You must be signed in to read the rest of this article.
Registration on AEGIS Dental Network is free. Sign up today!
Forgot your password? Click Here!
10 Keys for Successful Esthetic-Zone Single Immediate Implants
Robert A. Levine, DDS; Jeffrey Ganeles, DMD; Luiz Gonzaga, DDS, MS; Joseph Y. Kan, DDS, MS; Harry Randel, DMD; Chris D. Evans, BDSc, MDSc, MRACDS; and Stephen T. Chen, BDS, MDSc, PhD, FRACDS
Abstract:
The 10 keys for successful esthetic-zone single immediate implants encapsulate in an evidence-based manner the treatment planning and replacement of single hopeless teeth in the maxillary anterior sextant. These include 2 treatment-planning, 5 surgical, and 3 prosthetic keys, which, collectively, aim to minimize soft- and hard-tissue complications for an optimal esthetic implant restoration. The straightforward, advanced, and complex (SAC) classification was designed to aid clinicians in the treatment planning of dental implant cases. Cases are stratified by the degree of surgical and restorative risk and complexity for both the surgical and prosthetic phases of treatment. Based on the 10 keys, the management of an immediate implant in the esthetic zone is considered a complex SAC procedure. As described in this article, a complex SAC procedure requires careful patient selection and treatment planning, along with precise execution by skillful clinicians, to achieve successful results.
The straightforward, advanced, and complex (SAC) classification system1 was developed to aid clinicians in the treatment planning of dental implant cases. Treatment of a single-tooth replacement in the esthetic zone is considered a complex procedure requiring a team approach.2 This is because once an esthetic complication occurs, restoring the lost hard and soft tissues to their original presurgical levels is extremely difficult.3-6
According to Levine et al,4 immediate placement in the esthetic zone requires the clinician to be experienced and knowledgeable about esthetic diagnosis, minimally invasive extraction techniques, oral plastic-surgical procedures (eg, hard- and soft-tissue grafting, “gummy smile” correction/crown lengthening), and accurate 3-dimensional (3D) implant placement and restoratively driven planning/placement based on cone-beam computed tomography (CBCT) analysis. Tissue-contour management requires prosthetic knowledge of provisionalization techniques to sculpt peri-implant tissue for developing submergence contour from the implant shoulder to the mucosal zenith to adequately support the tissue. Final impression techniques must capture and transfer this submergence contour, or “transitional zone,” to be duplicated in the final crown.
In a 2009 systematic review, Chen et al6 suggested potential risk for facial gingival recession of was up to 30% of cases if inclusion criteria were not used for immediate implant placement. They identified preexisting defects of the facial bone, thin facial bone, thin soft-tissue biotype, and facial malposition of the implant as potential risk factors for gingival recession following immediate single-tooth implant placement.
Recent systematic reviews by Levine et al4 and Chen et al3 and consensus statements by Morton et al5 were written to organize the diagnosis, planning, and treatment of single-tooth implants in the esthetic zone, along with the treatment of complications associated with them. Their conclusions3-5 suggested that a team protocol, if strictly followed, would provide high predictability in preventing esthetic complications related to single-tooth implants, and they proposed guidelines to ensure high success rates.
Since 2014, various studies have reported on the expansion of specific indications and techniques for immediate placement and restoration of implants in the esthetic zone. Outstanding short- and medium-term results have been achieved that are comparable with staged or delayed placement7-19; however, none of these more recent publications were included in the aforementioned 2014 systematic reviews,3,4 and they represent newer information and a somewhat different perspective. The purpose of this article is to identify 10 essential elements for performing immediate single-tooth replacement in the esthetic zone in adult patients with long-term, successful outcomes. This treatment procedure is defined as complex under the SAC classification and requires careful patient selection and treatment planning, as well as precise execution by skillful clinicians, to achieve successful results.
10 Keys Defined
The 10 keys are as follows:
1. Esthetic risk assessment (ERA). Each patient’s case is reviewed so his or her specific esthetic risk criteria for immediate placement in the esthetic zone can be determined.
2. Tomographic plan. CBCT analysis and a restorative-driven treatment plan are performed to assess adequate buccal bony-wall thickness and determine the sagittal root position (SRP) of the tooth, the alveolar form, and the planned implant position.
3. Minimally traumatic tooth extraction. Extraction is performed without flap reflection (if possible) with evaluation of the status of the buccal plate.
4. 3D implant placement in good available bone both apically and palatally along the palatal wall. This will help assure a, preferably, screw-retained provisional and final restoration. Ideally, an anatomically correct surgical guide template (ACSGT) is used.
5. Use of a narrower (3.3 mm to 4.3 mm) implant versus a wider-diameter (4.5 mm or greater) implant. A narrower implant will assure at least a 2-mm- to 3-mm-buccal gap adjacent to the intact buccal socket wall. This can be preplanned with a careful CBCT analysis and an understanding of the restorative-driven plan.
6. Buccal gap bone graft. A low-substitution mineralized bone material (deproteinated bovine bone mineral [DBBM] or freeze-dried bone allograft [FDBA]) is used to bone-graft the buccal gap.
7. Facial gingival grafting. This is done using palatal connective tissue placed in a buccal envelope under the buccal marginal tissue and facial to the intact buccal plate to augment the existing gingiva so that it is thick.
8. Immediate contour management of the emergence profile from the implant. The goal is to preserve the soft-tissue and transition-zone contours using an anatomically correct or slightly under-contoured emergence profile with either a screw-retained immediate provisional or a customizable healing abutment.
9. Custom impression coping technique. Once the team is satisfied with the soft-tissue esthetics developed in the provisional stage, a custom impression coping technique is used to duplicate the transition zone, which is replicated in the final impression and transferred to the laboratory model.
10. Final restoration with a screw-retained crown. If direct-screw retention is not possible, stock abutments should be avoided because it is difficult to remove excess cement from deep interproximal margins. An anatomically contoured customized abutment with a titanium implant interface should be fabricated with the final facial cement line no deeper than 1 mm circumferentially. If cemented restorations are needed, radiopaque cement should be used via a minimum cement load technique (ie, copy abutment technique).
Review of the 10 Keys
1. Esthetic Risk Assessment
Achieving a long-term esthetic result starts with comprehensive planning prior to surgical intervention and a restorative-driven approach1-6,20-24 (Figure 1 through Figure 4). A patient’s pretreatment implant evaluation in the esthetic zone should include an initial consultation to establish a diagnosis and prognosis based on a comprehensive examination of his or her medical, dental, and compliance history. The patient’s periodontal and restorative needs should also be considered. Diagnostic casts and necessary radiographs should include CBCT to evaluate important anatomic landmarks,25,26 skeletal relationships, and bone availability to aid in careful presurgical planning.
Skeletal dimensional stability, even if determined using serial cephalometric radiographs, is not a guarantee of growth cessation, even in adults. Patients should be informed that, despite using the best available prognostic practices, alveolar growth can recur or continue, and changes in restorations may be required in the future.27 Intraoral and extraoral digital photographs documenting the patient’s smile both at rest and in full smile are recommended to determine the lip line in relation to the gingival margins surrounding the tooth to be replaced. The location of the adjacent interproximal papillae should also be documented. These photographs aid in the comprehensive treatment planning of the case and may influence the surgical approach.1-5,28-31
During the presurgical evaluation and consultation, the clinician should also review the ERA (Figure 4) with the patient to establish the overall esthetic risk. This considers the patient’s smile line and esthetic demands, and establishes a comprehensive site analysis of hard- and soft-tissue thickness and width along with the patient’s gingival biotype. Per Yoshino et al8 the gingival biotype is categorized as thin or thick based on visibility of an underlying periodontal probe (SE Probe SD12 Yellow, American Eagle Instruments Inc., am-eagle.com) through the gingival tissues (ie, visible = thin; not visible = thick).
The ERA becomes part of the patient’s record along with the documentation of the discussion. The patient’s surgical and prosthetic concerns regarding the tooth being replaced and adjacent teeth should be included. Restorative modifiers such as cervical tooth shape, adjacent tooth restorative status, parafunctional status, skeletal and occlusal classification, and overbite/overjet relationship should be evaluated in relation to the proposed treatment. Articulated study casts and/or other digital records should be collected to assist with treatment-planning procedures.
2. Tomographic Planning
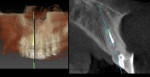
When placing implants in the esthetic zone, a presurgical CBCT scan provides invaluable information about the site, including the existing buccal plate width, anticipated need for bone grafting, anticipated implant width and length, and SRP (Figure 5). The CBCT information can also help determine if the anticipated implant site will need to be modified with orthodontic therapy or vertical extrusion (forced eruption) for site development.32 Based on limited studies and a general consensus among the scientific community, ideally ≥2 mm of buccal bone labial to the healed implant is considered necessary to ensure proper soft-tissue support and to avoid resorption of the buccal bone and gingival recession following restoration.4,33-35
A CBCT scan is strongly recommended to evaluate the patient’s buccal plate presence, dimension (which may not be visible if it is less than 1 mm thick), and ridge width.36 CBCT data will aid the team in preplanning the case and assessing the need for soft- and/or hard-tissue augmentation37,38 at the time of or prior to implant placement and whether immediate implant placement with immediate provisionalization can be performed. If the clinician has less than 1 mm of buccal bone facial to the root to be extracted, immediate placement might not be the preferred treatment because of increased risk for future tissue loss and recession. Instead, a lower risk treatment option—early implant placement—may be a consideration; it provides the opportunity for significant buccal augmentation using a staged approach.38
In relation to the SRP, Kan et al36 evaluated CBCT images of 100 patient retrospectively and classified the relationship of the SRP of the maxillary anterior teeth (600 samples) to their respective osseous housings (Class 1 to Class 4 categories). They found 81.1% were Class 1 (the root is positioned against the labial cortical plate: favorable for immediate placement), 6.5% were Class 2 (the root is centered in the middle of the alveolar housing without engaging either the labial or palatal cortical plates at the apical third of the root: technique-sensitive for immediate placement), 0.7% were Class 3 (the root is positioned against the palatal plate: technique-sensitive for immediate placement), and 11.7% were Class 4 (at least two-thirds of the root is engaging both the labial and palatal cortical plates: unfavorable or contraindicated for immediate placement).
A CBCT image is useful to evaluate the integrity of the existing facial bone.38-40 A Class 1 socket (no facial dehiscence or fenestrations) is most likely to have an excellent result without significant hard- or soft-tissue changes after immediate tooth replacement. However, some Class 2 (buccal dehiscence or bone loss) defects can be clinically present without associated gingival recession, which could represent complication risks for future recession.40
Assessing both the CBCT information and clinical parameters helps in developing a restoratively driven treatment plan. The final tooth position needs to be determined such that the planned SRP falls within the proposed tooth position with an emergence profile consistent with the appropriate 3D placement of the implant shoulder to avoid procedural placement errors. In cases in which the SRP and final tooth position cannot be correctly determined and achieved without staged augmentation procedures to develop an appropriate bone site, the immediate placement procedure should not be performed due to the high risk for developing a suboptimal result.3-5,38
Immediate implant placement should be considered in selected healthy patients and conducted by highly skilled clinicians with adequate clinical experience and expertise.6,38,41-44
3. Minimally Traumatic Tooth Extraction
Minimally invasive surgical techniques, including the use of anterior surgical forceps and elevators and aids to vertically extract a remaining fractured root, are available and highly recommended (Figure 6 and Figure 7). Overheating of the osteotomy site or trauma to adjacent soft-tissue papilla and socket walls should be avoided. If possible, a flapless procedure without any vertical releasing incisions is preferable. In addition, once the tooth is removed and the socket walls degranulated, creating multiple bleeding points in the socket is recommended to promote a more rapid vascularization of the graft material. Piezosurgical devices using copious amounts of sterile solution can be used for sectioning fractured roots and creating fine bleeding points.30,43 Confirmation of an intact buccal and palatal wall is necessary to proceed with immediate implant placement.
4. Platform-Switched Implant Along Palatal Wall
When immediate single-tooth implant placement is anticipated, a platform-switched implant is recommended8,13-15,38,43 (Figure 7 and Figure 8). Surgical placement should be completed with minimal trauma to the surrounding soft and hard tissues. The implant osteotomy point is directed along the palatal wall using an ACSGT to facilitate palatal or cingulum trajectory to enable (if practical) a screw-retained provisional restoration.
The buccal-lingual placement of the implant is critical to the final position of the facial gingival margin. Two studies45,46 evaluated facial soft-tissue recession and found a strong association between increased recession and a buccal position of the implant. Implants with a facially positioned shoulder showed three times more facial gingival recession than implants with a palatally positioned shoulder. The use of an ACSGT and manufacturer-specific bone profile drills (utilized along the palatal wall) aids the surgeon in maintaining the correct buccolingual position of the implant without the implant migrating facially during insertion.
Implant placement depth should be referenced from the anticipated final midfacial mucosal zenith of the planned final restoration. This will ensure that a gradual prosthetic emergence profile is developed that supports the peri-implant mucosa, is stable long term, and can be cleaned by the patient. If the coronal buccal wall is totally intact, the vertical position of the implant shoulder needs to be 1 mm apical to the buccal osseous crest to compensate for the average of 1 mm crestal loss that is normally seen. If bony undercuts are expected apical to the implant, then a tapered-design implant is recommended to avoid a buccal fenestration, which may be more likely to occur with a straight-walled design.47,48
Site preparation is performed using the manufacturer’s twist drills with copious irrigation with cold saline and completed employing an index finger for tactile sense along the buccal plate of bone to confirm no buccal vibration or fenestration.43 With good primary stability as measured by insertion torque greater than 35 Ncm or resonance frequency greater than ~65 RFI and favorable patient conditions and cooperation, an immediate provisional that is out of occlusal contact can be placed. Caution should be taken in placing an immediate provisional in a patient with significant parafunctional habits. Alternatively, a custom-contoured transmucosal healing abutment can be placed, which can be replaced with an esthetic provisional restoration following a conventional healing period of 2 to 3 months.7,11
5. Use of Narrower Implant
Treatment-planning decisions must be made prior to surgery based on CBCT analysis. Buccal bony-wall resorption should be expected following an immediate implant placement. This means that once the implant is inserted into the correct 3-dimensional position along the palatal wall, there should be at least a gap of 2 mm or more facial to the implant to the internal aspect of the buccal wall. This gap, once bone grafted, should be sufficient to prevent future midfacial mucosal recession. (Figure 7 and Figure 8). Often, a reduced-diameter implant affords additional buccal gap room to create a desired 2 mm to 3 mm of space for grafting.19,49,50 Using a wider-diameter implant (ie, ≥4.5 mm width) can have the negative effect of reducing the gap distance to the buccal plate to less than 2 mm to 3 mm and be responsible for future marginal gingival recession, especially if the implant is placed with buccal angulation.19,45,46 Reduced-diameter implants have narrower connections and require slightly deeper placement than standard-diameter implants (ie, 4.1 mm) to allow for the added room to create subgingival contours. Use of an ACSGT aids this critical 3D placement.
Smaller-diameter implants have less surface area than standard-diameter implants and may have correspondingly reduced primary stability. This also may contraindicate immediate provisionalization and should be considered in treatment planning.
The principle of using a reduced-diameter (3.3 mm) versus a standard-diameter (4.1 mm) immediately placed implant in conjunction with grafting the buccal gap with deproteinized bovine bone mineral (DBBM) was shown to promote new bone formation, and it enhanced the level of bone-to-implant contact in dogs.51 Covani et al52 also showed similar results in a dog model using 3.25-mm implants placed to the lingual. Vertical buccal bone resorption was only 0.05 mm51 compared to 2.5 mm in a study by Araújo et al53 in which wider-diameter (4.1 mm) implants were placed.
Chen and Buser31 suggested preparing the osteotomy palatally and avoiding oversized implants to reduce the risk for adverse esthetic outcomes for implants placed in immediate extraction sites. Rosa et al19 proposed a method for selecting the diameter of immediate implants and guiding the placement position of them based on the buccolingual dimension, with the goal of preserving the buccal bone wall. Using pre- and postoperative CBCT images, the socket buccolingual distance was measured to determine the appropriate implant diameter while considering a 3-mm gap to the buccal wall as the surgical goal. The authors suggested maintaining a 3-mm gap between the buccal bone surface of the implant and buccal bone wall offered predictable results in the stability and vascularization of the buccal plate (using tuberosity autogenous bone graft in the gap). In summary, positioning the implant along the palatal wall and maintaining a buccal gap of 2 mm to 3 mm, and possibly using reduced-diameter implants, may be important factors in reducing the rate of vertical and buccal bone resorption and subsequent facial gingival recession.
6. Bone Graft With Low-Substitution Bone Filler
Clinical studies using an immediate implant protocol (type 1 implant placement)2,3,6 in the esthetic zone strongly suggest bone augmentation of the buccal gap is necessary to achieve adequate buccal bony contours, assuming the minimum buccal bone width of 2 mm is valid (Figure 9). This approach will help maintain buccal bony-wall stability over time.7-12,15,16,19,30,38,43,45,46,54-56 When the surgeon is considering type 1 (immediate) implant placement the status of the facial bone should be evaluated for any preexisting defects, because this is a major risk factor for future facial mucosal recession.2-4,38,57 Kan et al57 studied the treatment of vertical buccal wall defects at the time of type 1 immediate implant placement and immediate provisionalization (IIPP). At 1 year, they observed 1.5 mm or greater of facial mucosal recession in more than one-third of the patients receiving treatment with bone grafting of the buccal wall vertical bony defects. The most facial recession noted in this study was when correspondingly larger facial bone defects were encountered. Notably, the study did not use platform-switched implants or other recommendations from the 10 keys mentioned herein, which may also have contributed to poor results.
Januario et al58 analyzed 250 CBCT scans and measured the facial-bone thickness in the anterior maxillae at 1 mm, 3 mm, and 5 mm from the bone crest in 250 patients. They found the bone thickness in almost all tooth sites examined was ≤1 mm thick (≤0.6 mm on average). They also noted in almost 50% of sites, the marginal (5 mm) portion of the wall was <0.5 mm wide. Based on these CBCT-scan studies, it may be concluded that once a maxillary anterior tooth is gone, not only may the entire marginal buccal bone wall be lost, but an additional 2 mm of the original socket dimension may also disappear during healing.34,58-60 Kan et al61 reported ongoing changes in the marginal tissue levels continued to occur up to 8.2 years (mean 4 years) after IIPP without grafting of the buccal gap or use of a subepithelial connective tissue graft (SCTG). In this study, thin biotypes receded three times more than thick biotypes. Four (11%) patients expressed esthetic concerns and were subsequently treated with hard- and soft-tissue grafting procedures to try to improve undesirable esthetic outcomes.
7. Palatal SCTG for ‘Biotype Conversion’
The last of the surgical keys is often overlooked. In their IIPP study (mean 4 years) of the esthetic zone without bone grafting the buccal gap or using a SCTG, Kan et al61 reported significantly greater facial gingival level (FGL) changes in the thin gingival biotype group (–1.50 mm) compared to the thick gingival biotype group (0.56 mm) (Figure 9 and Figure 10). This finding supported the results of 2 previously mentioned studies.45,46 Facial gingival recession is common after immediate tooth replacement. The amount of recession is approximately –0.5 mm to –0.8 mm of FGL.45,62,63,64 When SCTG was added to the IIPP protocol, no significant difference was observed in the FGL change at a mean follow-up of 2.15 years between thick (8 patients) and thin (12 patients) gingival biotypes (0.23 mm vs. 0.06 mm, respectively).65 This may suggest a thin gingival biotype can be converted to a thicker gingival biotype morphologically and behaviorally—thus the term “biotype conversion.” The mean mesial and distal marginal bone level changes and the mean FGL changes in this study also showed no significant differences at a mean follow-up of 2.15 years, demonstrating well-preserved peri-implant papilla.65 This agrees with a study by Fenner et al,66 in which cases that received SCTG (baseline facial tissue thickness of <2 mm) had stable papilla height after an observation time of 8 years, whereas the cases that did not obtain SCTG saw a decrease of the papilla between year 1 and year 8.
In a 1-year prospective study in nonesthetic sites in humans, Linkevicius et al67 found the initial gingival thickness at the alveolar crest may be considered a significant influence on marginal bone stability around implants. If the tissue thickness was 2.5 mm or less, crestal bone loss of up to 1.45 mm occurred within the first year of function, despite a supracrestal position of the implant–abutment interface. They also recommended thickening of thin mucosa before implant placement, converting a thin-tissue biotype into a thicker one.
The results of the study by Linkevicius et al67 are consistent with an animal study by Berglundh et al68 who reported the correlation of thin tissues with crestal bone loss during biologic width formation if a minimum dimension of the biologic width was not preexisting. Bone resorption would follow to allow for the reformation of the biologic width. Linkevicius et al69 found that platform switching in a 1-stage implant placement approach does not prevent crestal bone loss if, at the time of implant placement, mucosal tissue is thin (2 mm or less). However, in thick soft tissue (>2 mm), use of a platform-switch implant maintained crestal bone level with minimal remodeling at 1 year. In a 2-stage implant placement approach with a platform switch, Puisys et al70 found similar results. Thin tissues (≤2 mm) lost significant crestal bone, whereas thick tissues (>2 mm) or thin tissues augmented with acellular dermal matrix had similar crestal bone maintenance with minimal bone loss at 1 year.
The use of SCTG in conjunction with bone-grafting the implant–socket gap with IIPP in the esthetic zone and 3D placement has been evaluated in several other case studies.8,71-75 Rungcharassaeng et al74 examined the facial gingival tissue thickness (FGTT) with IIPP on maxillary anterior teeth with the placement of SCTG (n = 31) and without SCTG (n = 24). In a study by Jung et al,76 at 1.5 mm of gingival tissue thickness all materials tested (titanium, titanium-ceramic, zirconia-ceramic, and zirconia) caused visible tissue color change. It was determined that 3 mm of gingival thickness was necessary to sufficiently mask all test materials, while with 2-mm-thick gingival tissue, only zirconia did not induce visible color change using spectrophotometric analysis. In the study by Rungcharassaeng et al,74 patients who did not receive SCTG had a FGTT mean measurement of 1.42 mm, which seemed inadequate to mask any type of underlying restorative material, as Jung et al76 also noted. The mean for the SCTG cases was significantly greater at 2.61 mm. Rungcharassaeng et al74 concluded that performing IIPP in conjunction with a connective tissue graft will more likely result in sufficient peri-implant tissue thickness to conceal the underlying implant restorative materials compared to nongrafted sites.
Cosyn et al77 evaluated immediate screw-retained restorations in 22 patients who presented with thick gingival biotypes (patients with thin biotypes were excluded); the platform-switch concept was used with all implants. All implant–socket gaps were grafted with DBBM. At 3 months, 5 cases demonstrated alveolar process remodeling (1 mm or more) and received SCTG using the pouch technique. In addition, 2 cases showed advanced midfacial gingival recession (1.5 mm to 2 mm) and were also grafted with SCTG. Thus, 7 cases (31.8% of cases) were grafted at 3 months because of esthetic complications. SCTG use resulted in a steady improvement of the pink esthetic score (PES) after 3 months. The authors found similar PES post-treatment (PES: 11.86) compared to presurgery (PES: 12.15). They concluded preservation of pink esthetics is possible following immediate tooth replacement; however, to achieve this, SCTG is necessary in about one-third of the patients (who presented with a thick gingival biotype). Similarly, in the study by Chen et al,45 midfacial mucosa recession of 1 mm to 3 mm was noted in 10 (33%) of 30 sites within the first year.
Several recent clinical studies have shown highly acceptable esthetic outcomes resulting from grafting the buccal gap (freeze-dried cortical bone allograft or DBBM) without the use of SCTG. These sites were managed by preserving the gingival contours at the time of implant placement using a customized contoured healing abutment (polyether-ether-ketone [PEEK]) or a custom-contoured immediate provisional (IIPP) restoration for immediate support of the gingival tissues.7,9-19
To summarize, treatment strategies recommended to reduce the risk for facial mucosal recession when using type 1 implant placement include placing low-substitution bone fillers in the buccal gap, utilizing flapless surgery, using SCTGs, and immediately managing gingival contours at the time of immediate placement.
8. Management of Emergence Profile
Emergence profile management is performed with a flat or under-contoured customized anatomical screw-retained provisional restoration or a customizable PEEK abutment to mold and sculpt the soft tissues (ie, the transition zone) (Figure 11 through Figure 18). This first of the restorative-related keys begins with collecting patient data and treatment planning. After diagnosis, the team confers to generate a plan, which results in fabrication of an ACSGT to ensure correct tridimensional position of the dental implant. This is crucial in developing the transition zone with the provisional restoration.5,7,8,19-21,23,24,29,30,43,44 No clear advantage seems apparent for either screw retention or cement retention of the final restoration. The previously reported high incidence of screw loosening associated with older retention screw materials and external hexagon butt-joint designs has largely been resolved through the use of genuine (original equipment manufacturer) components, which have precise tolerance, control of machined interfaces, or internal connections.78,79 Cement retention can be associated with biologic/infection complications possibly because of operator error in controlling excess cement.80-88
Recommendation of a screw-retained restoration is based, in part, on the risk for excess cement potentially causing complications to adjacent tissues. A screw-retained provisional also facilitates the opportunity to apply pressure against the soft tissue when developing the transition zone during site optimization and tissue conditioning. As previously discussed, soft-tissue thickness around implants is important for long-term esthetic results. The shape of the provisional is fundamental in achieving good esthetics. The facial contour on the implant prosthesis can be quite different from that of a natural tooth. Undercontoured or flat facial design allows the soft tissue to occupy the space without pressure and proliferate coronally. Excessive or undesirable provisional pressure on the facial soft tissue can cause thinning of the mucosa and possible facial recession. The provisional can be adjusted to the correct height of the proposed mucosal margin without causing blanching of the tissue for a prolonged period (empirically 5 minutes). Typically, an immediate provisional will be initially undercontoured, and tissue maturation and shaping can be corrected after several appointments of adjustments (Figure 13 through Figure 18.).
The implant-retained provisional can be fabricated by either a direct method intraorally or an indirect method in the laboratory. With the indirect technique, a presurgical cast is modified after the intraoral index (impression) of the dental implant is made. Different abutment types, including titanium or PEEK, and materials—such as polymethyl-methacrylate (PMMA), bisphenol A-glycidyl methacrylate (bis-GMA), denture teeth, or the patient’s previous crown or tooth—can be used for fabrication of the provisional. Based on research, controlling the emergence contour in the esthetic zone has immediate benefits. This is most easily done with a screw-retained, custom-contoured abutment in unprovisionalized cases (Figure 11 and Figure 12) or a custom-contoured, screw-retained provisional (Figure 13 through Figure 18) when restored.
Use of the customized PEEK abutment allows the tissues to begin achieving the desired transition zone shape. This is done prior to insertion of a screw-retained, laboratory-processed provisional 12 weeks later (Figure 13 and Figure 14). This temporary titanium abutment usually needs to be adjusted to improve esthetics by opaquing the grayness of the titanium with a light-cured opaque resin material to prevent darkening the peri-implant mucosa. The provisional is shaped with the correct or undercontoured emergence profile, and the gingival embrasure is designed following the adjacent teeth even if a black triangle is present at insertion. The transition zone can be further modified with the provisional by adding or removing subgingival restorative material and allowing the gingiva to mature. Full papillary height may not be appreciated for several months following provisionalization.
Choquet et al89 showed when papilla is filling the space between an implant and a natural tooth, the average distance between the gingival portion of the proximal contact and the interproximal bone is approximately 3.8 mm. However, this number is merely an average of the patients in the study, and the papilla can be longer. The gingival embrasure ideally should be opened initially in the provisional to allow for papilla maintenance or regrowth. The provisional should eventually be reevaluated and a decision to close spaces or modify shapes should be considered. A provisional restoration in the esthetic zone may be worn for an extended period. Determining the optimal time to make a final impression for fabrication of the final restoration is a clinical decision, as interproximal tissues can continue to mature and increase in height for 1 year or longer.
9. Custom Impression Coping Technique
After the implant has osseointegrated and the clinicians are satisfied with the soft-tissue architecture and transition zone that has materialized in the provisional phase, the position of the implant and transition zone is communicated to the laboratory technician (Figure 19 through Figure 23). Once the provisional is removed, the tissue noticeably collapses immediately due to the circular peri-implant connective tissue fibers. In almost all esthetic-zone cases, a stock impression coping will not prevent the soft tissues from collapsing, nor will it hold the tissues in a proper shape. This prevents the transition zone from being duplicated accurately. Under these conditions, the laboratory technician will design the emergence profile according to his or her knowledge of the dental anatomy.
To provide the technician with an accurate representation of the transition zone and avoid having to estimate its shape, Hinds90 proposed a technique to produce a custom impression coping. Patras and Martin91 modified the technique by using photopolymerizing materials such as flowable composites. The provisional restoration contains the developed transition zone shape and, by default, the support for the transition zone (Figure 17 and Figure 18). A polyvinyl siloxane (PVS) material is used to copy the shape of the provisional on an implant analog (Figure 19 and Figure 20). Once the material is set, the provisional is removed from the analog and the stock impression coping (open tray or closed tray) is adapted to the analog. The space between the impression coping and the PVS (ie, the transition zone) is filled with flowable composite and light cured. The custom impression coping is then removed from the analog and placed in the implant site intraorally. The custom impression coping now supports the surrounding tissues identically to the provisional for the final impression92 (Figure 20 and Figure 21). Once the impression is removed, an analog is attached to the impression coping and a soft-tissue model is made (Figure 22 and Figure 23).
10. Final Restoration
The restorative doctor and/or dental laboratory have many materials from which to choose for laboratory fabrication of the final implant restoration (Figure 24 through Figure 29). Historically, ceramic fused to metal utilizing a “cast to” abutment has shown excellent long-term results and superb esthetics. Dentistry’s pursuit of even more predictable esthetics and greater manufacturing efficiencies has led to metal-free restorations and milled ceramic/titanium abutments.
Concerns regarding zirconia abutments with titanium implant interfaces focus on long-term survival and possible complications, including fracture of zirconia at the titanium implant connection and wear of the titanium walls of the implant adjacent to the abutment. The wear can result in micromovement of the abutment connection and eventual fracture of the zirconia abutment or tattooing of the soft tissues due to fretting.93 This complication can be avoided by using a titanium bonding base, which provides a titanium interface in contact with the dental implant and a retention portion for cementation of a ceramic abutment complex. This can be accomplished with the “Ti base” concept, whereby a titanium interface connection is milled in titanium (as in our case presentation) as a one-piece abutment, and the ceramic crown is cemented extraorally by the laboratory, and then screwed into place intraorally (“screw-ment” design). Alternatively, the abutment can be milled in zirconia and bonded to the Ti base. If done as a zirconia abutment, porcelain can be applied directly, thereby avoiding cementing the crown to the abutment. The firing of the porcelain would be performed before bonding to the Ti base.
When using final restorations that are cemented on custom abutments intraorally, there is no statistical difference in success for single-unit restorations. Clinicians should be aware of the risk for excess cement being left subgingivally due to the inability to detect or remove cement at tissue depths greater than 1 mm.83-88 Linkevicius et al84 demonstrated how difficult it can be to remove excess cement when the abutment margins are subgingival.
To avoid these clinical situations, a correct 3D custom abutment should be fabricated. The contours should follow the gingival margins equal to or no more than 1 mm subgingival. Also, when cementing is necessary, the amount of excess cement must be controlled.85-88 Resin and other radiolucent cements should be avoided because excess cement cannot be detected radiographically and because of the bacteriophyllic properties of the material. In addition, removing resin cement can be difficult due to the formation of a thin layer subgingivally along the abutment interface. Radiopaque cements, such as those containing zinc, are recommended for their ability to be seen radiographically and their bacteriostatic properties.86,88
Conclusions
The 10 keys for esthetic-zone success for single immediate implants are intended to be a guide for clinicians and aid them in the treatment planning and execution of these types of cases. Each key can be critical in achieving the final, predictable long-term esthetic outcome. Treatment in the esthetic zone is a complex SAC procedure for both the surgical phase (key Nos. 3 through 7) and prosthetic phase (key Nos. 8 through 10); therefore, the team approach should be considered when treatment planning in the esthetic zone.
Keys that have emerged in the past few years for immediate placement of implants at the time of extraction include: treatment planning, including facial buccal bone assessment and recognition and management based on the sagittal position of the tooth to be extracted using CBCT analysis; palatal placement of the implant leaving a 2-mm to 3-mm gap between the facial surface of the implant and the buccal plate; use of smaller-diameter implants to leave a larger buccal gap; placement of a mineralized bone graft in the buccal gap; placement of SCTG with a small envelope or tunneling incision facial to the buccal plate to compensate for anticipated buccal remodeling (this is particularly important for patients with thin- or medium-thickness gingival phenotype); and immediate contour preservation with either a custom provisional restoration or a custom healing abutment.
More traditional keys include: dedication to a team approach with open communication and each member having expertise in his or her own therapeutic area and knowledge of other aspects of treatment; optimization of the subgingival contours with accurate provisional restorations; accurate transfer of contours to the dental laboratory using a customized impression coping; and selection of final restorative materials and techniques recognizing possible limitations and complications of implant–abutment interfaces, cementation issues, and biologic parameters.
Short- and medium-term studies now show equivalent results between immediate placement and provisionalization compared with delayed placement with conventional healing when the 10 keys are followed.7-19,38,94 Long-term studies are needed that compare the procedures for optimal timing of implant placement in the esthetic zone, because contour changes of the soft and hard tissues may continue for many years post-implant placement.38,61
About the Authors
Robert A. Levine, DDS
Clinical Professor in Periodontology and Implantology
Kornberg School of Dentistry
Temple University
Philadelphia, Pennsylvania
Diplomate
American Board of Periodontology
Fellow
International Team for Implantology
Private Practice in Dental Implants and Periodontics
Philadelphia, Pennsylvania
Jeffrey Ganeles, DMD
Adjunct Associate Professor
Nova Southeastern University College of Dental Medicine
Ft. Lauderdale, Florida
Diplomate
American Board of Periodontology
Fellow
International Team for Implantology
Fellow, Academy of Osseointegration
Private Practice in Dental Implants and Periodontics
Boca Raton, Florida
Luiz Gonzaga, DDS, MS
Center for Implant Dentistry
University of Florida
Gainesville, Florida
Fellow
International Team for Implantology
Joseph K. Kan, DDS, MS
Professor and Private Practice
Prosthodontics and Implant Dentistry
Loma Linda University School of Dentistry
Loma Linda, California
Harry Randel, DMD
Private Practice in Prosthodontics and Implant Dentistry
Philadelphia, Pennsylvania
Fellow
International Team for Implantology
Chris D. Evans, BDSc, MDSc, MRACDS
Private Practice in Prosthodontics and Implant Dentistry
Brighton, Australia
Fellow
International Team for Implantology
Stephen T. Chen, BDS, MDSc, PhD, FRACDS
Clinical Associate Professor
University of Melbourne
Melbourne, Australia
Fellow
International Team for Implantology
Private Practice in Dental Implants and Periodontics
Melbourne, Australia
References
1. Dawson A, Chen S. The SAC Classification in Implant Dentistry. Berlin: Quintessence Publishing; 2009.
2. Morton D, Ganeles J. ITI Treatment Guide. Vol 2. Loading Protocols in Implant Dentistry - Partially Dentate Patients. Berlin: Quintessence Publishing; 2007.
3. Chen ST, Buser D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla—a systematic review. Int J Oral Maxillofac Implants. 2014;29(suppl):186-215.
4. Levine RA, Huynh-Ba, Cochran DL. Soft tissue augmentation procedures for mucogingival defects in esthetic sites. Int J Oral Maxillofac Implants. 2014;29(suppl):155-185.
5. Morton D, Chen ST, Martin WC, et al. Consensus statements and recommended clinical procedures regarding optimizing esthetic outcomes in implant dentistry. Int J Oral Maxillofac Implants. 2014;29(suppl):216-220.
6. Chen ST, Beagle J, Jensen SS, et al. Consensus statements and recommended clinical procedures regarding surgical techniques. Int J Oral Maxillofac Implants. 2009;24(suppl):272-278.
7. Tarnow DP, Chu SJ, Salama MA, et al. Flapless postextraction socket implant placement in the esthetic zone: part 1. The effect of bone grafting and/or provisional restoration on the facial-palatal ridge dimensional change—a retrospective cohort study. Int J Periodontics Restorative Dent. 2014;34(3):323-331.
8. Yoshino S, Kan JY, Rungcharassaeng K, et al. Effects of connective tissue grafting on the facial gingival level following single immediate implant placement and provisionalization in the esthetic zone: a 1-year randomized controlled prospective study. Int J Oral Maxillofac Implants. 2014;29(2):432-440.
9. Lee EA, Gonzalez-Martin O, Fiorellini J. Lingualized flapless implant placement into fresh extraction sockets preserves buccal alveolar bone: a cone beam computed tomography study. Int J Periodontics Restorative Dent. 2014;34(1):61-68.
10. Morimoto T, Tsukiyama Y, Morimoto K, Koyano K. Facial bone alterations on maxillary anterior single implants for immediate placement and provisionalization following tooth extraction: a superimposed cone beam computed tomography study. Clin Oral Implants Res. 2015;26(12):1383-1389.
11. Chu SJ, Salama MA, Garber DA, et al. Flapless postextraction socket implant placement, Part 2: The effects of bone grafting and provisional restoration on peri-implant soft tissue height and thickness—a retrospective study. Int J Periodontics Restorative Dent. 2015;35(6):803-809.
12. Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L. Soft tissue contour changes at immediate postextraction single-tooth implants with immediate restoration: a 12-month prospective cohort study. Int J Periodontics Restorative Dent. 2015;35(2):191-198.
13. Aguilar-Salvatierra A, Calvo-Guirado JL, Gonzalez-Jaranay M, et al. Peri-implant evaluation of immediately loaded implants placed in esthetic zone in patients with diabetes mellitus type 2: a two-year study. Clin Oral Implants Res. 2016;27(2):156-161.
14. Cooper LF, Reside GL, Raes F, et al. Immediate provisionalization of dental implants placed in healed alveolar ridges and extraction sockets: a 5-year prospective evaluation. Int J Oral Maxillofac Implants. 2014;29(3):709-717.
15. Ross SB, Pette GA, Parker WB, Hardigan P. Gingival margin changes in maxillary anterior sites after single immediate implant placement and provisionalization: a 5-year retrospective study of 47 patients. Int J Oral Maxillofac Implants. 2014;29(1):127-134.
16. Saito H, Chu SJ, Reynolds MA, Tarnow DP. Provisional restorations used in immediate implant placement provide a platform to promote peri-implant soft tissue healing: a pilot study. Int J Periodontics Restorative Dent. 2016;36(1):47-52.
17. Barone A, Titi P, Quarata A, et al. The clinical outcomes of immediate versus delayed restoration procedures on immediate implants: a comparative cohort study for single-tooth replacement. Clin Implant Dent Relat Res. 2015;17(6):1114-1126.
18. Barone A, Marconcini S, Giammarinaro E, et al. Clinical outcomes of implants placed in extraction sockets and immediately restored: a 7-year single-cohort prospective study. Clin Impl Dent Relat Res. 2016;18(6):1103-1112.
19. Rosa AC, da Rosa JC, Dias Pereira LA, et al. Guidelines for selecting the implant diameter during immediate implant placement of a fresh extraction socket: a case series. Int J Periodontics Restorative Dent. 2016;36(3):401-407.
20. Belser UC, Schmid B, Higginbottom F, Buser D. Outcome analysis of implant restorations located in the anterior maxilla: A review of the recent literature. Int J Oral Maxillofac Implants. 2004;19(suppl):30-42.
21. Morton D, Martin WC, Ruskin JD. Single-stage Straumann dental implants in the aesthetic zone: considerations and treatment procedures. J Oral Maxillofac Surg. 2004;62(9 suppl 2):57-66.
22. Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2001;22(3):199-206.
23. Levine RA, Katz D. Developing a team approach to complex aesthetics: treatment considerations. Prac Proced Aesthet Dent. 2003;15(4):301-306.
24. Funato A, Salama MA, Ishikawa T, et al. Timing, positioning, and sequential staging in esthetic implant therapy: a four-dimensional perspective. Int J Periodontics Restorative Dent. 2007;27(4):313-323.
25. Bornstein MM, Balsiger R. Sendi P, von Arx T. Morphology of the nasopalatine canal and dental implant surgery: a radiographic analysis of 100 consecutive patients using limited cone-beam computed tomography. Clin Oral Implants Res. 2011;22(3):295-301.
26. Scarfe W, Vaughn WS, Farman AG, et al. Comparison of restoratively projected and surgically acceptable virtual implant position for mandibular overdentures. Int J Oral Maxillofac Implants. 2012;27(1):111-118.
27. Daftary F, Mahallati R, Bahat O, Sullivan RM. Lifelong craniofacial growth and the implications for osseointegrated implants. Int J Oral Maxillofac Implants. 2012;28(1):163-169.
28. Levine R, Martin W. Esthetic risk assessment in implant dentistry. Inside Dent. 2012;8(8):66-71.
29. Martin W, Morton C, Buser D. Preoperative analysis and prosthetic treatment planning in esthetic implant dentistry. In: Buser D, Belser U, Wismeijer D, eds. ITI Treatment Guide. Vol 1. Implant Therapy in the Esthetic Zone - Single-Tooth Replacements. New Malden, Surrey, UK: Quintessenz Verlag; 2007;1:9-24.
30. Levine RA, Nack G. Team treatment planning for the replacement of esthetic zone teeth with dental implants. Compend Contin Educ Dent. 2011;32(4):44-50.
31. Chen S, Buser D. Advantages and disadvantages of treatment options for implant placement in post-extraction sockets. In: Buser D, Wismeijer D, Belser U, eds. ITI Treatment Guide. Vol. 3. Implant Placement in Post-Extraction Sites: Treatment Options. Berlin: Quintessenz Verlag: 2008:29-42.
32. Salama H, Salama M. The role of orthodontic extrusion remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: a systematic approach to the management of extraction site defects. Int J Periodontics Restorative Dent. 1993;13(4):312-333.
33. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19(suppl):43-61.
34. Huynh-Ba G, Pjetursson BE, Sanz M, et al. Analysis of the socket bone wall dimensions in the upper maxilla in relation to immediate implant placement. Clin Oral Implants Res. 2010;21(1):37-42.
35. Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000;5(1):119-128.
36. Kan JY, Roe P, Rungcharassaeng K, et al. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2011;26(4):873-876.
37. Buser D, Wittneben J, Bornstein MM, et al. Stability of contour augmentation and esthetic outcomes of implant-supported single crowns in the esthetic zone: 3-year results of a prospective study with early implant placement postextraction. J Periodontol. 2011;82(3):342-349.
38. Buser D. Chappuis V. Belser UC, Chen S. Implant placement post-extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol 2000. 2017;73(1):84-102.
39. Elian N. Cho SC, Froum S, et al. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-104.
40. Chu SJ, Sarnachiaro GO, Hochman MN, Tarnow DP. Subclassification and clinical management of extraction sockets with labial dentoalveolar dehiscence defects. Compend Contin Educ Dent. 2015;36(7):516-522.
41. Chen ST, Wilson TG Jr, Hammerle CH. Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. Int J Oral Maxillofac Implants. 2004;19 suppl:12-25.
42. Hämmerle CH, Chen ST, Wilson TG Jr. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants. 2004;19 suppl:26-28.
43. Levine RA. Surgical and prosthetic treatment of a failed maxillary central incisor. Inside Dent. 2016;12(6):64-70.
44. Ganeles J, Wismeijer D. Early and immediately restored and loaded dental implants for single-tooth and partial-arch applications. Int J Oral Maxillofac Implants. 2004;19(suppl):92-102.
45. Chen ST, Darby IB, Reynolds EC. A prospective clinical study of non-submerged immediate implants: clinical outcomes and esthetic results. Clin Oral Implants Res. 2007;18(5):552-562.
46. Evans CD, Chen ST. Esthetic outcomes of immediate implant placements. Clin Oral Implants Res. 2008;19(1):73-80.
47. Advanced surface and material enable Straumann’s bone level implants to overcome placement challenges. Compend Contin Educ Dent. 2015;36(8):628.
48. Kan JY, Roe P, Rungcharassaeng K. Effects of implant morphology on rotational stability during immediate implant placement in the esthetic zone. Int J Oral Maxillofac Implants. 2015;30(3):667-670.
49. Al-Nawas B, Brägger U, Meijer HJ, et al. A double-blind randomized controlled trial (RCT) of titanium-13 zirconium versus titanium grade IV small-diameter bone level implants in edentulous mandibles—results from a 1-year observation period. Clin Implant Dent Relat Res. 2012;14(6):896-904.
50. Levine RA, Gallucci GO. Implantology: an evolving dental discipline. Compend Contin Educ Dent. 2011;32(7):70-71.
51. Araújo MG, Linder E, Lindhe J. Bio-Oss collagen in the buccal gap at immediate implants: a 6-month study in the dog. Clin Oral Implants Res. 2011:22(1):1-8.
52. Covani U, Cornelini R, Calvo JL, et al. Bone remodeling around implants placed in fresh extraction sockets. Int J Periodontics Restorative Dent. 2010;30(6):601-607.
53. Araújo MG, Sukekava F, Wennström JL, Lindhe J. Tissue modeling following implant placement in fresh extraction sockets. Clin Oral Implants Res. 2006;17(6):615-624.
54. Sanz M, Cecchinato D, Ferrus J, et al. A prospective, randomized-controlled clinical trial to evaluate bone preservation using implants with different geometry placed into extraction sockets in the maxilla. Clin Oral Implants Res. 2010;21(1):13-21.
55. Sanz M, Lindhe J, Alcaraz J, et al. The effect of placing a bone replacement graft in the gap at immediately placed implants: a randomized clinical trial [published online ahead of print June 7, 2016]. Clin Oral Implants Res. doi:10.1111/clr.12896.
56. Abdelhamid A, Omran M, Bakhshalian N, et al. An open randomized controlled clinical trial to evaluate ridge preservation and repair using SocketKAP™ and SocketKAGE™: part 2 – three-dimensional alveolar bone volumetric analysis of CBCT imaging. Clin Oral Implants Res. 2016;27(6):631-639.
57. Kan JY, Rungcharassaeng K, Sclar A, Lozada JL. Effects of the facial osseous defect morphology on gingival dynamics after immediate tooth replacement and guided bone regeneration: 1-year results. J Oral Maxillofac Surg. 2007;657(suppl 1):13-19.
58. Januario AL, Duarte WR, Barriviera M, et al. Dimension of the facial bone wall in the anterior maxilla: a cone-beam computed tomography study. Clin Oral Implants Res. 2011;22(10):1168-1171.
59. Miyamoto Y, Obama T. Dental cone beam computed tomography analyses of postoperative labial bone thickness in maxillary anterior implants: comparing immediate and delayed implant placement. Int J Periodontics Restorative Dent. 2011;31(3):215-225.
60. Braut V, Bornstein M, Belser U, Buser D. Thickness of the anterior maxillary facial bone wall—a retrospective radiographic study using cone beam computed tomography. Int J Periodontics Restorative Dent. 2011;31(2):125-131.
61. Kan JY, Rungcharassaeng K, Lozada JL, Zimmerman G. Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants: a 2- to 8-year follow-up. Int J Oral Maxillofac Implants. 2011;26(1):179-187.
62. Kan JY, Rungcharassaeng K, Lozada J. Immediate placement and provisionalization of maxillary anterior single implants: 1-year prospective study. Int J Oral Maxillofac Implants. 2003;18(1):31-39.
63. De Rouck T, Collys K, Cosyn J. Immediate single-tooth implants in the anterior maxilla: a 1-year case cohort study on hard and soft tissue response. J Clin Periodontol. 2008;35(7):649-657.
64. Cosyn J, De Bruyn H, Cleymaet R. Soft tissue preservation and pink aesthetics around single immediate implant restorations: a 1-year prospective study. Clin Implant Dent Relat Res. 2013;15(6):847-857.
65. Kan JY, Rungcharassaeng K, Morimoto T, Lozada J. Facial gingival stability after connective tissue graft with single immediate tooth replacement in the esthetic zone: consecutive case reports. J Oral Maxillofac Surg. 2009;67(11 suppl):40-48.
66. Fenner N, Hämmerle CH, Sailer I, Jung RE. Long-term clinical, technical, and esthetic outcomes of all-ceramic vs. titanium abutments on implant supporting single-tooth reconstructions after at least 5 years. Clin Oral Implants Res. 2016;27(6):716-723.
67. Linkevicius T, Apse P, Grybauskas S, Puisys A. The influence of soft tissue thickness on crestal bone changes around dental implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants. 2009;24(4):712-719.
68. Berglundh T, Abrahamsson I, Welander M, et al. Morphogenesis of the peri-implant mucosa: an experimental study in dogs. Clin Oral Implants Res. 2007;18(1):1-8.
69. Linkevicius T, Puisys A, Steigmann M, et al. Influence of vertical soft tissue thickness on crestal bone changes around implants with platform switching: a comparative clinical study. Clin Implant Dent Relat Res. 2015;17(6):1228-1236.
70. Puisys A, Vindasiute E, Linkevciene L, Linkevicius T. The use of acellular dermal matrix membrane for vertical soft tissue augmentation during submerged implant placement: a case series. Clin Oral Implants Res. 2015;26(4):465-470.
71. Redemagni M, Cremonesi S, Garlini G, Maiorna C. Soft tissue stability with immediate implants and concave abutments. Eur J Esthet Dent. 2009;4(4):328-337.
72. Chung S, Rungcharassaeng K, Kan JY, et al. Immediate single tooth replacement with subepithelial connective tissue graft using platform switching implants: a case series. J Oral Implantol. 2011;37(5):559-569.
73. Tsuda H, Rungcharassaeng K, Kan JY, et al. Peri-implant tissue response following connective tissue and bone grafting in conjunction with immediate single-tooth replacement in the esthetic zone: a case series. Int J Oral Maxillofac Implants. 2011;26(2):427-436.
74. Rungcharassaeng K, Kan JY, Yoshino S, et al. Immediate implant placement and provisionalization with and without a connective tissue graft: an analysis of facial gingival tissue thickness. Int J Periodontics Restorative Dent. 2012;32(6):657-663.
75. Grunder U. Crestal ridge width changes when placing implants at the time of tooth extraction with and without soft tissue augmentation after a healing period of 6 months: report of 24 consecutive cases. Int J Periodontics Restorative Dent. 2011;31(1):9-17.
76. Jung RE, Sailer I, Hämmerle CH, et al. In vitro color changes of soft tissues caused by restorative materials. Int J Periodontics Restorative Dent. 2007;27(3):251-257.
77. Cosyn J, De Bruyn H, Cleymaet R. Soft tissue preservation and pink aesthetics around single immediate implant restorations: a 1-year prospective study. Clin Implant Dent Relat Res. 2013;15(6):847-857.
78. Henry PJ, Laney WR, Jemt T, et al. Osseointegrated implants for single-tooth replacement: a prospective 5-year multicenter study. Int J Oral Maxillofac Implants. 1996:11(4):450-455.
79. Binon PP, McHugh MJ. The effect of eliminating implant/abutment rotational misfit on screw joint stability. Int J Prosthodont. 1996;9(6):511-519.
80. Gotfredsen K, Wiskott A, Working Group 4. Consensus report - reconstructions on implants. The Third EAO Consensus Conference 2012. Clin Oral Implants Res. 2012;23(suppl 6):238-241.
81. Martin WC, Pollini A, Morton D. The influence of restorative procedures on esthetic outcomes in implant dentistry: a systematic review. Int J Oral Maxillofac Implants. 2014;29 (suppl):142-154.
82. Wittneben JG, Millen C, Brägger U. Clinical performance of screw- versus cement-retained fixed implant-supported reconstructions—a systematic review. Int J Oral Maxillofac Implants. 2014;29(suppl):84-98.
83. Wilson TG Jr. The positive relationship between excess cement and peri-implant disease: a prospective clinical endoscopic study. J Periodontol. 2009;80(9):1388-1392.
84. Linkevicius T, Vindasiute E, Puisys A, Peciuliene V. The influence of margin location on the amount of undetected cement excess after delivery of cement-retained implant restorations. Clin Oral Implants Res. 2011;22(12):1379-1384.
85. Wadhwani C, Piñeryo A. Technique for controlling the cement for an implant crown. J Prosthet Dent. 2009;102(1):57-58.
86. Present S, Levine RA. Techniques to control or avoid cement around implant-retained restorations. Compend Contin Educ Dent. 2013;34(6):432-437.
87. Piñeyro A, Ganeles J. Custom abutments alone will not eliminate the clinical effects of poor cementation techniques around dental implants. Compend Contin Educ Dent. 2014;35(9):678-686.
88. Pette GA, Ganeles J, Norkin FJ. Radiographic appearance of commonly used cements in implant dentistry. Int J Periodontics Restorative Dent. 2013;33(1):61-68.
89. Choquet V, Hermans M, Andriaenssens P, et al. Clinical and radiographic evaluation of the papilla level adjacent to single-tooth dental implants. A retrospective study in the maxillary anterior region. J Periodontol. 2001;72(10):1364-1371.
90. Hinds KF. Custom impression coping for an exact registration of the healed tissue in the esthetic implant restoration. Int J Periodontics Restorative Dent. 1997;17(6):584-591.
91. Patras M, Martin W. Simplified custom impression post for implant-supported restorations. J Prosthet Dent. 2016;115(5):556-559.
92. Fürhauser R, Mailath-Pokorny G, Haas R, et al. Immediate restoration of immediate implants in the esthetic zone of the maxilla via the copy-abutment technique: 5-year follow-up of pink esthetic scores. Clin Implant Dent Relat Res. 2017;19(1):28-37.
93. Taylor TD, Klotz MW, Lawton RA. Titanium tattooing associated with zirconia implant abutments: a clinical report of two cases. Int J Oral Maxillofac Implants. 2014;29(4):958-960.
94. Mangano FG, Mastrangelo P, Luongo F, et al. Aesthetic outcome of immediately restored single implants placed in extraction sockets and healed sites of the anterior maxilla: a retrospective study on 103 patients with 3 years of follow-up. Clin Oral Impl Res. 2017;28(3):272–282.