You must be signed in to read the rest of this article.
Registration on AEGIS Dental Network is free. Sign up today!
Forgot your password? Click Here!
Six-Year Follow-Up of Immature Tooth Revascularization With Enamel Matrix Proteins
Neidy S. Corredor Gerber, DDS; Beatriz S. Coelho, MS; Tatiana M. Deliberador, PhD; Darlan R Junior, DDS; Flares Baratto-Filho, PhD; Fernando Luis Esteban Florez, PhD; João C. Zielak, PhD; and Denise P. Leonardi, PhD
ABSTRACT
Novel endodontic revascularization techniques have been considered as alternative options for treatment of immature teeth affected by apical periodontitis. The continuous development of the root canal has been recognized as a major advantage of these techniques over traditional apexification approaches. This article reports a case in which endodontic revascularization using extracellular matrix proteins (EMPs) as a scaffold was utilized to treat an immature maxillary lateral incisor with history of trauma and chronic apical periodontitis. The root canal was accessed and sequentially irrigated with sodium hypochlorite (NaOCl) (2 mL, 5.25%), saline solution (10 mL), and gluconate chlorhexidine (10 mL, 0.12%). The root canal was then dried, filled with an antibiotic paste (ciprofloxacin, metronidazole, and minocycline), and sealed for 3 weeks. The antibiotic paste was then removed by irrigating the canal with NaOCl (10 mL, 5.25%). The intracanal scaffold was obtained by injecting a commercially available enamel EMP into the newly formed intracanal blood clot. Mineral trioxide aggregate was used to seal the scaffold in place, and a composite resin restoration was then placed using a universal restorative. At 3 and 72 months, clinical and radiographic analyses demonstrated short- and long-term success of the technique presented. The authors' findings indicate revascularization techniques are promising in the treatment of immature teeth with apical periodontitis. Longitudinal clinical trials are necessary to confirm the findings reported herein.
Despite the dental profession's best efforts, the endodontic treatment of necrotic teeth with incomplete apexes remains a challenge. Typically, the prognoses for these types of treatments are inconsistent and unpredictable due to inefficiencies during the shaping, cleaning, and obliteration steps. These difficulties are mainly associated with the presence of very thin dentin walls and underdeveloped apexes that allow for the extrusion of large volumes of obliterating materials.1,2
Traditionally, clinicians have performed endodontic treatments of necrotic immature teeth using apexification techniques with either calcium hydroxide (Ca(OH)2) or mineral trioxide aggregate (MTA), with the objective of creating a dentinal barrier. Though such techniques have been shown to have adequate success rates, major limitations have been reported in recent years, including long-term application of Ca(OH)2, hydroxide-mediated reduction in root strength, and incomplete root formation.3 According to Cvek, the frequency of cervical root fractures in immature teeth during or after treatment is 28% to 77% higher than the frequency of fracture observed on fully developed teeth.4
These limitations have precipitated the development of modern pulp revascularization techniques. The primary purpose of these regenerative treatments is to allow for root canal development, thereby decreasing the chances of fractures and extrusion of obliterating materials to the periapical regions, with the goal of enabling a more controlled and reliable treatment prognosis.5 The underlying mechanism of these treatments is based on the use of hydrophobic proteins of enamel known as "amelogenins." These proteins have the capacity to promote extracellular matrix formation with a potential to support cells in adjacent tissues. Such action was demonstrated to be amplified in periapical regions due to blood supplies rich in stem cells displaying the necessary potential to drive the so-desired regenerative response.6 According to its manufacturer, Emdogain® (Straumann, straumann.com) is capable of reproducing the biological processes associated with tooth development, because it forms an insoluble 3-dimensional extracellular matrix that remains in close contact with surfaces along the root canal and the periodontal defect, thereby allowing for the colonization, proliferation, and differentiation of healthy cells.7 In addition, amelogenins were demonstrated to stimulate the growth of cells present in tissues of mesenchymal origin (eg, connective, cartilage, and bone), which suggests a strong potential for the utilization of these proteins in different areas of dentistry.8
The objective of the present study was to report a 6-year follow-up clinical case where endodontic revascularization with extracellular matrix proteins (EMPs) as a scaffold was used to treat an immature maxillary central incisor with history of trauma and chronic apical periodontitis.
Case Report
The patient was a 10-year-old girl who was referred to the Endodontics Clinic of the Positivo University (Curitiba, PR, Brazil) for the evaluation of a fractured maxillary lateral incisor (tooth No. 7). The patient's major complaint was the presence of a coronal fracture that resulted from a bicycling accident 2 years before the initial clinical evaluation. Anamnesis (ie, recollection) procedures were performed in the presence of the patient's legal guardian (mother) and revealed that the patient did not perceive pain symptoms at the time of the trauma or in subsequent years.
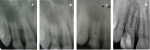
General and detailed clinical examination revealed a healthy and asymptomatic patient who displayed a coronal fracture of the maxillary lateral incisor (tooth No. 7) without the presence of pulp exposure, caries lesion, or discoloration. Vitality testing (Endo-Ice, Maquira, maquira.com.br) revealed that the tooth was non-vital due to a negative response to cold stimulus (~ -50°C). Subsequent radiographic analysis demonstrated that the tooth in question had an incomplete root apex that was surrounded by a radiolucent and diffuse image. Such radiographic finding suggested the presence of a periapical lesion (Figure 1) that was then diagnosed as chronic apical periodontitis. Because the tooth displayed incomplete risogenesis, along with chronic apical periodontitis, the treatment plan called for the use of an endodontic revascularization technique following the protocol published by Banchs and Trope.9 The advantages and limitations of the proposed technique were explained to the patient's legal guardian, who accepted the treatment terms and provided signed consent.
The treatment protocol used in the present study comprises three clinical sessions. In the first session, an access cavity was created and the presence of a necrotic pulp was confirmed. The root canal was gently irrigated with sodium hypochlorite (NaOCl) (2 mL, 5.25%, 3 mm below apex), and the necrotic pulp tissue was passively removed using a hand k-file (#50, Dentsply Maillefer, dentsplymaillefer.com). The root canal was then sequentially irrigated with NaOCl (10 mL, 5.25%), saline solution (10 mL), and gluconate chlorhexidine (10 mL, 0.12%), and dried using sterile paper points. A Lentulo bur (#40, Dentsply Maillefer) was then used to completely fill the root canal with an antibiotic paste containing ciprofloxacin, metronidazole, and minocycline. The access cavity was sealed with intermediate restorative material (Cavit™, 3M ESPE, 3m.com).
Three weeks later the patient returned, and tooth No. 7 was asymptomatic with no edema or fistula. Anesthetic procedures were performed using 3% mepivacaine (DFL, novadfl.com.br) without vasoconstrictor. This type of anesthetic is recommended in cases of endodontic revascularization, because the resultant blood flow in the root canal and periapical regions is adequate to form a clot that will drive the neo-formation of tissues.10 Tooth No. 7 was isolated with rubber dam. The access cavity was opened, and the triple antibiotic paste was removed from the canal by irrigation with 10 mL of 5.25% NaOCl. A #40 hand k-file was used to radiographically determine the total tooth length. To stimulate bleeding into the root canal, the #40 hand k-file was introduced into the periapical tissues. After bleeding occurred, the EMPs (Emdogain) were placed into the root canal as a structural matrix (ie, scaffold). The crown was cleaned and a paste of MTA (Angelus, angelusdental.com) was carefully placed into the canal 3 mm below the cementoenamel junction using an amalgam carrier, followed by use of a wet cotton pellet, and the access was sealed with glass-ionomer cement (Figure 2).
Three months later a clinical and radiographic assessment was conducted. The patient reported symptoms of slight sensitivity when tooth No. 7 was exposed to either hot or cold stimuli from beverages. Such sensitivity was confirmed by cold temperature testing using Endo-Ice. It was observed that tooth No. 7 was displaying moderately dark discoloration that was not associated with the presence of edema, fistula, or symptoms of pain. Percussion (vertical and horizontal) and palpation tests (apical region) resulted negative. Radiographic assessment at 3 months (Figure 3) demonstrated radiolucent areas that were significantly smaller when compared with those observed in the initial radiograph (Figure 1) of the case. Such radiographic findings suggest effective management of the apical periodontitis.
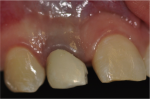
At the 6-year (72-month) follow-up clinical evaluation, tooth No. 7 was observed to display discoloration levels that were comparable to those observed at the 3-month evaluation. Further examination resulted negative for edema, fistula, percussion, and palpation tests, whereas vitality tests using Endo-Ice resulted positive. Radiographic assessment indicated the maintenance of dentin wall dimensions (height and thickness) (Figure 4). Cone-beam computed tomography (CBCT) assessment was performed to further evaluate the periapical regions of bone (Figure 5 and Figure 6). Clinically, the tooth and gingival region displayed significant darkening at 72 months (Figure 7). To resolve the gingival discoloration a subepithelial connective graph was placed at the cervical region of the tooth to increase gingival thickness while decreasing local color alteration. Figure 8 illustrates the clinical aspect of cervical gingival tissues 3 months after periodontal surgery.
Discussion
Several reports in the literature have demonstrated the benefits of treating immature permanent teeth with pulp necrosis and incomplete apexes using endodontic revascularization, thus establishing the efficacy and safety of this important regenerative technique. Typical benefits reported include pain-free postoperative results, positive vitality signs, absence of edema or fistula, and resolution of chronic apical periodontitis as suggested by radiographic images.11,12
Mechanical instrumentation is a critically important step in the success of any endodontic treatment. The correct instrumentation allows for a significant decrease in bacterial load while providing a root canal shape that enables obturation techniques to be followed. In the endodontic revascularization technique, this cornerstone step could not be performed because of the increased susceptibility of root fracture (trans- or postoperative) that immature teeth with incomplete root formation display.6,13-15 Due to this important clinical limitation, disinfection is based completely on the use of antibacterial solutions as per the protocol published by Petrino et al.12 Such irrigation protocol includes the use of NaOCl (5.25%), saline solution, and chlorhexidine (0.12%). Saline solution used between irrigation with antibacterial agents is needed to avoid the formation of complexes between NaOCl and chlorhexidine.16
Hoshino et al proposed the use of an intracanal antibiotic paste composed of three broad-spectrum antibiotics (ciprofloxacin, metronidazole, and minocycline) that must be kept sealed in the canal for at least 3 weeks.17 Other studies that investigated the antibacterial efficacy of such a method have demonstrated that this approach is safe and effective to promote the eradication of endodontic pathogens from infected root canals in both in vitro and in vivo studies.18,19
While investigating the antibacterial efficacy of minocycline against known endodontic pathogens, Ritter et al in a clinical study reported a strong cervical discoloration that was associated with the formation of coronal dark spots after use of such antibiotic paste for 2 weeks.20 The authors also reported a strong antibacterial behavior that facilitated revascularization of re-implanted teeth with incomplete root formation. In the study, the patient reported light sensitivity while being tested for vitality using traditional endodontic methods.
The discoloration findings reported in the present study are in agreement with previous publications that have shown that tooth discoloration is the major complaint from patients after being treated with endodontic revascularization techniques.12 Khademi et al while investigating the impact of the use of antibiotic pastes or MTA on tooth discoloration severity, showed that both experimental groups promoted significant discoloration levels when compared to the control group (no intervention), thereby demonstrating that MTA alone is capable of promoting strong tooth discoloration.19
In the present case report, some changes to the traditional endodontic revascularization technique were implemented in order to assess the utility of Emdogain gel as a structural matrix (scaffold). According to Lyngstadaas et al, Emdogain has been demonstrated to be safe and effective in periodontal treatments and has regenerative potential for application in other clinical areas of dentistry such as endodontics, implantology, and traumatology.8 Min et al also suggested that these important properties could be further explored in pulp and dentin regeneration approaches.21
According to Chen et al,22 and despite the fact that tissue growth (both in length and thickness) was not observed in the present study, this case could be classified as a type 2. Based on the findings reported herein, it is possible to affirm that the results attained were clinically favorable. Such a statement is based on the periapical response to the treatment, where no signs of tissue abnormality were observed during the 72-month follow-up period, and the positive response during vitality tests.
In this regard, the present study has demonstrated the observation of positive vitality results that might suggest the neo-formation of pulp tissues with no root canal obliteration in the long term. Because only imaging techniques were conducted in the present study, further molecular and histological characterizations are necessary to truly describe the types and origins of tissues neo-formed in the canal. Long-term longitudinal clinical trials are also necessary to determine the clinical success of endodontic revascularization techniques and to provide the field with important information extending over 48 to 60 months of follow-up.23,24
Conclusion
The present case report represents a 72-month follow-up that successfully demonstrated the utility of an amended endodontic revascularization protocol capable of promoting the neo-formation of tissues in the canal without the presence of adverse symptoms (eg, edema, fistula, or pain). The major limitation of the present study is related to tooth discoloration.
ACKNOWLEDGMENT
The authors acknowledge that no conflicts of interest have influenced the outcomes, findings, or conclusions of the present case report.
ABOUT THE AUTHORS
Neidy S. Corredor Gerber, DDS
Dentistry Graduate Program, Positivo University, Curitiba, Brazil
Beatriz S. Coelho, MS
Dentistry Graduate Program, Positivo University, Curitiba, Brazil
Tatiana M. Deliberador, PhD
Dentistry Graduate Program, Positivo University, Curitiba, Brazil
Darlan R. Junior, DDS
Dentistry Graduate Program, Positivo University, Curitiba, Brazil
Flares Baratto-Filho, PhD
Dentistry Graduate Program, Positivo University, Curitiba, Brazil
Fernando Luis Esteban Florez, PhD
Department of Restorative Sciences, Division of Dental Biomaterials, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma
João C. Zielak, PhD
Dentistry Graduate Program, Positivo University, Curitiba, Brazil
Denise P. Leonardi, PhD
Dentistry Graduate Program, Positivo University, Curitiba, Brazil
REFERENCES
1. Jeeruphan T, Jantarat J, Yanpiset K, et al. Mahidol study 1: comparison of radiographic and survival outcomes of immature teeth treated with either regenerative endodontic or apexification methods: a retrospective study. J Endod. 2012;38(10):1330-1336.
2. Trope M. Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dent Clin North Am. 2010;54(2):313-324.
3. Rafter M. Apexification: a review. Dent Traumatol. 2005;21(1):1-8.
4. Cvek M. Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha. A retrospective clinical study. Endod Dent Traumatol. 1992;8(2):45-55.
5. Huang GT. Apexification: the beginning of its end. Int Endod J. 2009;42(10):855-866.
6. Shin SY, Albert JS, Mortman RE. One step pulp revascularization treatment of an immature permanent tooth with chronic apical abscess: a case report. Int Endod J. 2009;42(12):1118-1126.
7. Qu Z, Laky M, Ulm C, et al. Effect of Emdogain on proliferation and migration of different periodontal tissue-associated cells. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(6):924-931.
8. Lyngstadaas SP, Wohlfahrt JC, Brookes SJ, et al. Enamel matrix proteins; old molecules for new applications. Ortho Craniofac Res. 2009;12(3):243-253.
9. Banchs F, Trope M. Revascularization of immature permanent teeth with apical periodontitis: new treatment protocol? J Endod. 2004;30(4):196-200.
10. Khoshkhounejad M, Shokouhinejad N, Pirmoazen S. Regenerative endodontic treatment: report of two cases with different clinical management and outcomes. J Dent (Tehran). 2015;12(6):460-468.
11. Antunes LS, Salles AG, Gomes CC, et al. The effectiveness of pulp revascularization in root formation of necrotic immature permanent teeth: a systematic review. Acta Odontol Scand. 2016;74(3):161-169.
12. Petrino JA, Boda KK, Shambarger S, et al. Challenges in regenerative endodontics: a case series. J Endod. 2010;36(3):536-541.
13. Cotti E, Mereu M, Lusso D. Regenerative treatment of an immature, traumatized tooth with apical periodontitis: report of a case. J Endod. 2008;34(5):611-616.
14. da Silva LA, Nelson-Filho P, da Silva RA, et al. Revascularization and periapical repair after endodontic treatment using apical negative pressure irrigation versus conventional irrigation plus triantibiotic intracanal dressing in dogs' teeth with apical periodontitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(5):779-787.
15. Trope M. Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dent Clin North Am. 2010;54(2):313-324.
16. Bui TB, Baumgartner JC, Mitchell JC. Evaluation of the interaction between sodium hypochlorite and chlorhexidine gluconate and its effect on root dentin. J Endod. 2008;34(2):181-185.
17. Hoshino E, Kurihara-Ando N, Sato I, et al. In-vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprofloxacin, metronidazole and minocycline. Int Endod J. 1996;29(2):125-130.
18. Ding RY, Cheung GS, Chen J, et al. Pulp revascularization of immature teeth with apical periodontitis: a clinical study. J Endod. 2009;35(5):745-749.
19. Khademi AA, Dianat O, Mahjour F, et al. Outcomes of revascularization treatment in immature dog's teeth. Dent Traumatol. 2014;30(5):374-379.
20. Ritter AL, Ritter AV, Murrah V, et al. Pulp revascularization of replanted immature dog teeth after treatment with minocycline and doxycycline assessed by laser Doppler flowmetry, radiography, and histology. Dent Traumatol. 2004;20(2):75-84.
21. Min KS, Yang SH, Kim EC. The combined effect of mineral trioxide aggregate and enamel matrix derivative on odontoblastic differentiation in human dental pulp cells. J Endod. 2009;35(6):847-851.
22. Chen MY, Chen KL, Chen CA, et al. Responses of immature permanent teeth with infected necrotic pulp tissue and apical periodontitis/abscess to revascularization procedures. Int Endod J. 2012;45(3):294-305.
23. Jung IY, Lee SJ, Hargreaves KM. Biologically based treatment of immature permanent teeth with pulpal necrosis: a case series. J Endod. 2008;34(7):876-887.
24. Kim DS, Park H, Yeom JH, et al. Long-term follow-ups of revascularized immature necrotic teeth: three case reports. Int J Oral Sci. 2012;4(2):109-113.
FIGURE CAPTIONS
Fig 1. Periapical radiographic analysis: Initial condition of the patient, denoting incomplete root formation and diffuse radiolucent region.
Fig 2. Three weeks after root canal irrigation treatment, denoting decrease in radiolucent region and neo-formation of hard tissues along the apex of tooth No. 7.
Fig 3. Three months postoperative, denoting stronger bone formation on periapical regions and maintenance of canal dimensions (thickness and height).
Fig 4. Follow-up radiography at 72 months, denoting obliteration of tooth apex and maturation of bone tissues in the periapical regions.
Fig 5. CBCT panoramic view after 72 months, denoting bone densities that are comparable to non-affected regions.
Fig 6. Axial slice of treated teeth after 72 months, denoting clear obliteration of the canal.
Fig 7. Clinical aspect 72 months after treatment, denoting strong discoloration of cervical gingival tissue.
Fig 8. Clinical aspect 3 months after periodontal surgery, which was performed to resolve the gingival discoloration issue (patient's major concern at 72 months).