of Health and Human Services; September 13, 2004. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn_template.cfm?id=k040143. Accessed April 1, 2016.
8. Vigolo P, Givani A. Clinical evaluation of single-tooth mini-implant restorations: a five-year retrospective study. J Prosthet Dent. 2000;84(1):50-54.
9. Mazor Z, Steigmann M, Leshem R, Peleg M. Mini-implants to reconstruct missing teeth in severe ridge deficiency and small interdental space: a 5-year case series. Implant Dent. 2004;13(4):336-341.
10. Froum SJ, Cho SC, Cho YS, et al. Narrow-diameter implants: a restorative option for limited interdental space. Int J Periodontics Restorative Dent. 2007;27(5):449-455.
11. Shatkin TE, Petrotto CA. Mini dental implants: a retrospective analysis of 5640 implants placed over a 12-year period. Compend Contin Educ Dent. 2012;33 spec 3:2-9.
12. Anitua E, Saracho J, Begoña L, Alkhraisat MH. Long-term follow-up of 2.5-mm narrow-diameter implants supporting a fixed prostheses. Clin Implant Dent Relat Res. 2015 Apr 27. doi: 10.1111/cid.12350. [Epub ahead of print]
13. Bidra AS, Almas K. Mini implants for definitive prosthodontic treatment: a systematic review. J Prosthet Dent. 2013;109(3):156-164.
14. Misch CM. Maxillary autogenous bone grafting. Oral Maxillofac Surg Clin North Am. 2011;23(2):229-238.
15. Krennmair G, Krainhöfner M, Weinländer M, Piehslinger E. Provisional implants for immediate restoration of partially edentulous jaws: a clinical study. Int J Oral Maxillofac Implants. 2008;23(4):717-725.
16. Bourauel C, Aitlahrach M, Heinemann F, Hasan I. Biomechanical finite element analysis of small diameter and short dental implants: extensive study of commercial implants. Biomed Tech (Berl). 2012;57(1):21-32.
17. Allum SR, Tomlinson RA, Joshi R. The impact of loads on standard diameter, small diameter and mini implants: a comparative laboratory study. Clin Oral Implants Res. 2008;19(6):553-559.
18. Bergkvist G, Simonsson K, Rydberg K, et al. A finite element analysis of stress distribution in bone tissue surrounding uncoupled or splinted dental implants. Clin Implant Dent Relat Res. 2008;10 (1):40-46.
19. Jofre J, Cendoya P, Munoz P. Effect of splinting mini-implants on marginal bone loss: a biomechanical model and clinical randomized study with mandibular overdentures. Int J Oral Maxillofac Implants. 2010;25(6):1137-1144.
20. Yilmaz B, Seidt JD, McGlumphy EA, Clelland NL. Comparison of strains for splinted and nonsplinted screw-retained prostheses on short implants. Int J Oral Maxillofac Implants. 2011;26(6):1176-1182.