You must be signed in to read the rest of this article.
Registration on AEGIS Dental Network is free. Sign up today!
Forgot your password? Click Here!
Immediate Implant Full-Arch Loading: Case Selection and Technique
Three case examples utilizing the All-on-4 treatment protocol
Olga Malkin, DMD, FICOI
For most patients, losing teeth is emotional. In the past, the only treatment option for patients who were about to lose all their remaining natural teeth was to provide them with an immediate denture followed by implant placement after 6 months of bone and soft tissue healing. This lengthy and uncomfortable protocol discouraged many patients from undergoing this treatment. Those who chose to proceed had to cope with wearing removable dentures for at least 1 year. Studies have demonstrated that removable denture wearers were reluctant to participate in social activities and embarrassed to speak or eat in public. They exhibited loss of self-esteem, symptoms of depression, premature aging, and even increased risk for early death.1,2
The All-on-4 Protocol
In the past 10 years, implant dentistry has been experiencing exciting changes associated with the introduction of immediate implant-load treatment modalities for fully edentulous patients. The introduction of the All-on-4® (Nobel Biocare, www.nobelbiocare.com) implant treatment concept makes it possible to provide treatment for patients who experienced significant bone loss in the posterior maxilla and mandible without needing complex bone-grafting procedures, which often require a staged approach for full-arch implant rehabilitation. With the All-on-4 protocol, only four implants are required to stabilize a full-arch fixed prosthesis. Therefore, the best sites for implant placement can be identified and utilized, making immediate full-arch prosthesis possible. Tilted posterior maxillary implants can be utilized to avoid a sinus-lift procedure, and tilted mandibular implants make it possible to restore posterior teeth with minimum prosthetic cantilever in the area where axial implant cannot be placed or where short implants, which are not suitable for immediate-load protocol, would have been used.
Predictability of full-arch immediate implant supported fixed prosthesis on the mandible has been successfully described in scientific literature as early as the 1990s. Multicenter studies showed a 85% to 97% success rate for such treatments.3,4 After the All-on-4 concept was introduced by Dr. Paulo Malo in 2002, the overall success rates of tilted implant therapy have exceeded 90% for both the maxilla and mandible.5,6
The All-on-4 treatment concept is not only for the patients who are already edentulous. It can also be successfully applied to patients transitioning from terminal dentition to full-arch implant-supported dentition in one surgical procedure because the use of the available bone is maximized.7 For this type of patient, after the hopeless teeth are removed, two axial implants can be placed in the anterior region, two tilted implants can be placed in the posterior area, and an immediate full-arch temporary screw-retained prosthesis can be fabricated and loaded using multi-unit abutments (Nobel Biocare).
Careful comprehensive treatment planning and establishing good communication among all team members (ie, restorative dentist, surgeon, laboratory technician) are the keys to a successful full-arch immediate-load implant treatment. However, this type of treatment starts with identifying patients suitable for the procedure. A comprehensive diagnosis is important for all implant cases, including 3D imaging with CBCT to evaluate and identify available bone. It should be utilized for all immediate-load implant cases. Sometimes a practitioner may not recognize a good candidate for transitioning from a terminal dentition to an implant-supported dentition utilizing immediate-load treatment concept. One should consider the patient’s esthetic expectations, commitment to lengthy treatment, previous dental experience, and finances when choosing an appropriate treatment plan.
Case Example 1
A 55-year-old woman presented to the office unhappy about the health and appearance of her teeth. A previous dentist had advised that all her teeth had to be removed. However, she delayed treatment, as she was not comfortable with the idea of wearing removable dentures during healing.
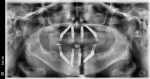
Clinical examination revealed moderate-to-severe generalized periodontitis of the remaining dentition, multiple carious lesions, and defective crown restoration. The patient exhibited a slightly collapsed vertical dimension of occlusion (VDO) and supereruption of some upper and lower anterior teeth (Figure 1). After discussing treatment options with the patient, the decision was made to remove the remaining teeth and rehabilitate her dentition utilizing the All-on-4 immediate-load protocol. The smile-line evaluation, for which the patient was asked to produce an exaggerated smile to observe if the attached gingiva was visible, did not reveal a gingival display (Figure 2). Therefore, bone reduction was not necessary to hide the transition line between the prosthesis and soft tissue. This patient’s VDO was only slightly collapsed, and the anterior teeth were present with close-to-adequate lip support. Therefore, All-on-4 treatment could be predictably planned on a semi-adjustable articulator because existing dentition could serve as a guide for an idealized tooth position for an immediate provisional prosthesis.
Once the immediate denture set-up was done, the restorative space between edentulous ridges was evaluated on an articulator and was deemed adequate at 24 mm. This confirmed that bone reduction was not needed to accommodate the prosthesis. According to the literature, the minimum space per arch for a screw-retained prosthesis with metal framework and wraparound acrylic should be 11 to 12 mm.8 A set of dentures was fabricated and converted to an implant-supported prosthesis immediately following implant placement. The patient was happy with the esthetic and functional outcome (Figure 3 and Figure 4).
Case Example 2
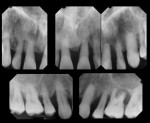
A 42-year-old male patient complained of loose upper teeth and the overall appearance of his smile (Figure 5 and Figure 6). Due to severe periodontal disease, he required a staged treatment in which some of his teeth would be removed, remaining teeth would be treated with periodontal surgery, and missing teeth would be replaced with implants.
His main concern was the duration of the treatment, as his job required extensive travel. He could not commit to a treatment plan with a large number of appointments or long downtime. He was also not comfortable with wearing removable dentures or a partial because he spoke to groups of people every day and attended dinners with clients. The predictability of a long-term outcome and finances were also important. After learning about different options, the patient chose an All-on-4 treatment concept to immediately load the implants on the maxilla following removal of his existing teeth.
Findings from the clinical examination revealed that the patient had an adequate VDO and appropriate tooth position. On the forced smile, 0 to 3 mm of the gingiva was visible above all maxillary teeth (Figure 6). Therefore, bone and soft tissue removal was required to hide the transition line between the prosthesis and gingiva. The case was mounted on a semi-adjustable articulator. Again, similar to the first case, existing dentition and radiographs were utilized to predictably address the bone reduction and fabricate a diagnostic set-up for an immediate screw-retained provisional prosthesis. The overall tooth position was kept the same as in the natural dentition. The spaces between the teeth were closed by using denture teeth, which were slightly wider than the patient’s natural anterior dentition.
The patient was happy with the esthetic outcome and function of the immediate provisional screw-retained prosthesis. The tooth arrangement of the provisional prosthesis is similar to his natural dentition, which made the esthetic outcome predictable (Figure 7 through Figure 9). The treatment was completed in one appointment under intravenous sedation. The patient was able to return to his full travel schedule less than 1 week after surgery.
Case Example 3
A 72-year-old female patient reported she was unhappy with her smile. Not only did she believe her teeth made her look old, but she also had difficulty chewing. The patient was also not comfortable undergoing a prolonged dental treatment that required wearing a removable prosthesis.
The smile evaluation revealed that only 2 to 3 mm of tooth structure was visible on a forced smile (Figure 10). Therefore, bone reduction was not required to hide the transition line. On oral and facial examinations, it was determined that the patient had a severely collapsed VDO and tooth position that did not offer adequate lip support (Figure 11). In addition, due to her skeletal anatomy, it would not be possible to appropriately increase her VDO to achieve desired lip support with tooth-supported restorations of the proper tooth-to-root ratio and contours. The VDO for this patient was established utilizing vertical dimension at rest (VDR) and subtracting 3 mm of freeway space from VDR to determine VDO. VDR was measured by asking the patient to open and slowly close her mouth until her lips lightly touched and measuring the distance between the small dots placed on the tip of her nose and on the chin at this position.9 The distance between the dots was then measured when the patient was fully closed in VDO. The difference between VDO and VDR was 8 mm. Therefore, it was decided that VDO could be opened by 5 mm anteriorly. Photographs and the addition of composite restoration to the anterior teeth were used to determine a more esthetically pleasing position of the anterior teeth. A set of immediate dentures was fabricated. A new VDO with an appropriate anterior tooth position for lip support and esthetics was to be converted to implant-supported prosthesis immediately after tooth removal and implant placement.
After extraction and implant placement, multi-unit abutments (straight for anterior implants and 30° for posterior implants) and Temporary Coping Multi-units (Nobel Biocare) were attached to the implants (Figure 12). A prefabricated denture was drilled to fit over the temporary copings (Figure 13). The temporary copings were picked up intraorally using cold-cure acrylic in a monoject syringe (Figure 14 through Figure 16). The palate of the denture was removed, and voids were filled with the cold-cure acrylic. From the evaluation of the patient’s temporary prosthesis (Figure 17), it was obvious that even though no bone reduction was required and the patient did not have significant bone loss prior to surgery, a temporary prosthesis that had both denture teeth and a significant amount of pink acrylic was required to achieve appropriate VDO and lip support. The patient wore provisional implant-supported bridges for 6 months to confirm her satisfaction with the esthetics and the ability to function comfortably at the increased VDO. The final prosthesis was constructed with a titanium framework layered with Gradia® gingival composite (GC America, www.gcamerica.com) and porcelain-fused-to-metal crowns cemented over the titanium framework (Figure 18).
The final result shows a final prosthesis with appropriate VDO and an esthetically pleasing tooth position (Figure 19).
Discussion
Following comprehensive diagnosis and treatment planning, the process of which is beyond the scope of this article, the patients described here received their treatments in single procedures consisting of surgical and restorative components. Without this option, these patients would have not undergone or significantly delayed treatment, as they did not want to wear removable prostheses during healing.
By maximizing the use of the existing bone post-extraction, the All-on-4 immediate function treatment concept was used to provide each patient with an immediately loaded fixed prosthesis supported with four implants. In the surgical part of the procedure, the remaining teeth were removed, the bone recontoured if needed, and implants placed. In the restorative aspect, a pre-made denture was converted intraorally into an implant-supported screw-retained bridge attached to the implants utilizing multi-unit abutments and temporary titanium cylinders. Fabrication and design of the dentures to be converted to a screw-retained prosthesis for immediate implant loading follows the same rules as fabrication of a conventional immediate denture, which is part of everyday practice for many dental professionals. The predictability of the All-on-4 immediate loading protocol is well-supported in the literature, with implant and prosthesis survival rates reported to exceed 90% overall and found to be as high as 99.3% in maxilla and 100% in the mandible.10
Conclusion
Immediate implant loading for a full-arch prosthesis is well documented and shows excellent success rates. Not only does it decrease healing and treatment time but also makes it easier for patients to accept treatment knowing that only one surgical procedure will be required, thus avoiding wearing removable dentures. A team of surgical and restorative providers with appropriate patient selection and treatment planning can successfully execute this type of treatment.
Acknowledgement
The author would like to acknowledge Sanda Moldovan, DDS, MS, CNS, for her assistance in the cases presented in this article; as well as Sam Alawie, MDT with Beverly Hills Dental Laboratory, Inc.
Disclosure
Olga Malkin, DMD, FICOI, was a lecturer at the Nobel Biocare 2016 Global Symposium.
References
1. Mack F, Schwahn C, Feine JS, et al. The impact of tooth loss on general health related to quality of life among elderly Pomeranians: results from the study of health in Pomerania (SHIP-O). Int J Prosthodont. 2005;18(5):414-419.
2. Emami E, de Souza RF, Kabawat M, Feine JS. The impact of edentulism on oral and general health. Int J Dent. 2013;2013 :498305. doi: 10.1155/2013/498305.
3. Schnitman PA, Wöhrle PS, Rubenstein JE, et al. Ten-year results for Brånemark implants immediately loaded with fixed prostheses at implant placement. Int J Oral Maxillofac Implants. 1997;12(4):495-503.
4. Brånemark PI, Engstrand P, Ohrnell LO, et al. Brånemark Novum: a new treatment concept for rehabilitation of the edentulous mandible. Preliminary results from a prospective clinical follow-up study. Clin Implant Dent Relat Res.1999;1(1):2-16.
5. Maló P, Rangert B, Nobre M. “All-on-Four” immediate-function concept with Brånemark System implants for completely edentulous mandibles: a retrospective clinical study. Clin Implant Dent Relat Res. 2003;5(suppl 1):S2-S9.
6. Maló P, Rangert B, Nobre M. All-on-4 immediate-function concept with Brånemark System implants for completely edentulous maxillae: a 1-year retrospective clinical study. Clin Implant Dent Relat Res. 2005;7(suppl 1):S88-S94.
7. Maló P, Nobre M, Rangert B. Implants placed in immediate function in periodontally compromised sites: a five-year retrospective and one-year prospective study. J Prosthet Dent. 2007;97(6 suppl):S86-S95.
8. Chee W, Jivraj S. Treatment planning of the edentulous mandible. British Dental Journal. 2006;201:337-347. doi:10.1038/sj.bdj.4814041.
9. Toolson LB, Smith DE. Clinical measurement and evaluation of vertical dimension. J Prosthet Dent. 1982;47(3):236-241.
10. Babbush CA, Kutsko GT, Brokloff J. The all-on-four immediate function treatment concept with NobelActive implants: a retrospective study. J Oral Implantol. 2011;37(4):431-445.