You must be signed in to read the rest of this article.
Registration on AEGIS Dental Network is free. Sign up today!
Forgot your password? Click Here!
Occlusal Augmentation of an Ankylosed Primary Second Molar with No Premolar Successor
Using PULPDENT’S ACTIVA™ BioACTIVE-RESTORATIVE™
Theodore P. Croll, DDS | Richard R. Cavanaugh, DDS
Ankylosed primary second molars with no premolar successor offer difficult challenges for dentists. They must consider the following: When is the ankylosis so severe that extraction is required? What is the patient’s age and dental maturity? Is orthodontic treatment indicated for the patient? What is the status of the roots? Are they resorbing? Are they thin? Are they complete with no evidence of resorption? Has space been lost by “tip-over” of adjacent permanent teeth?
In 1994, the authors reported on the fabrication of resin-bonded ceramic onlays for retained primary molars with infraocclusion.1 In such cases, as long as the primary molar has good root structure remaining and there are no other factors influencing treatment, a laboratory-fabricated porcelain onlay can be bonded to the primary tooth. This would effectively re-establish proper occlusion and mesio-distal contacts. Normal function can be achieved for the teen years and into adulthood until circumstances necessitate extraction and prosthetic replacement. A primary molar retained for a longer period of time will result in better osseous support for an implant. Significant boney resorption and reshaping occur after extraction of the primary molar, so root preservation for as long as possible is a worthy goal. The authors have seen primary second molars with no premolar successor last for decades.
Besides laboratory-fabricated porcelain onlays, bonded resin-based composite or a new “resin-modified glass-ionomer bioactive ionic resin-based composite”2 can also be used for enhancing coronal height and peripheral dimensions with no laboratory component to treatment.
This brief report documents mesio-occlusal repair of an ankylosed, carious mandibular primary second molar that had no succedaneous premolar. The restoration design included placement of an occlusal platform using ACTIVA™ BioACTIVE-RESTORATIVE™ (PULPDENT®, www.pulpdent.com) material.
Case Report
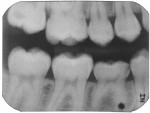
A 13-year-old girl had a retained ankylosed mandibular right primary second molar (Figure 1). The tooth had occlusal caries. In addition, a bitewing radiograph and lateral transillumination revealed a substantial caries lesion on the mesial surface (Figure 2). A panograph from a year prior (not pictured) showed congenital absence of the second premolar.
The patient was scheduled for mesio-occlusal restoration using bonded ACTIVA™ Restorative material.2 The plan was to fabricate a traditional mesio-occlusal bonded tooth-colored restoration with a raised occlusal section serving as a bite platform to occlude with the opposing premolar.
Treatment
After right inferior alveolar block anesthesia, a rubber dam was positioned, using the “slit dam” method.3 A standard Class I occlusal surface preparation, including all carious pits and fissures, was performed using a water-cooled inverted cone diamond bur (Figure 3). The inverted cone shape provided mechanical undercutting of the preparation for additional retention of the bite platform. Enamel peripheral to the preparation was roughened with a large round bur at slow speed. A mesial proximal box was then cut with a cylindrical diamond bur. Carious dentin and enamel was debrided using a slow-speed No. 6 round bur.
A 0.0015-inch x 0.25-inch matrix strip (Strip-T, DENOVO Dental, www.denovodental.com) was contoured with pliers, positioned into the mesial interproximal space, and secured with a wooden wedge. Another matrix strip was contoured, inserted, and stabilized with a wooden wedge distally. The strips were wedged into place in such a way that they rose up several millimeters above the height of the respective marginal ridges (Figure 4).
The enamel surface was saturated with a self-etching resin-bonding agent (Adper™ Prompt™ Self-Etch Adhesive, 3M, www.3m.com) for 30 seconds, without covering the exposed dentin in the internal aspects of the preparation. The resin-modified glass-ionomer component of ACTIVA Restorative chemically bonds to the cut dentin without a resin-bonding agent. Excess bonding agent was cleared with a dry applicator brush. The bonding agent was exposed to the visible light beam for 10 seconds.
The two components of ACTIVA Restorative were expressed from the double-barreled syringe container, blended on a mixing pad, and inserted into a fine-tipped AccuDose® syringe tip (CENTRIX INC, www.centrixdental.com).2 The first increment of material was injected, filling the mesial proximal box, and was then light-polymerized with a 20-second light beam exposure. Much care was taken to avoid air bubble inclusion in the material. One more increment of material was then injected in such a way that the occlusal table was elevated several millimeters (Figure 4).
The new occlusal table was exposed to the light beam (1,200 mW/cm2) from the occlusal, buccal, and lingual aspects for 20 seconds on each surface. The matrix strips were removed, and the occlusal platform was sculpted and trimmed to occlude ideally with the opposing premolar (Figure 5 and Figure 6). Blue articulating paper was used to ascertain contact during mandibular excursions (Figure 7).
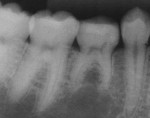
Fourteen months later, the ACTIVA Restorative platform had virtually identical contact with the opposing premolar. In addition, there was no evidence of wear or marginal chipping or staining (Figure 8 and Figure 9) and the root structure was sound with no evidence of resorption (Figure 10 and Figure 11).
Discussion
The enamel etching step in this procedure could also have been completed using the standard phosphoric acid-etch/water-rinse/air-dry protocol, rather than the self-etching bonding agent, Adper Prompt. However, with a 30-second etch time, the Prompt fluid, which has an extremely low pH, etches diamond-roughened surface enamel very effectively on both primary and permanent teeth. The senior author has used the Prompt system for enamel etching and bonding in this manner since 1999.
It is questionable whether acid-etch retained resin-based composite or the ACTIVA Restorative material would remain attached for the long term had the mesio-occlusal preparation not been required in this case. Masticatory and occlusal impact forces conceivably could have eventually detached the occlusal platform if mechanically interlocking retention form was not part of this preparation. In this case, it was a moot point because the patient had both mesial and occlusal caries lesions, and Class II preparation was required anyway. The substantial dentin involvement warranted repair with resin-modified glass-ionomer material, and ACTIVA Restorative filled that need, serving as a biomimetic dentin and enamel replacement. It is logical that any resin-based composite used for posterior tooth repair could be used in this technique. However, if that was the case, stratification using a resin-modified glass-ionomer liner/base would have been advisable.4,5 ACTIVA Restorative was also chosen for this patient for several other reasons.
The senior author has restored 537 permanent teeth and 531 primary teeth with ACTIVA Restorative material, and 18-month observations are all favorable. ACTIVA Restorative has been described as a “resin-modified glass-ionomer bioactive ionic resin-based composite.”2 The material has characteristics of both resin-modified glass-ionomer cement and resin-based composites. Studies have shown it to have wear resistance and fracture strengths that are equivalent to certain resin-based composites, while offering the advantages of resin-modified glass-ionomer systems.6-8 In addition, there is a chemical curing reaction along with photopolymerization and material hardening from the glass-ionomer acid/base neutralization reaction. The three hardening mechanisms, along with low polymerization shrinkage, allowed for placement of only two increments in the build-up stage.
Final Thought
More studies regarding physical characteristics and long-term performance of ACTIVA Restorative are ongoing. The patient pictured here will be followed to assess the status of the roots and occlusal relationships. Implant/crown replacement will be considered in future years, as necessary.
Disclosure
Theodore P. Croll, DDS, has financial interest in DENOVO’s Strip T Matrix by virtue of a patent licensing agreement.
Richard R. Cavanaugh, DDS, has no financial interest in any product or manufacturer mentioned in this article.
References
1. Cavanaugh RR, Croll TP. Resin-bonded ceramic onlays for retained primary molars with infraocclusion. Quintessence Int. 1994;25(7):459-463.
2. Croll TP, Berg JH, Donly KJ. Dental repair material: a resin-modified glass-ionomer bioactive ionic resin-based composite. Compend Contin Educ Dent. 2015; 36(1):60-65.
3. Croll TP. Alternative methods for use of the rubber dam. Quintessence Int. 1985;16(6):387-392.
4. Croll TP, Cavanaugh RR. Posterior resin-based composite restorations: a second opinion. J Esthet Restor Dent. 2002;14(5):303-312.
5. Croll TP, Swift EJ Jr. Tissue-specific, biomimetic, direct-application tooth repair. J Esthet Restor Dent. 2013; 25(3):156-158.
6. Garcia-Godoy F, Morrow BR, Pameijer CH. Flexural strength and fatigue of new Activa RMGICs [abstract]. J Dent Res. 2014;93(spec iss A). Abstract 254.
7. Girn VS, Chao W, Harsono M, et al. Comparison of deflection at break of four dental restorative materials [abstract 2375]. Presented at IADR/AADR/CADR General Session & Exhibition; Boston, Massachusetts; March 11-14, 2015.
8. Bansal R, Beck P, Lawson N, Burgess J. Wear of a calcium, phosphate and fluoride releasing restorative material. Am Dent J. In press.
About the Author
Theodore P. Croll, DDS
Affiliate Professor
Department of Pediatric Dentistry
University of Washington
School of Dentistry
Seattle, Washington
Adjunct Professor
Pediatric Dentistry
University of Texas Health
Science Center at San Antonio
San Antonio, Texas
Private Practice
Doylestown, Pennsylvania
Richard R. Cavanaugh, DDS
Clinical Associate Professor
Maurice Kornberg School of Dentistry Temple University
Philadelphia, Pennsylvania
Private Practice
Doylestown, Pennsylvania